Hong Kong Journal of Psychiatry (1996) 6, 4-13
ORIGINAL ARTICLE
Summary
Existing rating scales for formal thought disorder do not fully take into consideration levels of language organisation as suggested by modern linguistics science. A new scale, the Clinical Language Disorder Rating Scale (CLANG), is proposed using a framework based upon linguistically meaningful levels of organisation. The scale was validated in an extensive sample of 204 Hong Kong Chinese schizophrenic patients. Good interrater and internal reliabilities were obtained. Factor analysis revealed three major domains of language disorder captured by the scale: the semantic level, the syntactic level, and the production level. Satisfactory convergent and criterion validity were established by comparing CLANG subscale scores with ratings based on other standard instruments. We conclude that CLANG is a reliable, valid and informative instrument for clinical assessment of language disorder in schizophrenia.
Keywords: formal thought disorder, language, schizophrenia, rating instrument, validation.
INTRODUCTION
Formal thought disorder (language disorganisation) is an important sign in schizophrenia. Compared to other psyc hotic symptoms (such as hallucination and delusions), lang uage disorganization could be directly observed and is not dependent upon subjective report of abnormal experiences on the part of the patient. Consequently language disorgan ization can be regarded as one of the more informative clinical marker of brain dysfunction in psychosis (Taylor et al 1994). Another impetus for the study of language disorg anisation has been the delineation of a disorganization syn drome in schizophrenia (in which language dysfunction is a major component) which is independent of positive and negative symptoms (Bell et al 1994; Bassett et al 1994;
Thompson & Meltzer, 1993; Malla et al 1993; Peralta et al 1992). Recent neuroimaging studies have provided prelim inary evidence for specific neurobiological correlates of the disorganisation syndrome (Liddle et al 1992; Rossi et al 1994; Shenton et al 1992).
Evaluation of language disorder in psychiatry has not been a trivial task. Many approaches have evolved in the past decades. They could be divided into two board catego ries: firstly, detailed post hoc analysis of language output (e.g. complexity of sentence structure, relative frequencies of adjectives and qualifying clauses etc.) (Manschreck et al 1991; King et al 1990; Morice, 1986; Fraser et al, 1986; Morice & McNicol, 1985 & 1986; Morice & !gram, 1983); and secondly, real-time ratings based on clinician judgment (Simpson & Davis, 1985). The former is time consuming and objective rating is mostly confined to the level of syntax (grammar) analysis. Clinician-rated scales have the addi tional advantage of full access to all levels of contextual information.
However, existing clinician-rated scales for formal thought disorder suffer from a variety of shortcomings. For example, the Thought, Language and Communication diso rder rating scale (TLC) (Andreasen & Grove, 1986; Andreasen, 1979a & 1979b) adopted and re-defined some relatively dated psychopathological terms and does not take into full consideration recent advances in the understanding of language organization. There is consequently need for a new and relatively simple rating instrument which is based on a modern psycholinguistic framework.
Studies in psycholinguistics over the last few decades have suggested several different levels of language organi zation. At each level basic units interact with one another and operate within a distinct set of rules unique to the level. For example, words are constructed from phonemes (basic units of speech sound) based on particular rules (not all permutations of letters and phonemes are legal). At the level of syntax, sentences are constructed from words and clauses according to grammatical rules. Semantics addresses how meanings are conveyed by words or clauses.
At the level of discourse, larger units (sentences) are arranged to enable coherent expression of complex ideas. The segregation of language processing into these level is not absolute nor complete (i.e. cross-level constraints do exist). Nevertheless these major levels of language organi zation provide a rational framework for capturing the com plexity and diversity of language pathology.
In this context a new language disorganisation rating instrument (the Clinical Language Disorder Rating Scale, abbreviated CLANG) was developed based on well recog nized levels of linguistic organisation. We describe validation of the instrument in a sample Hong Kong Chinese Schizo phrenic patients. After the interrater and internal reliability of the inventory was established, factor structure of the instrument was explored. Criterion and convergent validity were evaluated by correlation analysis with standard rating instruments.
METHODS
SUBJECTS
Patients from 16 to 65 years of age and meeting DSM III-R diagnostic criteria for schizophrenia (American Psychi atric Association, 1987) were recruited from acute and continuing care inpatient facilities for the validation and reli ability study. Diagnosis was established by information obta ined in a clinical interview and review of clinical notes. Pati ents were carefully screened and those with co-morbidity in substance abuse, organic disorder, mental retardation, recent history of having electroconvulsive therapy (within 2 years) as well as a history of leucotomy were excluded. 204 patients participated in a validation and factor structure study for the CLANG. 14 additional subjects were involved in the interrater reliability study.
ASSESSMENT OF SYMPTOMS
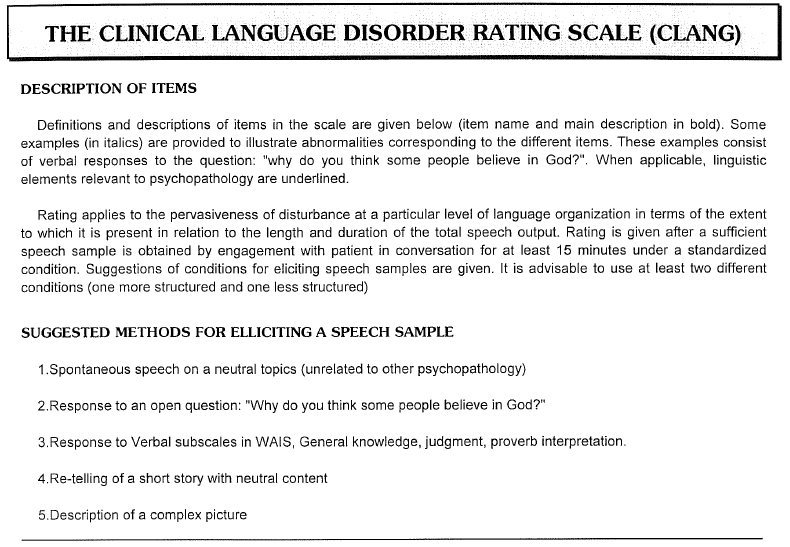
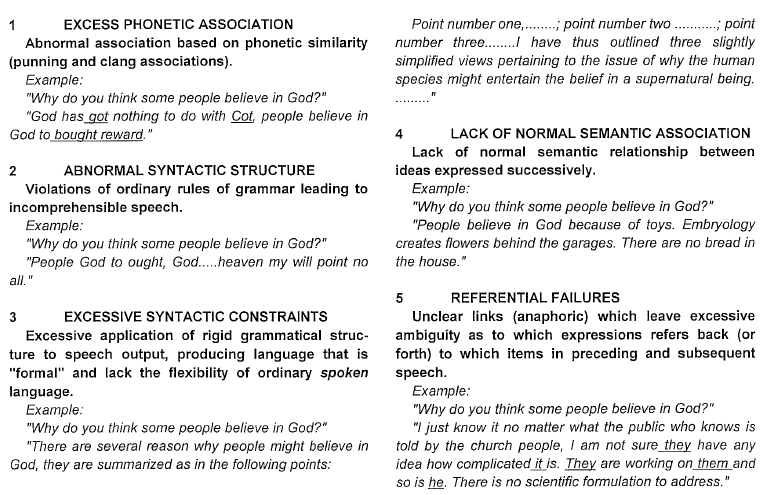
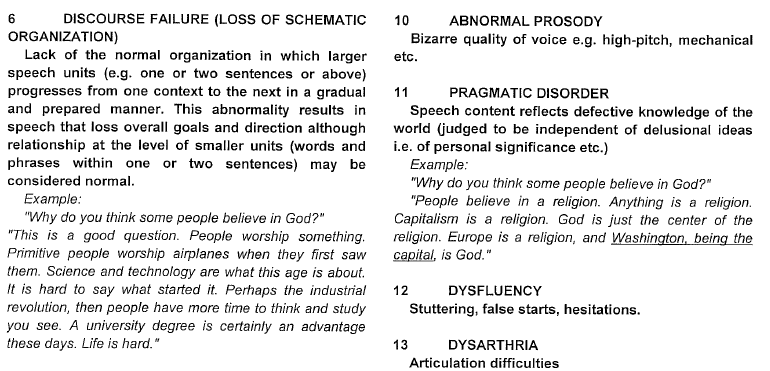
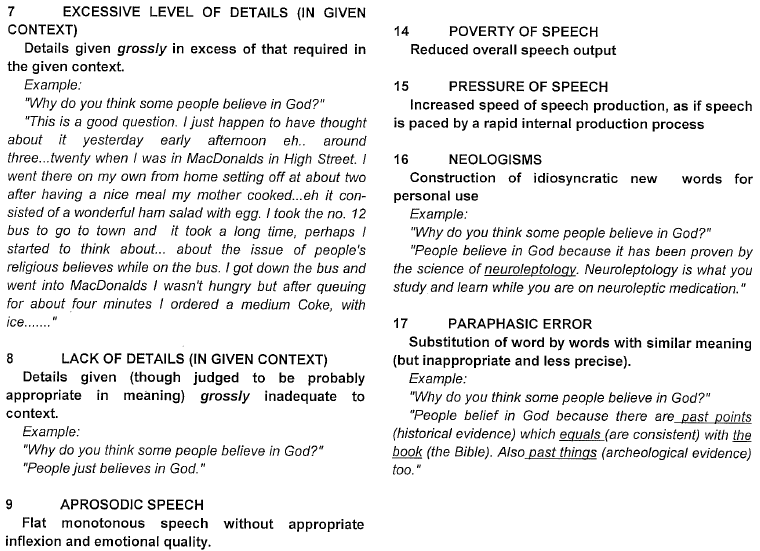
Clinical Language Disorder Rating Scale (CLANG)
The scale consisted of 17 observer-rated items anchored on a four point severity scale (see Appendix 1). Rating was based on verbal output during a period of conversation with the patient (lasting at least 15 minutes). CLANG ratings in the validation study were carried out by raters blind to the results of other clinical ratings.
The Brief Psychiatric Rating Scale (BPRS)
Symptom assessment was carried out for each patient with the 18-item Brief Psychiatric Rating Scale (BPRS) (Overall & Gorham, 1962). Semi-structured assessment and anchored rating were used according to Lukoff et al (1986). The BPRS has been successfully used in the Hong Kong Chinese population for assessment of psychopathology (Chan & Lai, 1993). The interrater reliability was ascer tained by rating a further 20 patients. The intraclass corre lation (Bartko & Carpenter, 1976) for BPRS items ranges from 0.84 to 0.99.
Thought, Language and Communication disorder rating scale (TLC) items
These items were used in the present study to provide an independent way of assessing formal thought disorder. lnterrater reliability was assessed by 3 raters on a further 14 patients. The intraclass correlation coefficient for the scale was 0.96.
The High Royd Evaluation of Negativity Scale (HEN) The HEN scale for negative symptom rating consisted of 18 observer-rated items falling into six domains, covering appearance , behaviour , speech , thought , affect and functioning (Mortimer et al 1989). In each of these areas, a global score was assigned after rating the individual items. All items were rated along an anchored five-point severity scale. A final score was derived from summing the global score from each of the six domains. Interrater reliability (intraclass correlation coefficient based on a further 20 pati ents) for the overall score in the HEN was 0.92.
RESULTS
THE VALIDATION SAMPLE
204 patients participated (122 Male, 82 Female; mean age 40.5 years; s.d. 12.2 years) in the validation study. The mean duration of illness was 15.1 years (s.d. 9.8). The mean daily neuroleptic dosage was 940 mg of chlorpr omazine equivalent (s.d. 1007 mg). The mean daily dosage of benzhexol was 3.2 mg (s.d. 3.3 mg).
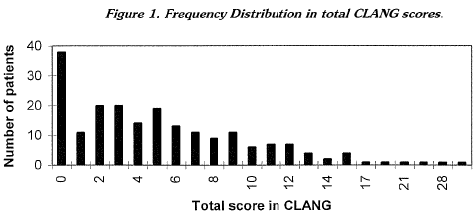
The median CLANG score for the sample was 4. The frequency distribution is shown in Figure 1. CLANG total score was negatively correlated with education (Pearson correlation coefficient -0.24; p<0.001). However this correlation was probably confounded by illness duration and negative symtpoms as the partial correlation between educ ation and CLANG score controlling for negative symptom score and illness duration was not significant (partial corre lation coefficient -0.11; p=0.10).
FACTORIAL STRUCTURE OF LANGUAGE DISOR DER RATED BY CLANG
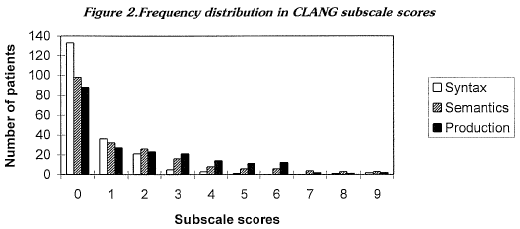
A factor analysis (principal component analysis with varimax rotation) was carried out over the 17 CLANG indi vidual items. Five factors were extracted using an eigen value of > 1 as criterion for interpretation, accounting for 87.9 percent of the total variance (See Table 1). Most of the variance (48.3 percent) was accounted for by the first three factors which corresponded to syntactic disorders, semantic disorders and production disorder respectively. A fourth factor corresponded to pressured speech and accounted for 8.4 percent of the variance. The final factor corresponded to theabnormal prosody item. The first three factors were adopted as a basis for constructing three subscales for the CLANG and their scores were used in fur ther analysis. Distribution of the subscale scores for the sample is shown in Figure 2. Columns labelled 9 include two instances of scores above 9 (both found in subscale "syntax", actual scores 12 and 15 respectively).

INTERNAL RELIABILITY
The internal consistency of the CLANG and the relative contribution of individual items was characterized by apply ing Cronbach lpha coefficient to the data set (table 2). The internal reliability for the subscales was generally high (alpha coefficient 0.76 for the semantics subscale; 0.80 for the syntax subscale; and 0.72 for the production subscale). The alpha coefficient for the entire scale was 0.76. Alpha coefficients with items removed showed that the pragmatics item in the semantics subscale was better considered as separate. It was removed from the subscale in subsequent analysis.
INTERRATER RELIABILITY
Interrater reliability was ascertained by three of the inve stigators jointly rating another 14 patients. The intraclass correlation (Bartko and Carpenter, 1976) was 0.88 for the full scale. Intraclass correlation coefficient for the subscales were as follows: syntax subscale 0.93; semantics subscale 0.83; and production subscale 0.88.
CONVERGENT VALIDITY: RELATIONSHIP OF CLANG SCORE TO BPRS FACTORS
To the knowledge of the authors, the CLANG was the first formal thought disorder rating scale to be validated for use in the Chinese Hong Kong population. Convergent validity was therefore assessed by comparing HEN ratings with a general psychopathology rating instrument, the BPRS, which has been successfully applied to the Hong Kong Chinese population (Chan and Lai, 1993). In this sample of 204 patients, BPRS items segregated into five factors (details reported elsewhere). Factor one consisted of negative symptoms (Blunted affect, Motor retardation, Emotional withdrawal). Factor two consisted of positive symptoms (Unusual thought content, Suspiciousness, Hallucinatory behaviour). Factor three consisted of affective symptoms (Depressive mood, Guilt feelings). Factor four comprised anxiety symptoms (Tension, Anxiety). Factor five was a disorganisation factor (Conceptual disorganization, excitement).
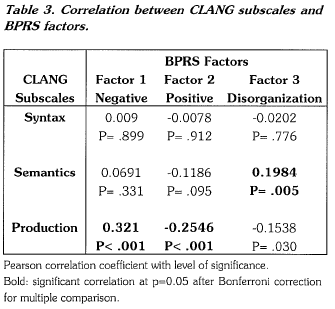
BPRS Factors 1 (negative), 2 (positive) and 5 (disorgan ization) were correlated with the CLANG subscales (table 3). The semantic factor was, as expected, correlated with the BPRS disorganisation factor. The production CLANG factor was correlated with the negative factor in the BPRS. An inverse correlation between the production factor in the CLANG and the positive BPRS factor was also observed. The syntax CLANG factor was not correlated with BPRS factors.
CRITERION VALIDITY
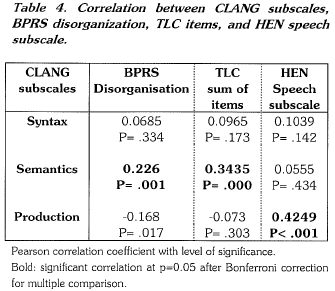
CLANG subscale ratings were compared with corre sponding ratings from established scales designed to meas ure different aspects of language disorder. The semantic factor was correlated with formal thought disorder items in the CASH (i.e. TLC items) and in BPRS. The production factor was correlated with speech subscale score in the HEN scale. The syntax factor was not correlated with any of these measures (Table 4 ).
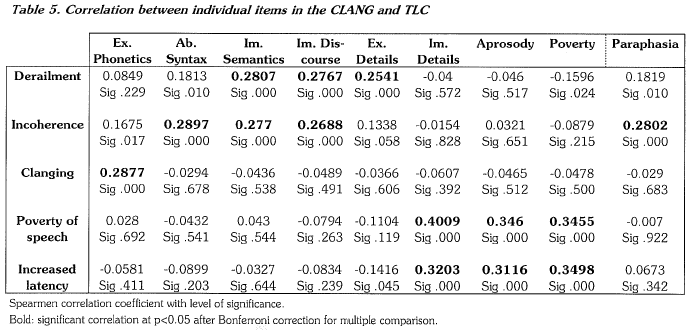
To assess how well the CLANG items were capturing what they were meant to measure, individual item ratings in the CLANG was correlated with individual items in the TLC. Table 5 below shows that abnormal phonetics (CLANG) was correlated with clanging (TLC); Abnormal syntax and paraphasia (CLANG) was correlated with incoherence (TLC); Lack of semantic relationship and discourse failure (CLANG) was correlated with derailment and incoherence (TLC); Lack of details, aprosody and poverty (CLANG) were correlated with the items poverty of speech and increased latency of response in the TLC. These individual item correlations further support the face validity of the CLANG at the level of single items.
DISCUSSION
We present validation and reliability data on a new rating scale for formal thought disorder. The scale was demon strated to be reliable and valid for use on Hong Kong Chinese patients. Although the scale was primarily validated in a sample of schizophrenic patients, its design and struc ture do not preclude application to patients with other con ditions (such as mania and dementia). The primary objective of the scale is to enable quantification and characterization of language-related psychopathology within a framework consistent with modern understanding of language organi sation. Like other observer-rated language disorder scales, this scale was not primarily designed for diagnositic or screening purposes. The use of the scale requires careful study of the item description and considerable practise in order to acquire the skill to monitor ongoing language pro duction in the patient. For research purposes, inter-rater reliability has to be re-established in the prospective research team.
The use of an extensive validation sample has enabled a preliminary exploration in the factor structure of language disorders in schizophrenia. Three main orthogonal (independent) domains of language abnormality are identi fied. They correspond to abnormalities at the level of semantic processing (corresponding to the traditional idea of loose associations); abnormality at the syntactic level (which is associated with phonetic abnormalities and abno rmal word choice, such as paraphasic error and neologism, and are distinguished from genuine semantic dysfunctions); and finally, the level of production disorder (corresponding to the notion of poverty of speech). The segregation of abnormalities into these three independent groups suggests that language disorder in schizophrenia is probably a reflec tion of complex interaction between factors located at multiple levels in the language production process. Full characterization of these levels will require further research.
Recent advances in cognitive psychology and neuroimag ing have conferred promises for better understanding of the neurobiological basis of psychotic symptoms. Among the latter, formal thought disorder is a potential candidate for intensive symptom-orientated research. The outcome of the search for neurobiological correlates, however, is crucially dependent upon the clinical measurement instrument. In addition to being reliable, a useful instrument is required to be able to capture clinical information at an optimal level of abstraction, that is, at a level of organisation which conceiv ably might map onto neurobiological findings. In this light it is crucial that formal thought disorder rating instruments continue to evolve with advancing knowledge in cognitive science. The current instrument is presented as offering a step in this direction.
ACKNOWLEDGMENT
The study was partly supported by a CRCG Grant from the University of Hong Kong. We are grateful to the patients and staff of Kwai Chung Hospital, Lai Chi Kowk Hospital, and Queen Mary Hospital for their facilitation and participation in the study.
REFERENCES
American Psychiatric Association, (1987) Diagnostic and Statis tical Manual of mental disorders, 3rd, American Psychiatric Association, Washington, DC,
Andreasen, N.C. (1979a) Thought, language, and communication disorders. II. Diagnostic significance, Archives of General Psychiatry, 36, 1325-1330.
Andreasen, N.C. (1979b) Though, language, and communication disorders. I. Clinical assessment, definition of terms, and evalua tion of their reliability, Archives of General Psychiatry, 36, 1315-1321.
Andreasen, N.C. & Grove, W.M. (1986) Thought, language, and communication in schizophrenia: diagnosis and prognosis, Schizophrenia Bulletin, 12, 348-359.
Bartko, J.J. & Carpenter, W.T. (1976) On the methods and theory of reliability, Jounral of Mental and Nervous Disease, 163(5), 307-317.
Bassett, A.S.; Bury, A. & Honer, W.G. (1994) Testing Liddle three-syndrome model in families with schizophrenia, Schizo phrenia Research, 12, 213-221.
Bell, M.D.; Lysaker, P.H.; Beam-Goulet, J.L.; Milstein, R.M. & Lindenmayer, J.P. (1994) Five-component model of schizo phrenia: assessing the factorial invariance of the positive and negative syndrome scale, Psychiatry Research, 52, 295- 303.
Chan, D.W. & Lai, B. (1993) Assessing psychopathology in chinese psychiatric patients in Hong Kong using the Brief Psychiatric Rating Scale, Acta Psychiatrica Scandinavica, 87(1), 37-44.
Fraser, W.l.; King, K M.; Thomas, P. & Kendell, R.E. (1986) The diagnosis of schizophrenia by language analysis, British Jour nal of Psychiatry, 148, 275-278.
King, K; Fraser, W.l.; Thomas, P. & Kendell, R.E. (1990) Reexamination of the language of psychotic subjects, British Journal of Psychiatry, 156, 211-215.
Liddle, P.F.; Friston, KJ.; Frith, C.D.; Hirsch, S.R.; Jones, T. & Frackowiak, R.S. (1992) Patterns of cerebral blood flow in schizophrenia, British Journal of Psychiatry, 160, 179- 186.
Lukoff, D.; Liberman, R.P. & Nuechterlein, KH. (1986) Symptom monitoring in the rehabilitation of schizophrenic patients, Schizophrenia Bulletin, 12 (4), 578-602.
Malla, A.K.; Norman, R.M.; Williamson, P.; Cortese, L. & Diaz, F. (1993) Three syndrome concept of schizophrenia. A factor analytic study, Schizophrenia Research, 10, 143-150.
Manschreck, T.C.; Maher, B.; Celada, M.T.; Schneyer, M. & Fernandez, R. (1991) Object chaining and thought disorder in schizophrenic speech, Psychological Medicine, 21, 443- 446.
Morice, R. (1986) Beyond language--speculations on the prefrontal cortex and schizophrenia, Australian & New Zealand Jour nal of Psychiatry, 20, 7-10.
Morice, R. & McNicol, D. (1985) The comprehension and produc tion of complex syntax in schizophrenia, Cortex, 21, 567- 580.
Morice, R. & McNicol, D. (1986) Language changes in schizo phrenia: a limited replication, Schizophrenia Bulletin, 12, 239-251.
Morice, R.D. & Igram, J.C. (1983) Language complexity and age of onset of schizophrenia, Psychiatry Research, 9, 233-242. Mortimer, A.M.; McKenna, P.J.; Lund, C.E. & Mannuzza, S. (1989) Rating of negative symptoms using the High Royds Evaluation of Negativity (HEN) Scale, British Journal of Psychiatry; 155 (suppl. 7), 89-91.
Overall, G.E. & Gorham, D.R. (1962) The brief psychiatric rating scale, Psychological Reports, 10, 799-812.
Peralta, V.; de Leon, J. & Cuesta, M.J. (1992) Are there more than two syndromes in schizophrenia? A critique of the positive negative dichotomy, British Journal of Psychiatry, 161, 335-343.
Rossi, A.; Serio, A.; Stratta, P.; Petruzzi, C.; Schiazza, G.; Mancini, F. & Casacchia, M. (1994) Planum temporale asymmetry and thought disorder in schizophrenia, Schizophrenia Research, 12, 1-7.
Shenton, M.E.; Kikinis, R.; Jolesz, F.A.; Pollak, S.D.; LeMay, M.; Wible, C.G.; Hokama, H.; Martin, J.; Metcalf, D.; Coleman, M. & et al, (1992) Abnormalities of the left temporal lobe and thought disorder in schizophrenia. A quantitative magnetic reso nance imaging study, New England Journal of Medicine, 327, 604-612.
Simpson, D.M. & Davis, G.C. (1985) Measuring thought disorder with clinical rating scales in schizophrenic and nonschizophrenic patients, Psychiatry Research, 15, 313-318.
Taylor, M.A.; Reed, R. & Berenbaum, S. (1994) Patterns of speech disorders in schizophrenia and mania, Journal of Nervous and Mental Disease, 182, 319-326.
Thompson, P.A. & Meltzer, H.Y. (1993) Positive, negative, and disorganisation factors from the Schedule for Affective Disorders and Schizophrenia and the Present State Examination. A three-factor solution, British Journal of Psychiatry, 163, 344-351.
*Eric Y.H. Chen MA(Oxon) MBChB. MRCPsych Lectu rer i n Psychiatr y, University of Hong Kong Linda C.W. Lam MBChB, MRCPsych., Lectu rer in Psychiatr y, Chinese University of Hong Kong Ronald Y.L. Chen, Bsc. MBBS. MRCPsych. Lectu rer in Psychiatr y, University of Hong Kong Charlotte KY. Chan BA. PCPsy. MsocSc. Formerly research assistant, University of Hong Kong Carol L. Kwok MB, Research assistant, University of Hong Kong C.S. Kan MRCPsych, Senior Med ical Of ficer, Castle Peak Hospital Desmond G.H. Nguyen, MBBS, MRCPsych. Senior Medical Officer, Kwai Chung Hospital
*Correspondence: Dr Eric Chen, Department of Psychiatry, University of Hong Kong, Queen Mary Hospital, Pokfulam Road, Hong Kong.