J.H.K.C. Psych. (1994) 4, SP2, 7-12
ORIGINAL PAPER
ELDERLY PSYCHIATRIC INPATIENTS AND THEIR AGE OF ONSET
T.W. Fan
SUMMARY
324 (13.5%) of all the registered psychiatric inpatients of Castle Peak Hospital belongs to the age ≥65 on 15 June 1993. Their demographic data, psychiatric diagnosed and age of onset were surveyed by case note review by the author. Female elderly patients were found to be more significantly more prevalent (especially among the old-olds), about 5 years older in their mean age, age on admission and age of onset of mental illnesses than the male elderly. 175 cases were diagnosed to be suffering from schizophrenia, 18 from paraphrenia, 31 from paranoid, 64 from dementia and 18 from affective disorder. Their mean age of admission was 6.42 years. 70% of cases had their age of onset ≤65 and 70% of these were schizophrenics. It is conformed that elderly inpatients of Castle Peak Hospital consisted mainly by long-stay schizophrenics/ Local data were reviewed and implications for psychogeriatric services planning is further discussed.
Keywords: psychogeriatrics, epidemiology, age of onset, elderly
INTRODUCTION
Now that psychogeriatric services are budding vigorously to cater for the escalating needs of the aging society in Hong Kong, there is still much misunderstanding and confusion about the target patients of the psychogeriatric services. Some misunderstanding arises that all the elderly psychiatric patients would be under care of the psychogeriatric teams similar to the case of geriatrics. This ambiguity arises more in the inpatient setting when the psychogeriatric services are newly developed and redistribution of workload and resources are necessary.
Very often the hospital administration, nurses, other disciplines and sometimes even the psychiatrists have the notion of handing over all the patients of age 65 or above under their service to the new psychogeriatric teams. Their idea is that since these patients are both psychiatric patients and old, they should be under the care of the psychogeriatric services.
DHSS (1972) divided elderly patients with psychiatric problems (in mental hospitals) into 3 board groups:
- old long-stay patients grown old in hospital;
- elderly patients with functional mental illnesses; and
- elderly patients with
The first group would be under care of the general adult psychiatric services while the other 2 groups would be under care of the psychogeriatric services
Psychogeriatric services would be responsible in assessment and treatment as well as consultation-liaison psychiatric services for elderly new to the Mental Health Services. Functional psychiatric illnesses with onset <65 should be cared by general adult psychiatric services, while some organic cases, e.g. presenile dementia, may be referred to the psychogeriatric services by the general adult psychiatric services if indicated (Wattis et al, 1987).
Henceforth it is necessary to differentiate between the 2 groups of "mad growing old" cases (elderly psychiatric patients with their illness onset before age 65) and the "old growing mad" cases (elderly persons presenting with mental illness after 65) in the process of services planning and resources allocation for the psychogeriatric services. Further breaking them down into the functional illness and organic illness is also important.
AIM
The aim of the present study is to obtain some local demographic data of the elderly inpatients in psychiatric hospital and to differentiate between the 2 groups by studying their age of onset.
METHODOLOGY
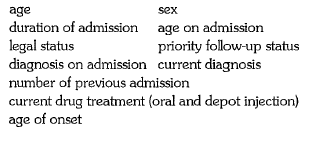
All inpatients aged 65 or above registered as inpatients of Castle Peak Hospital at midnight of 15 June 1992 were surveyed with the assistance of the nursing staffs in each ward. The following demographic data were then extracted from the case records by the author:
The initial diagnosis on admission referred to the diagnosis written down either after firm meeting discussion or the diagnosis put down on the formulation sheet. If both were missing, the diagnosis written in the progress record around 2 weeks after admission was taken. Current diagnoses refer to the most recent diagnosis as recorded in the progress sheet, case summary or annual review sheet. For cases with a subsequent change of diagnoses, the case notes was reviewed for determination of a more appropriate age of onset for the current diagnosis.
Age of onset was estimated from the age of first presentation to psychiatric services either as inpatients or outpatients and the duration of onset before first contact. Because the date of fist contact may be many years back, therefore the age at first presentation to mental health service would be taken as the age of onset. It must be emphasized that this age of onset would be only a gross estimation. Anyway this is considered to be an acceptable parameter for the purpose of the present study.
RESULTS
DEMOGRAPHIC DATA
Age & Sex
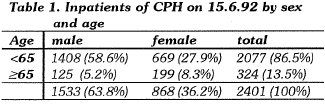
Of the 2401 registered inpatients of Castle Peak Hospital at midnight of 15 June 1992, 324 (13.5%) were elderly patients of age 65 or above. Elderly patients took up 8% of all the male patients and 23% of all the female patients. There is a reversal of sex predominance bestrewn the 2 age groups with significantly more female among the elderly population (x2= 90.1, d.f.=l, p<0.001). (See Table 1)
Among the elderly inpatients, age of the females (mean=75.7, s.d.=7.2)were significantly older than that of the males (mean = 70.4, s.d.= 5.3) (t= 7.65, d.f.= 322, p<0.001) by about 5 years. This female predominance was actually more marked among the old-old (75+) group as 104 of the female elderly belonged to the old-old group while only 15% of all male elderly did (x2 = 44.7, d.f.= 1, p<0.001). The oldest patient was a female aged 100 years old. (See Table 2)
Age at Current Admission
The age at current admission ranged from 30 to 95. The female patients' age at current admission (69.17, s.d.=10.31) were significantly older ( by about 5 years) at time of current admission than the males (64.10, s.d.=8.41)(t=4.84, d.f.=322, p<0.001).
Duration of admission
The mean duration of admission is about 6.42 years (s.d.=6.68). The case with the longest duration of hospitalization (37.5 years) had her stay dated back to the old Mental Hospital before its transfer to Castle Peak Hospital in 1961. 24% of elderly patients were admitted for less than 9 months, 31% between 9 months to 5 years and 45% of the patients were admitted for more than 5 years. 20% cases had stayed for more than 10 years. There is no significant difference between the male and female elderly. The majority of these elderly inpatients were long-stay cases.
If we look specifically at the duration of admission for the 2 diagnoses of schizophrenia and dementia, we can see that the 175 schizophrenics (8.99 years, s.d.=7.65 max.=37.5) has a much longer duration of stay than the 64 dementia cases (2.99 years, s.d.= 3.19, max.=13.5) (t=8.466, d.f.=237, p<0.001).
Readmission
In one third (110) of cases, the current admission was their first admission to Castle Peak Hospital. There is no difference between male and female in this aspect.
Legal Status
Half of the cases were initially admitted as voluntary patients while only 20 of the 324 cases were currently detained involuntarily.
PFU Status
Only 65 cases were labeled as priority-follow-up cases of which the male patients were significantly more prevalent especially for the 13 subtarget cases (x2=41.0, d.f .=1, p<0.001).
Diagnoses
The 5 diagnoses as shown in Table 3 constitute 95% (306) of all cases. There was no statistically significant difference between the male and female patients in any of these diagnoses.
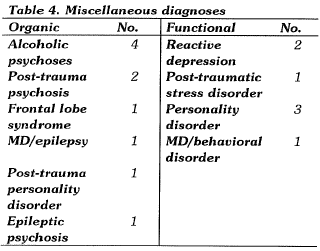
It can be seen that psychoses predominate in these elderly psychiatric inpatients. The author while reviewing the diagnoses from the case notes was impressed by the loose use of the diagnoses of schizophrenia and paraphrenia. Therefore the two were lumped together as one entity in the later analyses. Further study revealed that 3 of the dementia cases were labeled as multi-infarct dementia; 9 of the affective cases were major depression and 20 cases had their diagnoses revised. Besides the 5 current diagnoses, other miscellaneous diagnoses were tabulated in Table 4:
Organic/functional illnesses
From Tables 3 and 4, it can be seen that more than 75% (259) of the cases were suffering from functional mental illnesses.
Drug treatment
191 of the 324 cases were on oral psychoactive drugs only while 55 were on both oral and depot psychoactive drugs. 12 cases were maintained on depot psychoactive drugs alone. 20% (66) of patients were not on any psychoactive drugs on date of survey.
AGE OF ONSET
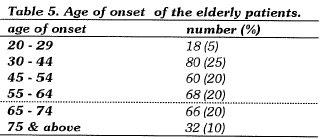
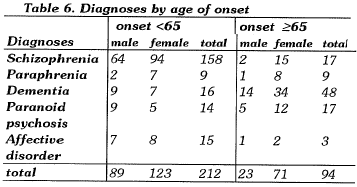
It can be seen from Table 5 below that 70% (226) of these patients had their mental illness onset at an age below 65. Actually 50% cases had their age of onset before 55. 70% of these cases with onset age below 65 were schizophrenia. These cases should not be under the psychogeriatric services but remained under the general adult psychiatric services (DHSS, 1972; Wattis et al, 1987).
Sex and Age of Onset
The mean age of onset for all female patients was 56.60 years (s.d.=16.35), about 5 years older than that of the male patients (51.54 years, s.d.=13.99). This was statistically significant (t=2.97, d.f.=322, p<0.01). If we concentrate on those 98 patients with age of onset ≥65, there was significantly more female patients than the male ( x2=13.54, d.f.=1, p<0.001).
Diagnoses and Age of Onset
From Table 6, it can be seen that schizophrenia and affective disorder have their onset more before 65 while dementia more ≥65. Paraphreina and paranoid psychoses were less distinct in this aspect. It can also be seen that male and female were more or less the same in presenile dementia while female was more prevalent among the senile dementia. A change in sex predominance by onset age of 65 can be seen among many of the diagnoses.
Organic illness and age of onset
Organic mental illnesses were significantly more prevalent among those patients with an age of onset 2:65 (x2= 56.94, d.f.=1, p<0.001). It can be seen that the functional illnesses was as prevalent as organic illnesses among patients with onset age 2:65. Among the 75 organic cases, there is a reversal of sex predominance with significantly more (35)female had their onset at or above 65 while more (18) male had onset before 65. (x2=11.49, d.f.=1, p<0.001). (See Table 7)
DISCUSSION
LOCAL DATA
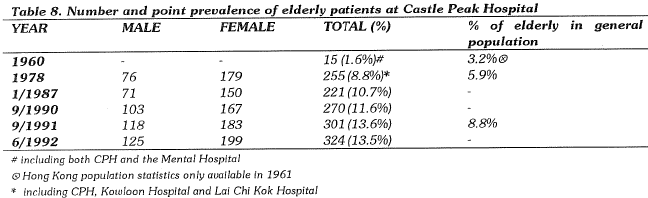
The author's effort in reviewing the local data on the elderly psychiatric inpatients was not rewarding at all. The data collected were tabulated in Table 8 above.
The 1960 and 1978 data were not limited to inpatients of Castle Peak Hospital alone and referred to all the psychiatric inpatients of the Mental Health Service (Lo, 1982). The very low number in 1960 was probably due to the limited number of inpatient beds available at that time rather than a reflection of the actual need. This was supported by the fact that although the number of psychiatric beds increased sharply from 400 beds at the Mental Hospital to 1,000 beds in CPH in 1961, they were very quickly fully occupied.
All the psychiatric inpatients of Castle Peak Hospital, Kowloon Hospital and Lai Chi Kok Hospital in September 1978 were surveyed to collect data in order to plan for the provision of rehabilitation services for the mentally ill (Mental Health Service, 1979). Unfortunately there was no breakdown of the data according to the 3 hospitals and we can only tell that 2,433 (83.3%) of the 2,921 cases were inpatients of Castle Peak Hospital.
Chen (1987) conducted a survey of all the inpatients of Castle Peak Hospital on 8 January 1987 on the diagnoses and and duration of stay with an intention to make suggestions in the classification of the wards. Detailed diagnoses for all non-geriatric cases were recorded. However this was not done for the elderly cases and they were lumped under the category of "psychogeriatric cases" and failed to provide a reference for comparison for the current study. The age distribution of the elderly patients was not reported. But it can be noted that 12 male patients aged under 65 were diagnosed to be suffering from dementia.
In 1987, 5.2% (71) of all male inpatients and 21.3% (150) of all female inpatients belonged to the elderly group. This can be compared with the corresponding figures of 8% (125) and 23% (199) from the current study. From the available data, the average duration of stay for the male elderly patients was 3.59 years and for the female elderly patients 5.17 years. The overeall mean duration of stay was 4.66 years. The mean duration of stay is 6.42 years (± 6.68) for the current study.
Over the years, both the absolute number and proportion of elderly inpatients is noted to be on the rise in Castle Peak Hospital. This is probably also the scene in other psychiatric institutes. Unfortunately there was no breakdown by sex or diagnoses for the earlier data. The patient data computer input used by the Hospital Services Department was not programmed with any updating of age after a patient was admitted to a mental hospital. Subsequent analysis only refer to their age on admission. Hence no useful data was available for meaningful analysis concerning age in the annual statistical reports.
From the present study, 13.5% (324) of inpatients of Castle Peak Hospital were elderly patients in mid 1992. Similarly, about 14% inpatients of Kwai Chung Hospital and up to 50% of the inpatients at Kowloon Hospital Psychiatric Unit and Lai Chi Kok Hospital belonged to the elderly group in late 1992 (Yu & Chung, 1993). This figure may not be easily compare with data in other countries because of the differences in age structure of the population, the quality and quantity of the mental health services and the development of psychogeriatrics. However we cannot rest our minds on this issue just because the local statistics seem moderate when compared to some Western countries.
"MAD-GROWING-OID" OR "OID-GROWINGMAD"?
Lo (1982) commented that the majority of elderly psychiatric patients staying in the mental hospitals were "chronic schizophrenics living to an old age". This statement has been confirmed by the present finding of 70% (226) of the elderly inpatients having their onset of illness before age 65 and 70% of these being schizophrenics. Hence we can definitely conclude that the majority of the elderly inpatients at Castle Peak Hospital are "mad-growing-old" rather than "old-growing-mad" and should fall outside the scope of service by the usual psychogeriatric services. The current study is the only local study looking at the age of onset of mental illnesses in elderly inpatients. More study in this area is warranted.
SEXUAL DIFFERENCE IN AGE OF ONSET
Another interesting finding of the current study is that the female patients are about 5 years older than their male counterparts in the mean age, age on admission as well as the age of onset of mental illness. All these differences are highly statistically significant.
Since there is no significant difference in the duration of admission between the male and female patients, we would certainly like to explain the differences in the mean age and the age on admission by their difference in age of onset of mental illnesses because of the temporal relationship.
It is also very tempting to speculate that since schizophrenia was the most prevalent illness for these patients, the difference in the age of onset may be mainly contributed by the differenct age of onset of schizophrenia between the two sexes reported in psychiatric textbooks (Hare, 1982; Kendell, 1983). Although schizophrenic illness is said to be equally common in male and female, the onset of schizophrenia is found to be on the whole about 5 years later in the female than in the male in several studies (Lindelius, 1970; Noreik & Odegard, 1967). 111e reason for this sex difference in age of onset of schizophrenia is not known despite the obvious theorectical interest. Flor-Henry (1974) had suggested an explanation in terms of different brain maturition in the two sexes but it is not too well accepted.
But speculation is only speculation. When subject to further analysis, it turns out that the age of onset for the male schizophrenics (44.7 years) is not statistically different from the female schizophrenics (47.6 years) (t=0.1325, d.f.= 172, p=0.13). On the other hand, the age of onset for the female dementia is 70.8 years, again about 5 years later than that of the male dementia (65.1 years) at a statistically significant level (t=2.428, d.f.=63, p=0.018). Analysing the mean age and age on admission, the females are highly significantly older than the males for both the schizophrenia and dementia cases. These findings cannot be interpreted easily because we are looking at a long-stay "surviving" sample of all the schizophrenics and dementia. The only comment is that further studies is needed.
IMPLICATION FOR SERVICES
Guidelines laid down by the Royal College of Psychiatrists (Wattis et al, 1987) pointed out that these 2 groups of elderly patients should be served by the general adult services and psychogeriatric services separately in different settings.
With the very limited resources so far vested into the psychogeriatric services and the paucity of trained psychogeriatricians and other professionals, the psychogeriatric services cannot possibly take up all the workload of providing psychiatric services to all mentally ill persons of age 2: 65. Moreover, such a model of service will break the continuity of care to those patients who have grown old with years of general adult services. Therefore mental health professionals should not have unrealistic expectation on the budding psychogeriatric teams such as taking over all existing elderly mental patients. Any subspecialty service will be necessarily expensive and can only focus on a narrowly-defined population. Psychogeriatric teams are set up to develop and guide the services rather than to take over all the load. If all the resources are adequate, the psychogeriatric will at most take over those patients with age of onset 65 and cases with presenile dementia. As seen in Table 7 above, 104 cases will fall into this category. Saying that, any reallocation of these cases should be carely considered as to the possible adverse consqeunces to their physical healthand mental condition.
Another unrealistic expectation on the newly developed psychogeriatric services is that they will eventually reduce the occupancy of mental hospital beds by the elderly patients. As we have discussed previously, as the beds are occupied mostly by the mad-growing-olds, so the psychogeriatric services will not help in their discharge from the hospital. Although psychogeriatric services are being set up with a target of providing psychiatric services in community (DHSS, 1972, 1978, 1985; Health Advisory Service; 1983) a small proportion of the psychogeriatric patients (old-growing-mad) will require inpatient treatment either as short-stay or long-stay at some points of their clinical course. Furthermore, with the early detection and more conprehensive assessment and treatment on mental illnesses in the elderly by the psychogeriatric teams, more utilization of hospital beds by psychogeriatric cases will be expected instead.
On the other hand, the number of elderly mental hospitals "graduate" (mad-growing-old) will nevertheless increases in number and percentage in our mental hospitals if no alternative placement such as long-stay care home or mental infirmary are available. Development of community psychiatric services or rehabilitation services may not provided a full answer to such a rising number of elderly in mental hospitals as they are aiming at different target groups with different goals. Railier, ilie need for services such as long-stay care home and mental infirmary should receive urgent attention and action to cater for the escalating need in the next decade and to improve the overcrowding seen in the mental hospitals.
CONCLUSION
The meager epidemiological data available in Hong Kong has revealed much differences to oilier countries. This may be due to the degree of population migration, the different age structure, the different birth rate, mortality rate, health services and many oilier factors. 111is fact has made thee simple adoption of data obtained from studies in oilier countries on psychogeriatric services unacceptable for services planning in the local setting.
Furthermore, the results of the present study is only looking cross-sectionally at the elderly inpatients in Castle Peak Hospital and differentiating them into the 2 categories served by the general adult services and the psychogeriatric services. We will need further studies in ilie longitudinal course of psychogeriatric patients to provide data such as
the rate of cumulation (annual admissions minus discharges) to assist our prediction of the need of long stay beds in mental hospitals. The only local study in this area to the author's knowledge is the follow up study on 102 new psychogeriatric admissions to Castle Peak Hospital in 1978 reported by Lo (1982). The study showed that within a mean follow-up period of 7.8 months (±10.4), 20 cases (20.6%) had deceased and 29 cases (28.4%) were still in hospital.
Breaking up the psychogeriatric patients into functional mental illness and dementia is also important because they have very different implication on the types of services required (DHSS, 1972; Wattis et al, 1987). As Anderson & Phaterpekar (1991) pointed out, the functional illness would remain more prevalent than the dementia and active psychogeriatric services would generate increased dmand for inpatient treatment for functional illness. It will be a mistake if we underestimte the future demands of functional illness in old age. The administration should have very clear idea and data for the 2 groups before they can carry out any effective planning of psychogeriatric long-stay beds and acute inpatient services for the target population in mind. Hence it is high time that we should build in a surveillance system in the patient data system of the Mental Health Services to keep us agile of the data on the 2 groups: the old-growing-mads and the mad-growing-olds and their changing needs. Repeating similar surveys or following up the subjects of this study may prove rewarding.
Blessed (1988) stated that the number of beds needed to support the severely mentally ill is likely to depend upon on factors including: (1) the nature and relative prevalences of the mental illnesses in a given population; (2) the susceptibility of the mentyal illnesses to psychiatric treatment; (3) the availability of family support; (4) the mean survival time of those occupying the beds and (5) the availability of other effective support systems. These are data that we cannot provide for the local population and services. If we really want to plan ahead for the needs of hospital beds and other aspects of services for the elderly mentally ill, it is high time for researchers and service administrators to start looking for these issues and be prepared to answer them.
ACKNOWLEDGEMENT
My thanks go to all the nursing staff of Castle Peak Hospital for their assistance in surveying the elderly patients in their wards and to Dr. H.K. Cheung, Medical Superintendant, for his permission to carry out this survey.
REFERENCES
Anderson,, D.N. & Phaterpekar, H. (1991) Demand for psychogeriatric services. British Journal of Psychiatry 158: 574 - 575.
Blessed, G. (1988) Long-stay beds for the elderly severly mentally ill. Bulletin of the Royal College of Psychiatrists 12(6): 250 - 252.
Chen, Sylvia (1987) Survey on in-patients of Castle Peak Hospital. (Unpublished report)
DHSS (1972) Services for mental illness related to old age. HMSO, London.
DHSS (1978) A happier old age. HMSO, London.
DHSS (1985) Government response to the second report from the Sociasl Servicea Committee, 1984-85 session. Community care. HMSO, London.
Flor-Henry, P. (1974) Psychosis, neurosis and epilepsy: developmental and gender, related effects and their aetiological contribution. British Journal of Psychiatry 124: 144 - 150.
Hare, E. (1982) Epidemiology of schizophrenia. In Wing, J.K. & Wing, L. (eds) Handbook of Psychiatry Vol. 3. Psychoses of Uncertain Aetiology. Cambridge University Press, Cambridge. p. 42 - 48.
Health Advisory Service (1983) The rising tide. DHSS, London.
Kendell, R.E. (1983) Schizophrenia. In Kendell, RE. & Zeally, AK. (eds) Companion to Psychiatrc Studies (third edition). Churchill Livingston, Edinburg.
Lindelius, R. (1970) A study of schizophrenia. Acta Psychiat. Scand., supp. 216.
Lo, W.H. (1982) Issues in psychiatric care of the elderly in Hong Kong. Journal of Hong Kong Psychiatric Association 2: 6- 9.
Mental Health Service (1979) Survey report on discharge programme plan for psychiatric patients in Castle Peak Hospital, Kowloon Hospital & Lai Chi Kok Hospital. MHD, Hong Kong.
Noreik, K. & Odegard, 0. (1967) Age of onset of schizophrenia in relation to socio-economic factors. British Journal of Social Psychiatry, 1: 243 - 249.
Wattis, J., Neal, D. & Philpott, R. (1987) Guidelines for regional advisers on consultant posts in the psychiatry of old age. Bulletin of the Royal College of Psychiatrists 11: 40 - 242.
Yu, C.S. & Chung, W.S. (1993) Psychogriatrics: The Local Scene and Kwai Chung Hospital Experience. Hong Kong Journal of Gerontology 7: 44 - 47.
T.W. Fan MBBS, MRCPsych, FHKAM(Psych) Senior Medical Of ficer, East Kowloon Psychiatric Clinic, 160, Hammer Hill Road, Diamond Hill, Kowloon, Hong Kong.