Hong Kong Journal of Psychiatry (1999) 9 (1) 21-25
ORIGINAL ARTICLE
Summary
It has been postulated that obsessive compulsive disorder(OCD) lies in a continuum between schizophrenia and the neurotic disorders. Patients of pure OCD develop psychotic symptoms when there is a transient loss of insight or there is emergence of paranoid ideas. Depression is frequently associated with OCD, which could either be a complication of OCD or could be an independent coexisting disorder. In our study, 17 out of 52 OCD patients has psychotic features. Relatively more patients in the psychotic group were found to be single. They had higher scores on YBOCS, BPRS and HDRS( SIGH-D) as compared to the OCD patients without psychotic features. 76.4% of the patients with psychotic features also fulfill the DSM III-R criteria for Major Depressive Disorder. The possible explanation of the findings have been discussed in the light of relevant literature.
Key words: obsession, compulsion, psychotic symptoms, depressive symptoms
INTRODUCTION
Obsessive Compulsive Disorders (OCD) is characterized by recurrent obsessions or compulsions that are significantly distressing or time consuming or that cause significant interference with social or occupational functioning (DSM llIR, APA, 1987). It has been postulated that obsessive compulsive disorders lies in a continuum between schizophrenia and the neurotic disorders (Goldberg, 1965; Blacker, 1966). Obsessive compulsive symptoms have also been observed in schizophrenia (Stengel, 1945; Rosen, 1957; Fenton & McGlashan, ·1990), in whom obsession may precede schizophrenic symptoms. Earlier studies by Rudin (1953), Ingram (1961), and Lo (1967) have shown that 1%-10% of patients with OCD subsequently develop schizophrenia, however Goodwin et al (1969) pointed out that most of these studies had used a broad criteria for the diagnosis of OCD. lnspite of the high incidence of psychosis in OCD most of the cases cannot be diagnosed as schizophrenia according to current diagnostic systems.
Welner et al (1976) had reported that out of their 14 patients of OCD with psychotic symptoms (having delusions, hallucinations and formal thought disorders) only 2 met the criteria for schizophrenia while the remaining 12 showed prominent affective symptoms. The relation between OCD and depression is complex, with some believing depression to be a complication of OCD (Lo, 1967; Rosenberg, 1968; Goodwin et al, 1969), whilst others believe that OCD and depression are two distinct disorders which often co-exist (Monteiro et al. 1986; Jenike et al, 1987; Vallejo et al, 1988; Rasmussen & Eisen, 1989).
Goodwin et al (1969), after reviewing 13 follow-up studies had concluded that OCD patients were predisposed to depression but did not develop schizophrenia more frequently than non obsessional patients. In fact, Insel & Akiskal (1986) have asserted that in the current classificatory systems most of the OCD cases with psychotic features will be either diagnosed as mood disorders or paranoid state rather than schizophrenia.
The present study was conducted to assess the presence of psychotic features and depression simultaneously in OCD patients in whom schizophrenia was ruled out and to examine the relationship between the psychotic features and depression.
MATERIALS AND METHODS
This study was conducted at Central Institute of Psychiatry (C.I.P.), which is a 643 bedded premier postgraduate teaching institute situated in eastern India. It is run by the Central government of India, and is an important referral centre for the collieries, the railways, the states of Himachal Pradesh, West Bengal, Bihar, Orissa, the entire north-eastern states and parts of Uttar Pradesh and Madhya Pradesh. The hospital also gets referrals from the neighboring countries like Nepal and Bhutan. The Institute runs postgraduate training courses in Psychiatry, Clinical Psychology, Psychiatric Social Work and Psychiatric Nursing.
In the OPD all cases are worked up by junior residents. The history and the mental status examination of all the cases are recorded in a semistructured proforma and the diagnosis is made according to ICD-10 (W.H.O., 1992) criteria, after the case is discussed with a consultant or a post graduate senior resident.
For this study, all cases attending the Out Patient Department (OPD) between August 1992 to July 1994, who had received a diagnosis of OCD were reassessed, and only those cases which fulfilled the DSM III-R (APA, 1987) Criteria were included. Patients who fulfilled the DSM III-R criteria for schizophrenia or who had any history suggestive of organicity or who had a previous history of an affective episode (mania or depression) were excluded from the study.
The patients were assessed on Yale Brown Obsessive Compulsive Scale [YBOCS] (Goodman et al, 1989) for the presence as well as severity of obsessive and compulsive symptoms. They were also assessed on the Brief Psychiatric Rating Scale [BPRSJ (Overall & Klett, 1972] to study the psychopathology including the psychotic features. Depression was assessed by the Structured Interview Guide for Hamilton Depressing Rating Scale (SIGH-D; Williams, 1988). The patients were rated only once on each scale at the first contact by separate investigators who were blind to the scores on the other rating scales.
RESULTS
The study sample constituted of 52 patients. There were 35(67.30%) males and 17(32.70%) females. 29 (55.77%) patients were married, whereas 23 (44.24%) patients were single. The mean age of the patients at the first psychiatric consultation was 29.94 ± 10.98 years. The mean age of illness onset for the sample was 22.46 ± 8.47 years and the mean duration of illness was 7.48 ± 7.66 years.
In the sample, 19 (36.54%) cases had multiple form of obsessions and 17 (32.69%) cases had multiple content of obsessions. A single compulsion was present in 30(57.13%) cases, while multiple compulsions were present in 13(25.0%) cases. 9(17.31%) patients had only obsessions without any compulsions. The commonest form of obsessions was obsessive ruminations seen in 40 (76.92%) of the cases. The commonest content of the obsessions was contamination and dirt, seen in 28 (53.85%) cases. The commonest type of compulsion observed was washing compulsions, seen in 27 (51.92%) cases. (TABLE I)
The mean obsessive score on YBOCS was 13.46 ± 3.44, while the mean compulsive score was 10.9 ± 5.84.
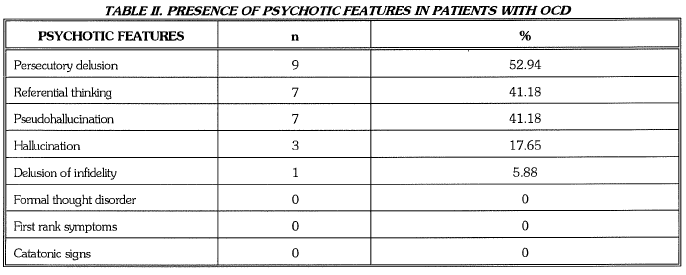
In our sample 17 (32.70%) patients had psychotic features and 35 (67.3%) patients had no psychotic features. Among the patients with psychotic symptoms 9 (52.94%) had persecutory delusions, 7 (41.18%) had delusion of reference, 1 (5.88%) had delusion of infidelity, 7 (41.18%) had pseudo hallucination and 3 (17.65%) had second person auditory hallucinations. (TABLE II)
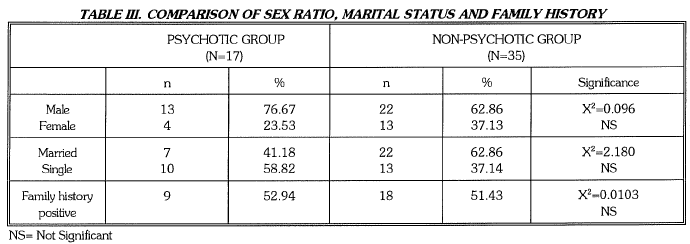
The mean age of illness onset in the psychotic group was 21±4.2 years compared to 23±9.85 years ('t'=0.6722, NS) in the non psychotic group. The mean duration of illness in the two groups was 6.35±5.84 years and 7.23±7.39 years respectively (t=0.438, NS). In the psychotic group 13 patients (76.47%) also fulfilled the DSM III-R criteria for a major depressive episode, whereas in the non-psychotic group 14 (40%) fulfilled the criteria for major depressive episode (p<0.01). Patients in the psychotic group, when compared with the non-psychotic group did not differ significantly in [1] age of onset [2] duration of illness [3] male female ratio, and [4] family history of psychiatric illness. Males were over represented in both the groups. In the psychotic group there were more patients who were single than married compared to the non-psychotic group, which showed a trend towards significance. (TABLE III)
Patients in the psychotic group had higher obsessive score (t=l.347) and compulsive score (t=l.227) on YBOCS which also showed a trend towards significance. Patients in the psychotic group had a higher score on BPRS (p<0.05), compared to those in the non-psychotic group. A positive correlation (r=0.734, p<0.01) was found between the BPRS and the HORS (SIGH-H) scores. On analysis of SIGH-D scores it was found that 15 (88.24%) patients in the psychotic group had depressive features compared to 16 (45.71%) patient in the non-psychotic group (p<O.01). (TABLE IV)
DISCUSSION
Looking at our sample of OCD cases, it appears that there is a preponderance of males, which is contrary to expectation. However, this apparent male dominance was an artifact, which became clear when the observed figures were converted into percentages of the total males and females attending the OPD during the study period. We found that only 0.72% of males were diagnosed as OCD whereas 1.03% females received a diagnosis of OCD. Male dominance in clinical sample of OCD has been observed in many studies from India, and it is a result of the referral bias, which has been discussed by us elsewhere (Khess et al, 1996).
In our sample 17 (32.7%) patients had psychotic features which was higher than the figures reported earlier, ranging from 6% to 20% (Rudin, 1953; Ingram, 1961; Rosenberg, 1968 & Solyom et al, 1985). In one study Jenike et al (1986) had described schizo-obsession in 32.6% of their sample, which was almost similar to our findings. The OCD patients with psychotic features did not differ from the patients without psychotic features except that there were more patients who were single or unmarried, and they had higher obsessive and compulsive scores, indicating a more severe pS1Jchopathology, which was similar to the findings of Solyom et al (1985). In the psychotic group 13 (76.47%) patients had a major depressive episode compared to 14 (40%) in the non-psychotic group. When the SIGH-D scores were analysed 15 (88.24%) patients in the psychotic group had depressive features compared to 16 (45.71%) in the non-psychotic group. Most of the earlier studies have reported depression in 30%-40% of their samples (Rachman & Hodgson, 1980; Coryell, 1981; Rasmussen & Eisen, 1992). The incidence in the psychotic group was much higher. Such high figures have also been reported by workers llke Turner (1984) and Zetin et al (1992) who have found depression in 70%-79% of their samples. The high incidence of both psychotic features and depression in our sample can be partially attributed to a sample bias, as the patients were taken from a mental hospital setup.


Stengel (1945) and Rosen (1975) had earlier emphasized the depressive and paranoid quality of their obsessional psychotics. An appreciable proportion of OCD patients become psychotic when there is a transient loss of insight or there is emergence of paranoid ideas (lnsel & Akiskal, 1986; Mirza-Hussain & Chaturvedi, 1988). The shift from an obsession to a delusion has been described when the resistance is abandoned and insight is lost (Gordon, 1950; Blacker, 1966; lnsel & Akiskal, 1986). This shift can either take an affective or paranoid form. Infact even paranoid shift can arise from disturbed affective processes, in that guilty preoccupation over a reprehensible thought or act may get transformed into a delusional conviction that one is being subjected to persecution (Insel & Akiskal, 1986). The strong association between psychotic features and depressive features in OCD is of interest from a phenomenological point of view and it may also have important implications in the treatment strategies in such cases. It should, however be kept in mind that often it may be difficult to ascertain whether the psychotic features are part of OCD or are due to the co-existing primary depression. A limitation of this study was that the patients were assessed only once and no follow up was conducted, hence the longitudinal course and association between psychotic features and depression in OCD can not be commented upon.
REFERENCES
American Psychiatric Association (1987) Diagnostic and Statistical Manual of Mental Disorders (ed. 3, revised) (DSM ill-R), Washington, D.C.
Blacker, K. (1966) Obsessive compulsive phenomena and catatonia states : continuum. Psychiatry, 29: 185-194.
Coryell, W. (1981) Obsessive compulsive disorders and primary unipolar depression : comparisons of background family history, course and mortality. Journal of Nervous and Mental Diseases, 169: 220-224.
Fenton, WS, McG!ashan, TH. (1990) Longterm outcome of obsessive compulsive disorder with psychotic features. Journal of Nervous and Mental Diseases, 178: 760-761.
Goldberg, GJ. (1965) Obsessional paranoid syndromes. Psychiatric Quarterly, 39: 3-64.
Goodman WR LH, Rasmussen SA, Mazure C, Fleischman RL, Hill CL, Heninger GR, Charney DS.(1989) The Yale Brown Obsessive Compulsive Scale. Development, use and reliability. Archives of General Psychiatry, 4: 1006-1011.
Goodwin DW, Guze SB, Robins E. (1969) Follow up studies in obsessional neurosis. Archives of General Psychiatry, 20: 182-187.
Gordon, A. (1950) Transition of obsession into delusions: evaluation of obsessional phenomenon from the prognostic standpoint. American Journal of Psychiatry, 107: 455- 458.
Ingram IM. (1961) Obsessional illness in mental hospital patients. Journal of Mental Science, 107: 382-402.
Inse! TR, Akiskal HS. (1986) Obsessive compulsive disorder with psychotic feature: a phenomenological analysis. American Journal of Psychiatry, 143: 1527-1533.
Jenike MA, Baer L, Minichiello WE. (1986) Coexistent obsessive compulsive disorder and schizotypal personality disorder : a poor prognostic indicator (letter). Archives of General Psychiatry, 43:296.
Jenike MA, Baer L, Brotman AW. (1987) Obsessive compulsive disorder and dexamethasone suppression test. Journal of Clinical Psychophannacology, 7: 182-184.
Khess CRJ, Akhtar S, Jagawat T, Das S, Srivastava A (1996) Gender and psycho- pathology in obsessive compulsive disorder. Indian Journal of Psychiatry, 38: 166-171.
Lo W. (1967) A follow up study of obsessional neurotics in Hong Kong. British Journal of Psychiatry, 113: 823-832.
Mirza Hussain KA, Chaturvedi. SK. (1988) Obsessive compulsive disorder with psychotic features: a case report. Indian Journal of Psychiatry, 30: 315- 317.
Monterio W, Marks IM, Noshirvari H. (1986) Normal dexamethasone test in obsessive compulsive disorder. British Journal of Psychiatry, 148: 326-329.
Overall JE, Klett CJ. ( 1972) Applied multivariate analysis. McGraw Hill Book Company, New York : 3-32.
Rachman SJ, Hodgson RJ. (1980) Obsession and compulsion, Eaglewood Cliff , Prentice Hall, New Jersey.
Rasmussen SA, Tsuang MT. (1984) The epidemiology of obsessive compulsive disorder. Journal of Clinical Psychiatry, 45: 450-457.
Rasmussen SA, Eisen JL. (1989) Clinical features and phenomenology of obsessive compulsive disorder. Psychiatric Annals, 19:2-5.
Rasmussen SA, Eisen JL. (1992) The epidemiology and differential diagnosis of obsessive compulsive disorder. Journal of Clinical Psychiatry, 53 (suppl.): 4- 10.
Rosen J. (1957) The clinical significance of obsession in schizophrenia. Journal of Mental Science, 103: 773-786.
Rosenberg CM. (1968) Complication of OCD. British Journal of psychiatry, 114: 477-478.
Rudin E. (1953) Ein beitrag zur frage zwangskranheit. Archive fur psychiatrie und Nervenkrankheiten, 191: 14-54.
So!yom L, DiNicola VF, Phil M, Sookman D, Luchins D. (1985) Is there an obsessive psychosis? Aetiological and prognostic factors of an atypical form of obsessive compulsive neurosis. Canadian Journal of Psychiatry, 30: 372 - 380.
Stengl E. (1945) A study of some clinical aspects of relationship between obsessional neurosis and psychotic reaction type. Journal of Mental Science, 91: 166-187.
Turner SM, Beidel DC, Nathan RS. (1987) Biological factors in obsessive compulsive disorders. Psychological Bulletin, 97: 430-450.
Vallejo J, Olivare Marcos T, Martinezosabas MJ, Ribera F, Bulbena A. (1988) Dexamenthasone suppression test and primary obsessional complsive disorder. Comprehensive Psychiatry, 29: 498-502.
Welner A, Reich T, Robins E, Fishman R, Doren TV. (1976) Obsessive compulsive neurosis: record, family and follow up studies. Comprehensive Psychiatry, 17: 527-539.
Williams JB. (1988) Structured interview guide for the Hamilton Depression Rating Scale. Archieves of General Psychiatry, 45: 742-747.
World Health Organization (1992) The ICD-10 classification of mental and behavioural disorders: Clinical description and diagnostic guidelines, Geneva.
Zetin M, Kramer MA. (1992) Obsessional compulsive disorder. Hospital and Community Psychiatry, 43: 689- 699.
Christoday R.J. Khess M.D.(Psychiatry), Associate Professor of Psychiatry, Central Institute of Psychiatry
Jnanamay Das DPM(Psychiatry) , Resident in Psychiatry, Central Institute of Psychiatry
Arunanshu Parial DPM(Psychiatry), Resident in Psychiatry, Central Institute of Psychiatry
Sonia Kothari MBBS, Resident in Psychiatry, Central Institute of Psychiatry
Thresiamma Joseph M.Phil(Medical & Social Psychology), PhD. Clinical Psychologist, Central Institute of Psychiatry
Correspondence: Dr. Christoday R.J. Khess, Associate Professor of Psychiatry, Central Institute of Psychiatry, Kanke, Ranchi-834006, Bihar, India


