Hong Kong J Psychiatry 2000;10(4):4-6
ORIGINAL ARTICLE
PSYCHIATRIC ASPECTS OF HEADACHE: INITIAL EXPERIENCE FROM A NEWLY ESTABLISHED HEADACHE CLINIC
Dr CRJ Khess, MD, Associate Professor of Psychiatry, Central Institute of Psychiatry, Kanke, Ranchi - 834 006, India.
Dr R Kumar, DPM, Junior Resident, Central Institute of Psychiatry, Kanke, Ranchi - 834 006, India.
Dr S Basu, MB BS, Junior Resident, Central Institute of Psychiatry, Kanke, Ranchi - 834 006, India.
Dr S Akhtar, MD, DNB, Chief Medical Officer, Central Institute of Psychiatry, Kanke, Ranchi - 834 006, India.
Address for correspondence: Dr CRJ Khess
Associate Professor of Psychiatry Central Institute of Psychiatry Kanke
Ranchi - 834 006
India
ABSTRACT
Of 138 patients who sought consultation for headache in a newly established headache clinic, migraine was found to be the commonest diagnosis (36.20%) followed by depression (23.20%). Overall, there was an over-representation of females in the group, but a higher proportion of males among patients with depression. The males were generally younger than the females. The male sex-role stereotype is discussed as a possible reason for the over-representation of young males with depression. Emphasis is placed on the need to identify and effectively treat such patients who may never see a psychiatrist since they may not admit to their depression or seek treatment for the symptoms.
Key words: Depression; Headache; Help-seeking Behaviour; Migraine; Sex-role Stereotype
INTRODUCTION
In an interesting study, Packard surveyed 100 patients and 50 physicians to explore the expectations each held regarding headache treatment.1 Surprisingly, neither the patients nor the physicians listed psychological evaluation as important in the initial interview. However, there is now sufficient evidence to suggest a strong relationship between pain and psychiatric disorders.2-4 It has been reported that pain is located in the head rather than elsewhere in psychiatric patients. Some authors are of the opinion that psychological factors can serve as the sole basis for headache (e.g. conversion, hypochondri- asis, somatisation and somatoform pain disorders).5 Researchers such as Merskey2 and Large3 have reported a high incidence of neurosis and depression in patients referred from pain clinics. Depression and headache are particularly strongly associated — not only are chronic headache sufferers frequently depressed but headache is the most common somatic symptom of patients presenting for the treatment of depression, with an incidence rate of more than 50% in some studies.6,7 Our study was planned with these factors in mind. The aim of the study was to determine the frequency of psychiatric morbidity, especially depression, in patients attending a headache clinic.
MATERIAL AND METHODS
The study was conducted at the Central Institute of Psychiatry, which is a 643-bed postgraduate teaching institute. The insti- tute runs various special clinics such as the epilepsy clinic and the skin and venereal disease clinic. The headache clinic was established in August 1995 as an outpatient treatment facility. The clinic is held once a week. Patients who are registered at the headache clinic are examined by junior residents who record the history and physical findings in a case record file designed for the clinic. The findings are then discussed with the consultant and the final diagnosis is made. Whenever there is a possible psychiatric disorder present, a thorough mental status examination and diagnostic psychometry is done. The classification and diagnostic criteria for headache disorders, cranial neuralgias, and facial pain are used for the diagnoses of headache.8 For patients with a psychiatric disorder, the International Classification of Disease (ICD)-10 criteria is used.9
For this study, the case records of all patients attending the headache clinic during a 12-month period (from January 1997 to December 1997) was reviewed. The socio-demographic and clinical details, along with the diagnoses, were recorded on a specially designed form. The diagnoses were independently reviewed by at least two researchers and, only when there was a consensus, was a final diagnosis assigned. For patients with evidence of psychiatric problems, either from the history, mental status examination, or diagnostic psychometry, it was ensured that they fulfilled the ICD-10 criteria for a definite psy- chiatric disorder before being assigned a psychiatric diagnosis.
RESULTS
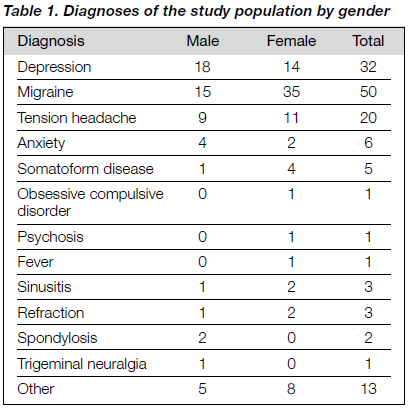
One hundred and thirty eight patients were included in the stum¡, of whom 57 (41.30%) were male and 81 (58.70%) were female. One hundred and three (74.64%) patients were married and 35 (25.36%) were single. The married group had a significant over-representation of females when compared with the unmarried group (66.02% vs 37.14%; Chi square = 8.98; df = 1; p = 0.00272). The mean age of the patients was 31.25 ± 10.57 years. The mean age of the males and females did not differ significantly (30.79 ± 10.80 years compared with 31.57 ± 10.46 years). The diagnoses of the study population by gender are shown in Table 1.
Forty five patients (32.6%) had a primary diagnosis of a psychiatric disorder. Depression was the commonest psychiatric disorder and was seen in 32 patients with headache (23.20%). This was followed by generalised anxiety disorder (GAD) in six patients with headache (4.30%) and somatisation disorder in five (3.60%). One patient (0.70%) had obsessive compulsive disorder (OCD) and one (0.70%) had non-organic psychosis. Comparison of patients with or without a psychiatric disorder showed no significant difference in the mean age of the patients (33.40 ± 10.01 years vs 31.20 ± 10.88 years). However, the psychiatric population had a higher number of males compared with the non-psychiatric population (52.27% vs 36.17%). This showed a trend towards significance (Chi square = 3.21; df = 1; p = 0.07). Further, 28 patients (20.30%) with headache with a psychiatric diagnosis had an illness duration of less than 1 year compared with 20 (21.28%) patients without such a diagnosis. This was found to be statistically significant (Chi square = 23.71; df = 1; p = 0.001). Amongst the patients with depression, 18 (56.25%) were male and 14 (43.75%) were female. The mean age of the patients with depression was 30.97 ± 10.78 years, with the males having a lower mean age than the females (27.06 ± 6.91 years vs 36.00 ± 12.90 years). This difference was found to be statistically significant (p = 0.017). The mean duration of illness among the patients with depression was 39.69 ± 72.43 months. Of these 32 patients, 19 (59.38%) had an illness duration of less than 1 year and 13 (40.62%) had an illness duration of more than 1 year, although the illness duration did not differ between males and females.
DISCUSSION
In this study, there was a preponderance of female patients, which was contrary to expectation since earlier outpatient- based studies done at this institute and at other centres in India have consistently found an over-representation of male patients in clinical trials.10-12 The commonest disorder among the study population was migraine (36.20%), followed by depression (23.20%). Both of these disorders are known to be more prevalent among females.13-15 In our sample, 70% of the patients suffering from migraine were female, which was consistent with the views of Adler and Adler13 that women are nearly three-fold more likely to have this disorder than men. Hence, this could explain the over-representation of females in the study population. A large body of evidence indicates that women are more prone to unipolar depression, which is supported from two sources of data on the rates of depression in men and women — records of persons treated for depression and surveys of the general population.16 However, in our study we found an over-representation of males, therefore, the preponderance of females in the study cannot be explained by the increased frequency of depression.
This study was conducted in a headache clinic located in a psychiatric unit, hence one might be tempted to explain the excess of psychiatric patients in the headache clinic by a referral artefact, such as patients being referred to the headache clinic to avoid the social stigma attached to mental illness in general and depression in particular.17,18 However, if this was true we should have expected an equal distribution of gender and not an excess of males as found. This preponder- ance of males in the psychiatric sample might be due to some other reason. A possible explanation could be the difference in the active response style of men towards their depressed mood as compared with women.
Chevron et al. are of the opinion that men and women experience depressive symptoms equally frequently and to the same degree, but because depression is perceived to be ‘feminine’, men are less likely to admit to it.19 Hence, a seriously depressed man might be unwilling to admit to depression and seek help for depressive symptoms.20 On the other hand, seeking help for a symptom such as headache may be more consistent with the male sex-role stereotype and perhaps more acceptable. This explanation seems quite plausible consider- ing the young age of the male patients. In fact, Boyd and Weissman15 and Hirschfeld and Cross21 have reported that sex-role stereotype is one of the important factors that affect help-seeking behaviour.
In our sample, 32.60% of patients had a psychiatric disorder, with depression being present in 23.20% of the entire sample. This is much less than the prevalence observed in some studies.2,3,6,7 The reason for this was that we used the ICD-10 criteria, whereas most of the earlier studies did not use such stringent operationalised criteria to make a psychiatric diagnosis.
Depression was found to be the commonest psychiatric disorder in headache patients. Headache has been recognised to be one of the complaints or the only complaint in up to 84% of depressed patients in clinical trials.22 The duration of a headache secondary to depression is believed to be an important distinguishing feature, often lasting for years.22,23 Interestingly, even though the mean duration of the headache in our depressed patients was 39.69 ± 72.43 months, 59.38% of patients had a duration of illness of less than 1 year. Hence the chronicity of the headache should not be over-emphasised in depressed patients, rather the physician should look beyond the physical symptom for which he is being consulted to avoid overlooking the underlying depression. It would be worthwhile mentioning that assessment of the role of depression could be complicated since several of the vegetative signs of depres- sion such as anorexia, sleep disturbance, lack of energy, and somatic complaints could be attributable to the headache as well. Hence, in a non-psychiatric unit, referral for a psychiatric evaluation or psychological testing would always be advisable.23
In conclusion, it can be said that migraine was found to be the commonest type of headache. It occurred more frequently in women, especially in the post-pubertal age group, than in men. The delayed onset of the sex difference in prevalence is an established fact and has been explained from a develop- mental perspective as well as by endocrinal factors. Psychiatric disorders, especially depression, accounted for the second com- monest type of headache. This was found to be more prevalent in relatively younger males, most of whom had an illness duration of less than 1 year. The focus of our attention should therefore be on young male patients with depression who may be elusive to psychiatrists and who need to be identified by physicians so that they can be effectively treated.
This was a retrospective study and therefore had all the limitations that such types of study have. In our study population, there was an underestimation of psychiatric morbidity as we took into consideration only cases that fulfilled the ICD-10 criteria for a psychiatric disorder, although psychological evaluation was done for all patients in whom a psychiatric disorder was suspected.
REFERENCES
- Packard RC. What does the headache patient want? Headache 1979;19:370-374.
- Merskey H. The characteristics of persistent pain in psychological illness. J Psychosom Res 1965;9:291-298.
- Large RG. The psychiatrist and the chronic pain patient: 172 anecdotes. Pain 1980;9:253-263.
- Lindsay PG, Wyckoff M. The depression-pain syndrome and its response to antidepressants. Psychosomatics 1981;22:571-577.
- Andrasik F. Psychological and behavioral aspects of chronic headache. Neurol Clin 1990;8:961-976.
- Kudrow L. Tension headache (scalp muscle contraction headache). In: Appenzeller O, ed. Pathogenesis and treatment of headache. New York: Spectrum; 1976.
- Diamond S. Depression and headache. Headache 1983;23:122 126.
- Headache Classification Committee for the International Headache Society. The classification and diagnostic criteria for headache dis- orders, cranial neuralgias and facial pain. Denmark: Scandinavian University Press; 1991.
- The ICD-10 classification of mental and behavioral disorders. Clinical description and diagnostic guidelines. Geneva: World Health Organization; 1992.
- Khanna R, Gupta N, Shankar S. Course of bipolar disorders in Eastern India. J Affect Disord 1992;24:35-41.
- Khess CRJ, Akhtar S. Jagawat T, et al. Gender and psycho- pathology in obsessive compulsive disorder. Indian J Psychiatry 1996;38:166-171.
- Khess CRJ, Das J, Akhtar S. Four year follow up of first episode manic patients. Indian J Psychiatry 1997;39:160-165.
- Adler CS, Adler SM. The migraine patient: descriptive studies. In: Adler CS, Adler SM, Packard RC, eds. Psychiatric aspects of headache. Baltimore: Williams and Wilkins; 1987:131-141.
- Weissman MM, Klerman GL. Sex differences in the epidemiology of depression. Arch Gen Psych 1977;34:98-111.
- Boyd JH, Weissman MM. Epidemiology of affective disorders: a re-examination and future directions. Arch Gen Psych 1981; 38:1039-1046.
- Nolen Hoeksema S. Sex difference in unipolar depression: evidence and theory. Psycho Bull 1987;101:259-282.
- Varma VK, Chakrabarti S. Social correlates and cultural dynamics of mental illness in traditional society: India. In: Al-Issa, ed. Handbook of culture and mental illness. Madison, WI: International University Press; 1995:115-127.
- Raguram R, Weiss Ma, Channabasavanna SM, Devins GM. Stigma, depression and somatization in south India. Am J Psychiatry 1996;153:1043-1049.
- Chevron ES, Quinlan DM, Blatt SJ. Sex roles and gender differences in the expression of depression. J Abnor Psychol 1978;87:680-683.
- Phillips DL, Segal BE. Sexual status and psychiatric symptoms. Am Sociol Rev 1969;34:58-72.
- Hirschfeld RMA, Cross CK. Epidemiology of affective disorders: psychosocial risk factors. Arch Gen Psych 1982;39:35-46.
- Diamond S. Depression and headache: a pharmacological pers- pective. In: Adler CS, Adler SM, Packard RC, eds. Psychiatric aspects of headache. Baltimore: Williams and Wilkins; 1987:259- 274.
- Packard RC. Emotional aspects of headache. Neurol Clin 1983;1:445-456.