East Asian Arch Psychiatry 2024;34:147-9 | https://doi.org/10.12809/eaap2442
Case Report

Hoi Ying Choi, Department of Psychiatry, Kwai Chung Hospital, Hong Kong SAR, China
Men Ming Bonnie Chiu, Department of Psychiatry, Kwai Chung Hospital, Hong Kong SAR, China
Yung Kong Wong, Department of Radiology, Tuen Mun Hospital, Hong Kong SAR, China
Wai Tat Chan, Department of Radiology, Tuen Mun Hospital, Hong Kong SAR, China
Address for correspondence: Dr Hoi Ying Choi, Kwai Chung Hospital, New Territories, Hong Kong SAR, China. Email: choihy@ha.org.hk
Submitted: 25 August 2024; Accepted: 24 October 2024
Osmotic demyelination syndrome (ODS) is a demyelinating disorder caused by disturbances in the osmotic environment of the central nervous system. This condition can manifest both as central pontine myelinolysis (CPM), affecting the central pons, and extrapontine myelinolysis (EPM). Patients with CPM typically present with upper motor neuron signs such as locked-in syndrome and coma, whereas patients with EPM are characterised by movement disorders including parkinsonism, mutism, and dystonia, with catatonia being less common.1
Catatonia comprises various motor phenomena (eg, stupor, waxy flexibility, stereotypies), affective signs (eg, flat affect, affect incontinence, impulsivity), and cognitive-behavioural disturbances (eg, mutism, echolalia, echopraxia).2 Catatonia has been documented as a presenting symptom of ODS in a middle-aged man with depression following rapid correction of hyponatraemia.3 Here, we report a case of catatonia as a presenting symptom of ODS in a patient with schizophrenia. The importance of investigating potential ODS in patients with schizophrenia presenting with catatonia is highlighted.
Case presentation
In February 2023, a 51-year-old Chinese man with a 30-year history of schizophrenia was admitted to Kwai Chung Hospital with catatonia. He had experienced multiple psychotic relapses characterised by delusions and hallucinations but had never exhibited symptoms of catatonia before this admission. Notably, he had been free from psychotic symptoms for over a decade; however, he had displayed excessive water-drinking behaviour for 1 year before the onset of catatonia.
The catatonia was characterised by mutism and a loss of spontaneous volitional movements, except for visual pursuit. Neurological examination revealed no ophthalmoplegia or ataxia. The patient also presented with hypothermia (core temperature, 35.5°C) and hypotension (blood pressure, 87/49 mmHg).
Laboratory tests showed unremarkable complete blood counts, liver function, thyroid function, and serum electrolytes, except for a low serum sodium level of 117 mmol/L (normal range, 136-145 mmol/L) and a low vitamin B12 level of 24 pg/mL (normal range, 160-950 pg/mL). A urine drug screen result was negative.
The patient was transferred to the general medical unit for further management. Vitamin B12 replacement therapy was initiated, leading to gradual normalisation of serum vitamin B12 level. An infusion of 0.9% saline at a rate of 150 mL/hour was administered for 12 hours according to hospital guidelines. His serum sodium level increased rapidly to 128 mmol/L. Shortly thereafter, he developed acute tetraparesis, hyperreflexia, and increased muscle tone while maintaining preserved eye movements — all consistent with locked-in syndrome. Although the locked-in syndrome resolved spontaneously, the catatonia persisted.
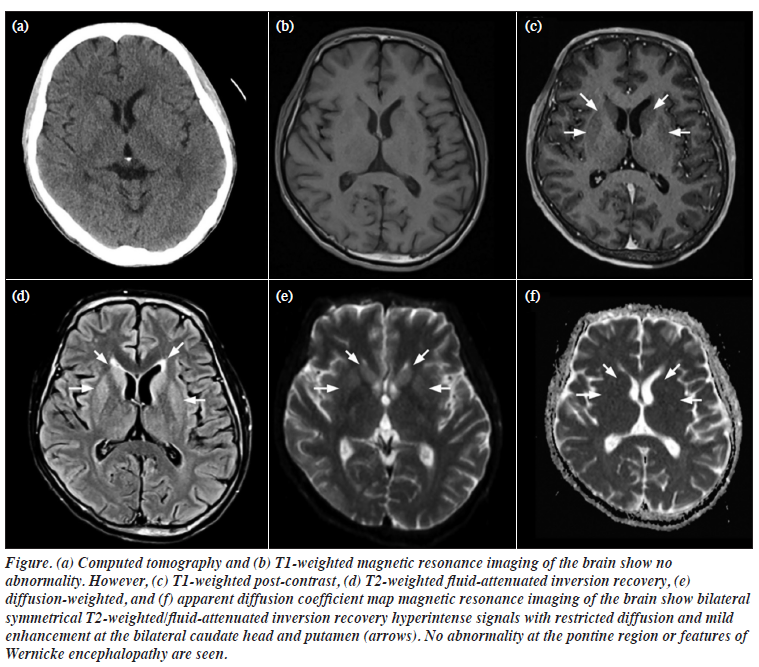
Computed tomography of the brain showed normal parenchymal attenuation without structural lesions. However, subsequent magnetic resonance imaging of the brain demonstrated symmetrical T2-weighted/fluid- attenuated inversion recovery hyperintense signals with restricted diffusion and mild enhancement without increased mass effect at the bilateral basal ganglia, suggestive of recent extrapontine demyelination (Figure). No abnormalities were detected in the pontine region, thalamus, or mammillary bodies that indicates Wernicke encephalopathy.
The patient was already taking quetiapine for his schizophrenia, and the dosage was increased from 250 mg to 300 mg in the evening. Physiotherapy and occupational therapy were also initiated. Over the following month, his catatonia gradually resolved, and he was discharged.
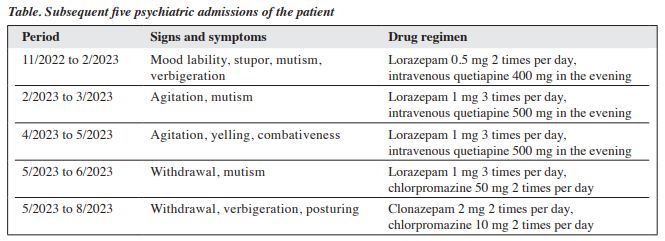
In the subsequent year, the patient was hospitalised five times for relapses of catatonia despite adherence to psychiatric medications (Table). Each time, the presentation was similar — stupor alternating with irritability, mutism, rigidity, staring spells, and catalepsy, but without delusions or hallucinations. Complete remission occurred between episodes. All episodes were preceded by excessive water- drinking behaviour, which was correlated with low serum sodium levels ranging from 127 to 132 mmol/L. Blood and urine test results were unremarkable. His catatonia resolved spontaneously in each episode upon normalisation of serum sodium levels after fluid restriction (1-1.5 litres per day). Throughout this period, he received maintenance treatment with a combination of antipsychotics and benzodiazepines without extensive changes to his medication regimen.
Discussion
This case illustrates both forms of ODS in a patient with schizophrenia: EPM presenting as catatonia triggered by hyponatraemia related to psychogenic polydipsia and CPM manifesting as locked-in syndrome following rapid correction of severe hyponatraemia.
The diagnosis of ODS primarily relies on an accurate medical history that identifies preceding triggers or potential causative factors alongside common symptoms associated with CPM/EPM. Initially linked to alcoholism and malnutrition, ODS is now considered to be associated with rapid sodium correction in patients with hyponatraemia. However, ODS is also correlated with alcoholism, malnutrition, psychogenic polydipsia, post-liver transplant status, and post-surgical states involving glycine infusion.1
In our patient, blood tests were instrumental in ruling out potential aetiological factors. For instance, renal function tests indicated hyponatraemia likely stemming from psychogenic polydipsia, whereas low vitamin B12 levels suggested malnutrition. Neuroimaging plays a supportive role in diagnosis; computed tomography is useful for excluding gross intracranial space-occupying lesions or infarcts, whereas magnetic resonance imaging can detect demyelination signal abnormalities and classify ODS into CPM or EPM based on the location.
Historically regarded as a subtype of schizophrenia, catatonia is now classified as an independent entity by the ICD-11.4 Our case underscores the necessity of considering medical aetiologies, rather than solely psychiatric conditions, in patients with schizophrenia who present with catatonia. Patients with schizophrenia may be particularly susceptible to aetiological factors associated with ODS; for example, our patient had experienced psychogenic polydipsia and malnutrition. Targeted management strategies should be based on causative factors for ODS including controlled fluid restriction during sodium replenishment for hyponatraemia and vitamin B12 replenishment for deficiency.
Interestingly, our patient developed CPM following rapid correction of severe hyponatraemia while exhibiting EPM in the form of catatonia during repeated episodes of mild hyponatraemia linked to psychogenic polydipsia. We therefore hypothesise that different triggers may be associated with distinct forms of ODS due to varying extents of osmotic disturbance within the central nervous system; further research is warranted to explore this hypothesis.
Contributors
All authors designed the study, acquired the data, analysed the data, drafted the manuscript, and critically revised the manuscript for important intellectual content. All authors had full access to the data, contributed to the study, approved the final version for publication, and take responsibility for its accuracy and integrity.
HYC designed the study, acquired the data, analysed the data, drafted the manuscript, and critically revised the manuscript for important intellectual content. MMC, YKW, and WTC critically revised the manuscript for important intellectual content.
Conflicts of interest
All authors have disclosed no conflicts of interest.
Funding / support
This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Data availability
All data generated or analysed during the present study are available from the corresponding author on reasonable request.
Ethics approval
This study was approved by Central Institutional Review
Board of the Hospital Authority (reference: CIRB-2024- 146-2). The patient provided written informed consent for all treatments and procedures and for publication.
References
- Martin RJ. Central pontine and extrapontine myelinolysis: the osmotic demyelination syndromes. J Neurol Neurosurg Psychiatry 2004;75(Suppl 3):iii22-28.
- Hirjak D, Foucher JR, Ams M, et al. The origins of catatonia: systematic review of historical texts between 1800 and 1900. Schizophr Res 2024;263:6-17.
- Mattoo SK, Biswas P, Sahoo M, Grover S. Catatonic syndrome in central pontine/extrapontine myelinolysis: a case report. Prog Neuropsychopharmacol Biol Psychiatry 2008;32:1344-6.
- Heckers S, Walther S. Catatonia. N Engl J Med 2023;389:1797-802.


