Hong Kong J Psychiatry 2002;12(3):5-11
ORIGINAL ARTICLE
G Singh, P Sharan, P Kulhara
Dr G Singh, MD, Senior Resident, Department of Psychiatry, Postgraduate Institute of Medical Education and Research, Chandigarh, India
Dr P Sharan, MD, Associate Professor, Department of Psychiatry, Postgraduate Institute of Medical Education and Research, Chandigarh, India
Dr P Kulhara, MD, FRCPsych, Professor, Department of Psychiatry, Postgraduate Institute of Medical Education and Research, Chandigarh, India
Address for correspondence: Dr P Sharan, Associate Professor, Department of Psychiatry, Postgraduate Institute of Medical Education and Research, Chandigarh-160012, India
Tel: (91 172) 747 585-602, ext. 247
Fax: (91 172) 744 401
E-mail: medinst@pgi.chd.nic.in
Submitted: 21 December 2001; Accepted: 30 May 2002
Abstract
Objective: To examine socio-demographic and clinical correlates of coping strategies employed by patients with chronic schizophrenia to manage hallucinations.
Patients and Methods: Seventy five patients with chronic stable schizophrenia with hallucinations (in any form) were enrolled. Data on socio-demographic and clinical variables were recorded. The following scales were utilised: Phenomenology of Hallucinations, Attitude towards Hallucinations, and Instrument for Assessment of Coping Behaviour.
Results: On average, each patient used 4 coping strategies to deal with hallucinations. ‘Help seeking’ coping strategies were most commonly employed. Unmarried patients employed a greater number of coping strategies than married patients and used more ‘avoidance’ strategies. Patients from an urban background used more ‘diversion’ and ‘help seeking’ coping strategies. Age correlated negatively with the total number of coping strategies and specifically with ‘helpseeking’, ‘problem solving’, and ‘diversion’ strategies. Duration of illness also correlated negatively with ‘help-seeking’ coping strategies.
Conclusions: Indian patients with schizophrenia used numerous coping strategies to deal with hallucinations. There were few significant correlations between coping strategies and sociodemographic or clinical variables.
Keywords: Coping, Hallucinations, Schizophrenia
Introduction
Coping is an action directed at resolution or mitigation of a problematic situation.1 Lazarus and Folkman defined coping as the “person’s cognitive and behavioural efforts to manage internal and external demands on the person, which are appraised as taxing or exceeding the person’s resources.”2 Ostell also provided a ‘stress-coping’ paradigm to explain human reaction to a stressful situation.3
According to Hatfield,4 an account of patients’ efforts at coping with symptoms of schizophrenia can be found in the descriptive literature of Bleuler and Freud. Auto- biographical accounts by patients with schizophrenia also provide glimpses of coping methods employed to handle distressing symptoms.5 Since psychotic symptoms are a major source of stress in schizophrenia, most research has focussed on this area. Coping strategies for dealing with hallucinations in schizophrenia have been studied along with other symptoms5-8 and also individually.9-10,11-15 It is now generally accepted that patients employ more coping strategies for dealing with hallucinations than for any other psychotic symptom.6
Approximately 60% to 90% of patients with schizophre- nia who hallucinate can specify the use of distinct coping strategies.11,13,15,16 The mean number of coping strategies used varies from 1 to 13.4 in different studies, with the difference probably being due to differences in assessment methods used to elicit coping responses.13,15
Studies consistently show that patients most frequently use cognitive methods of suppression and shifting attention. Behavioural methods such as distraction (active and passive) are also frequently used.5,7,9,10,12,13,15 Increased socialisation (which involves initiating contact), change of activity (passivity), and seeking medical help were other commonly used coping strategies.5,7,14,16-19 Physiological methods such as relaxation, use of prescribed/non-prescribed drugs and others were less commonly employed.5,10,11,13,15,16
Farhall and Gehrbe reported that patients with schizo- phrenia who hallucinate most frequently used the problem- solving method of ‘taking action’ as a general strategy.12
Interacting with voices was identified as the most common hallucination-specific strategy. Strategies of ‘talking back/shout- ing at voices’ were also employed by some patients.9,11,15
A significant proportion of patients used active acceptance as a coping mechanism, for example “listening to what they say and accept.”13 Similar strategies were reported by Romme et al using the term ‘selective listening’.12 Specified social activities, task performance, and subvocalisation (for example humming) were infrequently employed.7,11,15 Patients also reported the use of strategies such as the use of ear plugs and loud music to drown the intensity of the hallucinations.1,15
Attempts have been made to group coping strategies. Falloon and Talbot were amongst the first to study coping in relation to hallucinations and divided coping strategies into 3 main categories:9
- behavioural change (e.g. activities, taking drugs)
- changes in physiological arousal — either a reduction (e.g. relaxation) or increase (e.g. stimulating music)
- cognitive strategies (e.g. suppression, acceptance).
Ramanathan identified 6 coping themes.10 These were rejection, control, resignation, minimisation, avoidance, and dependency. ‘Rejection’ was defined as disparagement of oneself, castigation of those ’responsible’, and bitterness against those who cannot empathise with one’s fate. ‘Control’ meant deliberate involvement in activities such as work and social life and taking preventive action to ward off recurrence. ‘Resignation’ indicated cultivation of philosophical stoicism so that one yields to the possibility of recurrence of illness. ‘Minimisation’ involved dismissal of the possibility of recurrence and its implications by the use of denial and rationalisation. In ‘avoidance’, one was presumed to indulge in self-distraction by reading or talking and to reject op- portunities for information about possible consequences. ‘Dependency’ meant complete reliance upon the judgement of external resources (the individual sees him/herself as powerless). These themes were arranged in 2 dimensions: control-helplessness and acknowledgement of threat- disavowal of threat.10
Empirical grouping has been suggested following multi- variate statistical methods. Carter et al elicited a variety of coping reactions using the Mental Health Institute Unusual Perception Schedule (MUPS)20 in their group of 100 hallucinating patients.11 The authors created 4 clusters of coping reactions using cluster analysis:
- cluster I consisted of strategies such as reading aloud, playing games, writing, humming, subvocalisation, and using ear plugs
- cluster II consisted of coping strategies of listening to music or the radio
- cluster III included relaxation and talking to someone about voices
- cluster IV consisted of withdrawal/avoidance responses such as yelling back or using drugs.
Studies of correlates of coping behaviour have shown that males and females use an equal number of coping strategies. Regarding specific strategies, males tend to use socialisation and talking about voices more than females, who were reported to use prescribed drugs more often.9 No differences in coping patterns were observed across subgroups divided according to educational attainment.11,21
Wahass and Kent reported cross-cultural differences in coping strategies for dealing with hallucinations in western (British) and non-western (Saudi Arabian) patients.15 Saudi Arabian patients often coped through the use of religious activities, while British patients used distraction and physiological methods (such as relaxation) more often.15 Blacks are reported to use relaxation and posturing more than Caucasians, who use drugs more often.9
No significant differences in the number or type of coping strategies have been reported in subgroups of schizophrenic patients stratified according to illness vari- ables (age of onset, subtypes of schizophrenia, comorbid depression, use of neuroleptic agents alone or in combination with antiparkinsonian agents, drug dosages, and so on) or according to parameters of hallucination (frequency, duration).9,11
Patients with schizophrenia are reported to employ more coping strategies for voices with unpleasant content, to deal with the dimension of loudness and to stop the voices. More distressed patients employed a greater number of coping strategies.15 Carter et al found that patients who claimed that they would miss their voices (had positive attitudes) employed more coping strategies than those who said that they would not miss the voices.11
A review of studies of coping strategies used to deal with hallucinations revealed that the majority of patients studied belonged to heterogeneous groups of patients with psy- chosis. Moreover, in these studies, attention was not paid to the influence of important factors such as pharmacotherapy, duration of illness and so on. The present study aimed to examine the coping strategies used by patients with schizophrenia and to evaluate their correlates.
Patients and Methods
The study group consisted of patients attending the Psychiatry Out-patient Department, Nehru Hospital, Post- graduate Institute of Medical Education and Research, Chandigarh, India. The inclusion criteria were a definite diagnosis of schizophrenia according to the International Classification of Diseases (ICD) -10 diagnostic guidelines, 22 for a duration of more than 2 years, stability of illness for at least 3 months prior to assessment (stability of illness was defined as clinical and functional stability as judged by the treating physician, reflected by the criterion of absence of exacerbation of illness requiring increase in drug dosages by ³50% — as mentioned by Gupta et al23), and presence of hallucinations (in any modality) in the past 3 months. Patients who were changing their antipsychotic medication were not included, since change of medication would suggest the absence of stability.
Patients with concomitant major chronic illness, organic brain disease, or substance abuse were excluded from the study. The exclusion of patients with schizophrenia with comorbid substance abuse could potentially bias the results. However, in the clinic at the Nehru Hospital, this comorbidity does not frequently occur (only 6% of patients with schizophrenia have an additional diagnosis of substance abuse).The presence of comorbidity would have affected the way that patients with schizophrenia cope with hallu- cinations in unknown ways.
After explaining the purpose and nature of the research, written informed consent was taken from the patient or an adult relative in case the patient was considered to be unfit for providing informed consent. Socio-demographic data was recorded, and the patient and a relative were interviewed to elicit information regarding the diagnosis, duration of illness, duration of drug treatment, mean daily dose of neuro- leptic agents in chlorpromazine equivalents during the past week, change of drug dosage in the past 3 months, modality of hallucinations, and family history of schizophrenia.
All patients were assessed using the Brief Psychiatric Rating Scale (BPRS),24 Phenomenology of Hallucinations,25 Patient’s Attitudes Towards Hallucinations,26 and Instrument for Assessment of Coping Behavior (IKB).27 Phenomenology of Hallucinations25 is a semi-structured interview consisting of 15 items, each of which is scored from 1 to 3. The scale measures various parameters of hallucinations, namely extent (frequency and duration), location, reality (current and past), sensory intensity, constancy, overt behaviour, control, time, ‘causal’, experience shared, content-affect, content-noun, and content-verb.
As a parameter of extent, ‘frequency’ measures the number of times that a hallucination occurs and ‘duration’ measures the period for which the hallucination lasted. ‘Location’ means assessing the source of the hallucination in objective space. ‘Reality’ assesses the ‘perceived veridicality’ of the experience. ‘Sensory intensity’ measures the ‘oblit- eration’ of patient’s ordinary perception in a given modality by the hallucination. ‘Constancy’ establishes the degree of change in the experience during its occurrence. ‘Overt behaviour’ is a measure of the actions that the patient takes in response to the experience of hallucination. ‘Control’ establishes the degree of perceived control of the patients over the occurrence of hallucinations and its effects. ‘Time’ assesses the change in patient’s sense of time during the occurrence of the hallucination.
The item ‘causal’ assesses the specificity of the attrib- uted cause of the hallucinations. ‘Experience shared’ assesses the patient’s belief about the degree to which other (real) people perceive what is being felt by him/her. ‘Content- affect’ (reaction) describes emotions produced in response to hallucinations. ‘Content-noun’ assesses the predominant item that is hallucinated, for example, person, object, or self. ‘Content-verb’ measures actions relating to the patient occurring within the hallucination.
A modified version of the scale was reported to have good inter-rater reliability.25 To obtain a Hindi translation, the standard protocol of (repeated) translation/back-translation was followed. This was supervised by a Consultant in Clin- ical Psychology who had considerable experience of scale construction.
The original scale does not yield a total score. However, for the purpose of the present study, the scale was administered as recommended, but a total score signifying the overall severity of the hallucination was calculated, based on a restricted set of items (9 items), which correlated to a significant extent with the raw total (15 items) on item- total analysis. The items that contributed to the severity of hallucination score were frequency, duration, location, reality (current and past), sensory intensity, overt behaviour, ‘causal’, and content-verb.
Patient’s Attitudes towards Hallucinations is an 11-item scale.26 Each item is rated as follows: 0 ‘not positive or only negative’, 1 ‘both positive and negative’, or 2 ‘positive only’. A total score can be obtained by adding up item scores. The scale was found to have good inter-rater reliability by the authors. The sample questions for the interview were translated into simple Hindi, back-translated into English and then retranslated into Hindi. Cronbach’s a to test the consistency of the scale yielded a value of 0.68.
The IKB is a structured interview that assesses coping strategies in response to various complaints.27 For each com- plaint, the degree of perceived stress is rated from 0 (no stress) to 4 (high stress). Patients are asked to indicate their usual coping strategies from a list of coping reactions. The instrument is reported to have good inter-rater reliability. As with the other instruments, the IKB was translated into Hindi, back-translated into English and then retranslated into Hindi. Factor solution used by Kumar et al6 was used for descriptive purposes. Each question on coping was asked in relation to hallucination as the stressor.
Statistical Analysis
Student’s ‘t’ test and ANOVA were used for group compari- son. Pearson’s product moment coefficient of correlations was computed to examine the relationship between coping strategies score with other variables.
Results
Nearly two-thirds of the patients were male and a similar proportion of patients had married at some point in their lives. Nearly 60% of patients belonged to the unemployed/ housewife, retired, or student category and had no income. Forty six percent of patients were educated above matricu- lation (10 years of education). The majority of the study population were Hindu. Fifty three percent of patients were part of nuclear families and the majority were from an urban locality.
Two-thirds of patients had paranoid schizophrenia. The average duration of illness was more than 10 years (mean, 128.73 months; SD, 90.31 months). The mean BPRS score at the time of the assessment was 44.66 (SD, 7.09). Patients had sought treatment approximately 28 months after the onset of illness and were receiving approximately 500 mg of neuroleptic agents in chlorpromazine equivalents per day (mean, 483.33 mg/day; SD 312.56 mg/day). The majority of patients had never been admitted to hospital during the course of their illness. Eighty percent had no family history of schizophrenia.
Most patients (76%) were currently hallucinating (last hallucination on the day of assessment). Auditory hallu- cinations alone were reported by 84% of patients. Auditory and visual hallucinations were reported by 11% of patients.
Thirteen percent of the patients reported that they did not employ any coping strategies to deal with hallucina- tions. Five percent of patients used 1 coping strategy and 81% used more than 1 coping strategy. On average, each patient used 4 coping strategies to deal with hallucinations (mean, 3.87; SD, 2.36).
The distribution of coping strategies under the headings proposed by Kumar et al6 is shown in Table 1. ‘Help-seeking’ strategies were used most frequently (mean, 1.36; SD, 0.61). Consulting the doctor/taking medicines was the strategy favoured by most patients (69%). The second most com- monly used group of coping strategies was ‘diversion’ (mean, 1.20; SD, 0.66) — meditation or relaxation had been tried by 56% of patients. ‘Problem-solving’ coping strategies were less frequently employed by patients (mean, 0.97; SD, 0.48). ‘Self-encouragement’ was the most frequently used strategy in this category with 50% of patients reporting its use. The ‘avoidance’ category was the least frequently used (mean, 0.21; SD, 0.30).
Comparison of various sociodemographic subgroups with respect to the total number of coping strategies used found that the number of coping strategies used to manage hallucinations did not differ amongst subgroups defined by gender (male: mean, 4.00; SD, 2.41; female: mean, 3.62; SD, 2.28; t = 0.66), occupation (F = 0.46), income (F = 0.05), educational status (F = 2.55), religion (Hindu: mean, 3.58; SD, 2.26; other: mean, 4.44; SD, 2.48; t = 1.49), family type (nuclear: mean, 3.85; SD, 2.35; other: mean, 3.89; SD, 2.39; t = 0.06). However, patients who had never married were found to be using a significantly greater number of coping strategies (mean, 4.67; SD, 2.52) than those who had married at some point (mean, 3.42; SD, 2.32; t = 2.261; p < 0.05).
Comparison of patients grouped according to various clinical characteristics revealed that the total number of coping strategies used to deal with hallucinations did not differ in subgroups defined by diagnosis, dose change (dose change 0% to 25%: mean, 3.92; SD, 2.35; dose change 25% to 50%: mean, 3.67; SD, 2.46; t = 0.36), number of admis- sions to hospital (no admissions: mean, 3.62; SD, 2.19; 1 or more admissions: mean, 4.55; SD, 1.52), family history of schizophrenia (positive: mean, 2.13; SD, 0.91; negative: mean, 2.48; SD, 0.83; t = 1.42), time of last reported hallu- cination (F = 1.60), type of hallucination (auditory: mean, 3.73; SD, 2.30; other: mean, 4.58; SD, 2.60; t = 1.15).
When patients within different socio-demographic sub- groups were compared with respect to coping strategies grouped according to factors derived by Kumar et al,6 it was observed that patients who had never married in their lives used more ‘avoidance’ coping strategies (mean, 0.41; SD, 0.57) compared with patients who had married at some point (mean, 0.10; SD, 0.30; t = 2.9; p < 0.01). Patients from an urban background had significantly higher scores for ‘problem solving’ coping strategies (mean, 1.46; SD, 0.41) compared with patients from a rural background (mean, 0.70; SD, 0.61; t = 3.00; p < 0.01). Patients from urban back- grounds also used significantly more ‘diversion’ coping strategies (mean, 1.81; SD, 0.91) compared with their rural counterparts (mean, 0.91; SD, 0.71; t = 2.4; p < 0.05). They also used more ‘help seeking’ coping strategies (mean, 1.50; SD, 0.29) than patients from rural backgrounds (mean, 0.66; SD, 0.68, t = 3.15, p < 0.01). Similarly, comparison of subgroups with different clinical characteristics found that patients with auditory hallucinations alone (mean, 1.11; SD, 0.84) used significantly more ‘diversion’ coping strategies than patients with hallucinations of other types (mean, 1.67; SD, 0.97; t = 2.03; p < 0.05).
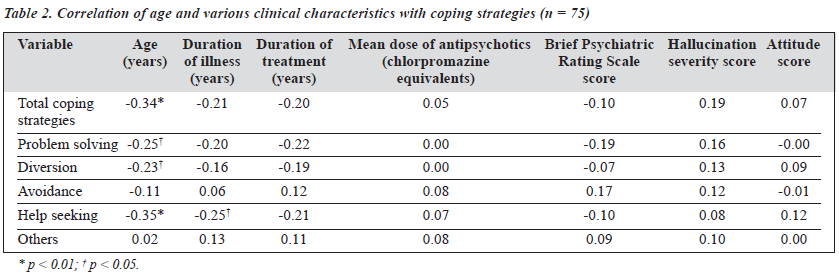
Table 2 shows the correlation between age and various clinical parameters with coping strategies. The total coping strategies score had a significant negative correlation with age (r = -0.34; p < 0.01).
Age also had a significant negative correlation with ‘help seeking’ (r = -0.35; p < 0.01), ‘problem solving’ (r = 0.025; p < 0.05), and ‘diversion’ scores (r = -0.23; p < 0.05). Duration of illness correlated negatively with ‘help seeking’ coping strategies (r = -0.25; p < 0.05). Coping strategies grouped according to the factor analytic model of Kumar et al6 did not correlate significantly with BPRS scores, hallucination severity score, and attitude score.
Discussion
Approximately 80% of patients used 1 or more coping strate- gies. Other researchers have also reported similar figures (60% to 94%).11,13,14,21 Patients reported using an average of 4 coping strategies each. Wahass and Kent, while assessing the coping strategies of patients with schizophrenia in different phases of the illness, also reported comparable figures (mean, 2.38 strategies).15 The mean number of coping strategies used was less than the number reported by Farhall and Gehrbe (13.4).13 The difference may be explained by the fact that no active prompting to elicit more coping strategies was used in the present study, as against the latter study. Also, Farhall and Gehrbe used a different instrument.13
In the present study, the majority of patients reported using the coping strategy of ‘going to the doctor/taking medicine’ (69.3%). Others have also reported that 40% to 50% of patients seek medical help.5,7,17 Kumar et al had stated that this was the commonest strategy employed by Indian patients to manage schizophrenic symptoms in general (including hallucinations). 6 Kumar et al also noted that this finding might reflect a cross-cultural difference in that Indian patients might seek help, while a Caucasian patient might try to deal with the problem on his/her own.6
Patients used coping strategies of ‘thinking about chang- ing the problem’ and ‘actively changing the situation’ less frequently than seeking medical help (28% and 9%, respect- ively). Other authors have also reported that only 10% to 15% of patients used coping strategies which involved their own active effort.7,11,15
Many patients have been reported to use non-prescribed addictive drugs (15% to 25%).5,10,11,13,15,16 In the present study, the exclusion criteria for substance abuse could have led to exclusion of subjects who used such substances to cope with hallucinations. However, the rate of such comorbidity was low in the present sample (6%).
‘Help seeking’ coping strategies and ‘diversion’ tactics were reported to be used relatively frequently in the present sample, while ‘problem-solving’ were not frequently used. ‘Avoidance’ coping strategies were used least frequently. In another Indian sample, Kumar et al had found that patients with schizophrenia in partial or total remission used coping strategies belonging to the following subgroups: ‘problem solving’, ‘avoidance’, ‘diversion’, and ‘help seeking’ in decreasing order of frequency.6 On the other hand, German patients used coping strategies belonging to the following subgroups: ‘problem solving’, ‘diversion’, ‘help seeking’, and ‘avoidance’ in decreasing order of frequency. In Kumar et al’s study, coping strategies for all psychotic symptoms and subjective complaints were assessed6 as opposed to the focus in this study of coping strategies to manage hallu- cinations. This fact may explain the differences in findings between the 2 studies. Greater reporting of use of ‘help seek- ing’ coping strategies may also have occurred because the patients were selected from those attending the outpatient clinic (rather than patients in the community). However, this interpretation should be moderated by the fact that vast majority of patients in our study are brought to the clinic by family members (rather than coming on their own).
The frequency of use of ‘problem solving’ coping strat- egies in the present study was actually greater than that in earlier studies that have focussed on hallucinations (approximately 15%).7,11,15 This may be explained by the fact that the current sample included only patients with stable disease. Patients who were acutely/severely ill have been reported to use fewer ‘problem solving’ coping strategies.28,29
In our study, socio-demographic variables such as sex, educational status, income group, family type, and religion had no association with the number of coping strategies and specific coping strategies used. Similar findings have been reported by others.9,10,11,21 Older patients were found to use fewer coping strategies, although others have reported no such association with age.9,11
Patients also used fewer ‘help seeking’, ‘problem solving’, and ‘diversion’ coping strategies. This could be due to lesser overall use of coping strategies, rather than less use of specific subgroups of coping strategies. Some of the findings noted by Carter et al, (less use of listening to music, loud sounds, and singing songs)11 were similar to those noted in the present study.
In the present study, male and female patients did not differ significantly regarding the number of coping strat- egies or specific subgroups of coping strategies used. Falloon and Talbot had noted that males used less socialisation and females used more prescribed drugs as ways of dealing with hallucinations.9 The difference in findings between their study and this one could be due to the fact that Falloon and Talbot focussed on individual coping strategies, while this study analysed data pertaining only to groups of coping strategies.
Other researchers have reported that patients of different marital status did not differ with respect to the total number of coping strategies used. 9,11,21 However, in the present study, patients who had never married (single) were noted to use more coping strategies compared with patients who had married at some point in their lives. Single patients were found to use ‘avoidance’ coping strategies more often compared with married patients. This may be explained by the smaller opportunity for married patients to avoid interaction and consequently other active methods of coping.
Contrary to observations by others,9-10,11,21 the present study suggests that patients who come from urban localities used a greater number of coping strategies than those from rural areas. They also used more ‘problem solving’, ‘help seeking’, and ‘diversion’ coping strategies than patients from a rural background. The reason for this is not clear. It may be that urban patients may be more able to verbalise alter- native coping strategies, while rural patients might be content to mention only a few strategies. Greater use of ‘problem solving’, ‘help seeking’, and ‘diversion’ among urban patients appears to be a reflection of the generally higher number of coping strategies used.
As noted by others,9,11 the total number of coping strat- egies used by patients was not associated with duration of illness and duration of treatment. However, patients with a greater duration of illness were found to be using a smaller number of ‘help seeking’ coping strategies. This may suggest that patients begin to accept their hallucinations or give up their efforts to cope, realising the futility of their efforts.
Other clinical characteristics — diagnostic subgroups, mean dose of neuroleptic agents, number of admissions to hospital, change of drug dosage, family history of schizophrenia, and time of last reported hallucinations were not associated with the number of coping strategies or specific groups of coping strategies used. Other researchers have obtained similar results with respect to diagnostic sub- groups.9,11 Lack of association between coping strategies and these variables suggests that coping efforts are determined by the individual’s personality and coping resources rather than by illness characteristic.
In the present study, patients who had auditory hallu- cinations alone used fewer ‘diversion’ coping strategies compared with patients with hallucinations of other types or hallucinations of more than 1 type. The reasons for this are not immediately apparent. However, this finding needs to be replicated before any comment is made since no other study has focussed on this aspect.
Total psychopathology, hallucination severity, and attitude scores did not correlate with the total number of coping strategies used or specific subgroups. Again, this points towards the lack of influence of illness characteris- tics on coping efforts.
Carter et al, while assessing coping strategies in different diagnostic groups, had reported that those who held positive attitudes towards hallucinations (did not want to reject hallucinations as they claimed that they would miss them) used more coping strategies.11 In the present study, no such relationship was noted. Differences in methodology, sample characteristics or response format (forced choice vs open ended) could have been responsible for the discrepancy in the results between the 2 studies.
The study suggests that schizophrenic patients use many coping strategies to deal with hallucinations. This augers well for the use of coping skills training in psychosocial rehabilitation of patients with schizophrenia who continue to hallucinate despite adequate treatment. Such efforts may be particularly directed at older adults from a rural back- ground who have an illness of long duration (particularly if they are single) as this subset of patients is deficient in the use of coping resources. Further studies can explore the usefulness of various strategies to enable the development of a treatment package. Lack of any important correlation with socio-demographic or clinical variables suggests that future studies could target the personality or biological factors as possible correlates of coping behaviours.
This study has some important limitations. The IKB used for the present study does not make any inquiry into hallu- cination specific coping strategies. An approach similar to Farhall and Gehrbe13 may have been better. Secondly, the grouping of coping strategies used in the present study was based on a factor analytic solution that has not been validated for Indian patients. Thirdly, selection of out- patients with chronic and stable disease who are being treated at a tertiary care centre limits the generalisability of find- ings to the general schizophrenic population, particularly those who are acutely ill (‘help seeking’ may have emerged as the most frequent method because the sample consisted of outpatients rather than people in the community). How- ever, this exploratory study targeted such a group because it is this group of patients who may benefit most from psychosocial interventions of coping strategies and skills training.
References
- Ray C, Lindop J, Gibson S. The concept of coping. Psychol Med 1982;12:383-395.
- Lazarus RS, Folkman S. Stress, appraisal and coping. New York: Springer; 1984.
- Ostell A. The development of diagnostic framework of problem solving and stress. Counsl Psychol Quart 1988;1:189-209.
- Hatfield BA. Patient’s account of stress and coping in schizophrenia. Hosp Community Psychiatry 1989; 10:1141-1145.
- Carr V. Patients’ techniques for coping with schizophrenia: an explor- atory study. Br J Med Psychol 1988;61:339-352.
- Kumar S, Thara R, Rist F. Coping with symptoms of schizophrenia: a cross-cultural comparison. Indian J Soc Psych 1994;10:4-10.
- Raguram R. An exploratory study of coping styles in schizophrenic patients. Indian J Psychiatry 1993;35:22-26.
- Kumar S, Thara R, Rajkumar S. Coping with symptoms of relapse in schizophrenia. Eur Arch Psychiatr Neurol Sci 1989;239:213-215.
- Falloon IRH, Talbot RE. Persistent auditory hallucinations: coping mech- anisms and implications for management. Psychol Med 1981;11:329-339.
- Ramanathan A. A study of coping with auditory hallucinations in schizophrenics. Indian J Psychiatry 1984;26:229-236.
- Carter DM, Mackinnon A, Copolov DL. Patients’ strategies for coping with auditory hallucinations. J Nerv Ment Dis 1996;184:159-164.
- Romme MAJ, Honig A, Noorthoorn EO, Escher ADMAC. Coping with hearing voices: an emancipatory approach. Br J Psychiatry 1992;161: 99-103.
- Farhall J, Gehrbe M. Coping with hallucinations. Exploring stress and coping framework. Br J Clin Psychol 1997;36:259-261.
- Nayani TH, David AS. The auditory hallucinations: a phenomeno- logical survey. Psychol Med 1996;26:177-189.
- Wahass S, Kent G. Coping with auditory hallucinations: a cross culture comparison between Western (British) and non-Western (Saudi- Arabian) patients. J Nerv Ment Dis 1997;185:664-668.
- Brier A, Strauss JS. Self control in psychotic disorders. Arch Gen Psychiatry 1983;10:1111-1145.
- Lewinsohn PM. An empirical test of several popular notions about hallucinations in schizophrenic patients. In: Koup W, ed. Origin and mechanisms of hallucinations. New York: Plenum Press; 1970.
- Slade PD. The external control of auditory hallucinations. An informa- tion theory analysis. Br J Soc Clin Psychol 1974;13:249-258.
- Cohen CI, Berk LA. Personal coping styles of schizophrenic out- patients. Hosp Community Psychiatry 1985;36:407-410.
- Carter DM, Mackinnon A, Howard S, Zeegers T, Copolov DV. The development and reliability of the Mental Health Research Institute Unusual Perceptions Schedule (MUPS): An instrument to record auditory hallucinatory experience. Schizophr Res 1995;16:157-165.
- O’Sullivan K. Dimensions of coping with auditory hallucinations. J Ment Health 1994;3:251-256.
- World Health Organization. ICD-10. Classification of mental and behavioural disorders. Geneva: Oxford University Press; 1992.
- Gupta S, Kulhara P, Verma SK. Quality of Life in schizophrenia and dysthymia. Acta Psychiatr Scand 1998;97:290-296.
- Overall JE, Gorham DR. The Brief Psychiatric Rating Scale. Psychol Rep 1962;102:799-812.
- Lowe GR. The phenomenology of hallucinations as an aid to differen- tial diagnosis. Br J Psychiatry 1973;123:621-633.
- 26. Miller LJ, Eiloon O, Connor RN, Di Psaquaic T. Patient’s attitude towards hallucinations. Am J Psychiatry 1993;150:584-588.
- Thurm HM, Hafner H. Perceived vulnerability, relapse risk and coping in schizophrenia. Eur Arch Psychiatr Neurol Sci 1987;237:46-53.
- Takai A, Utomatsu M, Kaiya H, Inoue M, Ueiki H. Coping styles to basic disorders among schizophrenics. Acta Psychiatr Scand 1990;82:289-294.
- Weiki KH. Assessment of coping with schizophrenia: stressor, appraisal and coping behaviour. Br J Psychiatry 1992;161:114-122.