Hong Kong J Psychiatry 2004;14(4):9-14
ORIGINAL ARTICLE
SK Kasturiaratchi, PL Jayawardana
Dr SK Kasturiaratchi, MBBS, MSc Community Medicine, Department of Community & Family Medicine, Faculty of Medicine, University of Kelaniya, Sri Lanka.
Dr Pushpa L Jayawardana, MBBS, MSc Community Medicine, MD Community Medicine, Department of Community & Family Medicine, Faculty of Medicine, University of Kelaniya, Sri Lanka.
Address for correspondence: Dr SK Kasturiaratchi, 69/8, Rosmead Place, Colombo 7, Sri Lanka.
E-mail: skkastur@sltnet.lk
Submitted: 3 January 2005; Accepted: 6 April 2005
Abstract
Objective: To describe the physical disabilities and to determine the prevalence of psychologi- cal ill health among permanently disabled servicemen.
Patients and Methods: 430 disabled servicemen were selected by stratified sampling from the 8 regiments of the Sri Lanka army. A self-administered questionnaire was used to collect per- sonal data and details of physical disabilities. The General Health Questionnaire and Bradford Somatic Inventory were used to detect psychological distress and the presence of somatic symptoms, respectively.
Results: Thirty four (8.3%) of the 408 servicemen included in the analysis had more than 1 injury, giving a total of 442 injuries. The two most common disabilities were limb amputation (49.7%) and nerve injury (27.5%). 201 servicemen (49.3%) had a positive General Health Questionnaire result and 119 (29.2%) had a positive Bradford Somatic Inventory result. Of the 119 servicemen positive for Bradford Somatic Inventory, 109 (91.6%) had a positive General Health Questionnaire result (odds ratio, 23.3; 95% confidence interval, 11.2-49.9).
Conclusions: The findings of this study may be useful for the adoption of a holistic approach for rehabilitation of disabled servicemen, and they emphasise the need for early diagnosis and treatment of psychological distress.
Key words: Disabled persons, Military personnel, Stress, psychological
Introduction
The conflict in Sri Lanka during the past 20 years has re- sulted in a large number of young disabled soldiers under- going profound physical and psychological health problems. The psychological problems may be attributed to the phy- sical status, as well as to the traumatic experiences of fighting in a war. Careful assessment of the psychological status of these servicemen is important to ensure long-term benefits of rehabilitation. The determination of factors related to psychological ill health would enable service providers to identify appropriate interventions. Although moderate to severe psychological conditions may be overt, mild conditions often remain undetected. It is therefore necessary to screen for possible psychological ill health. The aim of this study was to describe the physical disabilities and to determine the prevalence of psychological ill health among permanently disabled servicemen.
Patients and Methods
A cross-sectional descriptive study was performed during August 2001. Physically disabled soldiers who had been redeployed were selected from the 8 regiments of the Sri Lanka army, as follows: Sinha (n = 900), Gamunu (n = 1200), Gajaba (n = 1500), Wijayabahu (n = 1200), National Guard (n = 500), Light Infantry (n = 1200), Com- mando (n = 350), and Special Forces (n = 550).
A stratified sampling technique was performed in which each regiment was considered to be a stratum. The number of servicemen was selected using a simple random sampling technique from each stratum, which was propor- tionate to the number of servicemen in each regiment. Only servicemen who had sustained injuries since 1998 (inclusive) were included in the study. The computed sample size was 430.
A self-administered questionnaire with 3 components was used to collect the relevant data. The first component consisted of basic sociodemographic information including age, place of residence, marital status, educational background, and physical disabilities. The second component was the Sinhala version of the 30-item General Health Questionnaire (GHQ), which was used to detect psychological distress. Each question has 4 responses; response numbers 1 and 2 score 0 points and response numbers 3 and 4 score 1 point each. The maximum total score is 30. A score of 5/6 was taken as the cut-off point. The third com- ponent consisted of the Sinhala version of the Bradford Somatic Inventory (BSI), which is a questionnaire used to measure emotional distress characterised by somatic experiences. The BSI consists of 21 questions with 3 responses to each question. Response numbers 1, 2, and 3 score 0, 1, and 2 points, respectively; the maximum score is 42 points. A score of 20/21 was taken as the cut-off point. The GHQ and the BSI have been validated for use in Sri Lanka.1-3
The data analysis was carried out using Epi-Info 2000. The chi-square test was used to determine the association between qualitative variables. A probability value of less than 0.0024 was considered to be significant using the Bonferroni method. Ethical approval to conduct the study was obtained from the Ethics Committee, Faculty of Medicine, University of Kelaniya, Sri Lanka.
Results
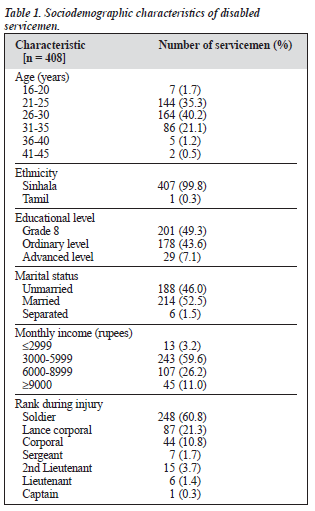
430 disabled soldiers participated in the study. Twenty two questionnaires were incompletely filled in and were excluded from the final analysis. 408 of 430 servicemen (94.9%) were included in the analysis. Table 1 shows their sociodemo- graphic characteristics. 248 servicemen (60.8%) were soldiers at the time of injury. The mean age of the service- men was 27.70 ± 1.95 years (range, 18 to 44 years). All the servicemen were Sinhalese except for one Tamil. There were 399 Buddhists (97.7%), 8 Christians (2.0%), and 1 Hindu (0.3%). Sixty one servicemen (15.0%) were from the Kurunegala district, which was the largest proportion, while none were from the Northern and Eastern Provinces. 201 servicemen (49.3%) had studied up to grade 8; none had received tertiary education. 214 servicemen (52.5%) were married and 188 (46.0%) were unmarried. 243 servicemen (59.6%) had a family income of 3000 to 5999 rupees. 110 servicemen (25.58%) indicated that they were in debt as a result of the injury.
395 servicemen (96.8%) had no history of chronic medi- cal conditions (Table 2). The 6 servicemen (1.5%) with a medical condition had asthma. Twenty three servicemen (5.6%) had a history of a mental illness or had consulted a psychiatrist in the past (Table 2). Fifteen servicemen (3.7%) reported a family history of suicide (Table 2).
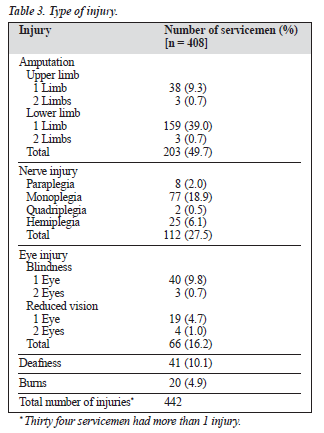
Of the 408 disabled servicemen, 34 (8.3%) had more than 1 injury, making a total of 442 injuries. The most com- mon injury was amputation of a limb (n = 203; 49.7%), and the second most common injury was nerve injury (n = 112; 27.5%) [Table 3]. Of the limb amputations, 162 (39.7%) were of the lower limb. Severity of injury was categorised according to mobility with or without aid. All 408 servicemen were mobile, although 250 (61.3%) required aid (Table 2). 260 servicemen (64.7%) perceived their main problem to have a physical origin, while 130 (31.9%) perceived the problem to be psychological in origin (Table 2). Only 383 servicemen (93.9%) responded to the question about sexual problems, 200 of whom (52.2%) were married. Thirty one servicemen (7.6%) had experienced sexual problems fol- lowing the injury (Table 2). 124 servicemen (30.4%) had increased their alcohol intake since the injury, while 87 (21.3%) had reduced their alcohol intake (Table 2). 104 servicemen (25.5%) had increased their tobacco use since the injury, while 101 (24.8%) had decreased their tobacco use (Table 2).
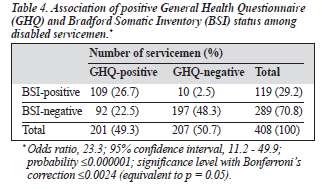
Positive GHQ and BSI scores were observed among 201 (49.3%) and 119 (29.2%) servicemen, respectively. Of the 119 servicemen with positive BSI scores, 109 (91.6%) also had positive GHQ scores. The association between BSI- and GHQ-positive status was statistically significant (odds ratio [OR], 23.3; 95% confidence interval, 11.2 - 49.9) [Table 4]. The BSI had a sensitivity of 54.2% and a specificity of 95.2%, with positive and negative predictive values of 91.2% and 68.2%, respectively.
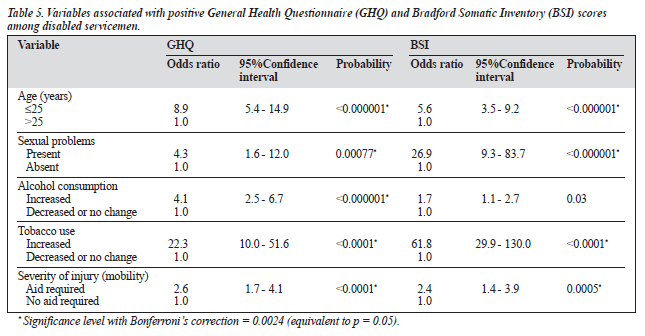
Age (OR, 8.9), experience of sexual problems (OR, 4.3), increased consumption of alcohol (OR, 4.1), increased to- bacco use (OR, 22.3), and severity of injury in terms of mobility with instrumental aid (OR, 2.6) were significantly associated with positive GHQ status (Table 5). Age (OR, 5.6), experience of sexual problems (OR, 26.9), increased tobacco use (OR, 61.8), and severity of injury in terms of mobility with instrumental aid (OR, 2.4) were significantly associ- ated with positive BSI status (Table 5).
Discussion
This study of the psychological status of physically disabled servicemen from the war in Northeast Sri Lanka showed that nearly half of the disabled servicemen (49.3%) had psycho- logical distress (GHQ status) while nearly one-third (29.2%) presented with psychosomatic conditions (BSI status).
Among the Norwegian and Australian war veterans of the United Nations force who served in Lebanon and Somalia, the GHQ-positive status was 5.0% and 24.8%, respectively,4 which was lower than the GHQ-positive sta- tus of the study described here. This low prevalence may be accounted for by the fact that, in both these studies, the ser- vicemen would have comprised healthy and disabled war veterans, unlike in this study, which included only disabled servicemen.
It has been postulated that a large proportion of people with psychological disorders present with somatic symptoms.5,6 However, in this study, 46% of the service- men with a positive GHQ score did not have a positive BSI score, although 92% of servicemen with a positive BSI score also had a positive GHQ score. This latter finding indicates that 92% of servicemen with a positive BSI score are likely to be experiencing psychological distress. Therefore, the GHQ may be recommended as a screening stool for detecting the mental health status of disabled servicemen, rather than the BSI, which has a low sensitivity.
GHQ-positive status was significantly associated with age, experience of sexual problems, increased alcohol and tobacco use, and severity of injury, whereas BSI-positive status was associated with age, experience of sexual problems, increased tobacco use, and severity of injury. However, positive BSI status showed a stronger association for sexual problems (OR, 26.9) and tobacco use (OR, 61.8) than positive GHQ status (ORs, 4.3 and 22.3, respectively).
Age has not been shown to be a significant predictor of psychological morbidity among veterans of the Falklands and Vietnam wars,7 although Weisaeth has shown that young age (younger than 21 years) was associated with post- traumatic psychological morbidity among United Nations military peacekeepers.8 The results of this study are in agree- ment with the results of Weisaeth's study.
It was not possible to show a significant association be- tween psychological status and educational levels of the servicemen as all the servicemen had a similar educational background. The largest group (49.3%) had studied up to grade 8. Only 7.1% of the respondents had successfully completed the Advanced level examinations. Weisaeth showed that a lower IQ is associated with poor psychologi- cal status.8 However, it is possible that the majority of Sri Lankan servicemen did not pursue higher education because of poverty rather than low intelligence.
Marital status was not shown to be a predictor of posi- tive psychological status among veterans of the Falklands war.7 Similarly, the findings of this study did not show an association between marital status and positive GHQ and BSI status. Although it could be anticipated that married individuals are provided with better social support than un- married people, having dependents to support may be a cause of psychological distress.
The rank of the servicemen had no association with the GHQ or BSI status in this study. However, a positive asso- ciation between rank and psychological and physical ill health has been shown in a study of UK veterans of the Gulf war.9 Higher ranking servicemen have a better financial sta- tus than those of lower ranks; therefore, a difference be- tween the 2 groups could be expected. Failure to show an association between rank and psychological ill health in this study may be attributed to the small sample.
The number of servicemen with a history of chronic ill- ness was small in this study. Therefore, an association be- tween positive psychological symptoms and history of chronic illness in the past was not evident. One of the re- cruitment criteria for joining the armed services is physical fitness and lack of chronic illness. Therefore, it is unlikely that there would be many servicemen with a chronic illness at the time of recruitment.
It was shown by Mcfarlane that a history of psychiatric illness is a predictor of psychological status among Austra- lian firefighters.10 However, there was no significant associa- tion between previous psychiatric illness and the presence of psychological symptoms measured by the GHQ or BSI in this study. Only 5.3% of respondents had a history of psychiatric illness, including those who had consulted a psychiatrist but did not have a psychiatric condition diagnosed. It is unlikely that people with a chronic psychi- atric illness would apply to join the armed forces; hence, this result was not surprising.
Weisaeth found that a family history of psychiatric ill- ness has been shown to be associated with the psychologi- cal status of war veterans.8 In the present study, 3.7% had a family history of suicide. It was not possible to show an association between family history of suicide and positive GHQ and BSI status in this study, and this may be attrib- uted to the small number of servicemen in this study. However, Weisaeth's finding highlights the importance of knowing the family psychiatric history of servicemen and the need for close follow-up during highly stressful times. Regular counselling services may be of value for these servicemen.
Sixty five percent of servicemen perceived that their main problem following injury was physical in origin. However, one-third of the servicemen perceived the problem to be psychological. It appears that these servicemen were un- able to come to terms with their disability and were psycho- logically affected. This highlights the need for provision of regular psychiatric reviews and psychological support for injured servicemen. Early detection and treatment of this psychological problem would improve the quality of their lives.
Only 8.1% of the 383 respondents admitted to sexual problems. In a study of Iowan Gulf war veterans, 1.5% of servicemen and 5.1% of female partners had experi- enced sexual discomfort.11 Culturally, sexual problems are not openly discussed in Sri Lanka. The use of the self- administered questionnaire was thought to minimise this inhibition. A significant association was observed between the presence of sexual problems and both GHQ and BSI status. The OR for the BSI revealed a 27-fold greater likelihood of having a positive BSI score when experienc- ing sexual difficulties. These findings are consistent with the study of Iowan Gulf war veterans, which reported a significant association between sexual discomfort and psychological morbidity.
Wards has shown in his study of war veterans that 29.1% of servicemen reported a change in their alcohol con- sumption following exposure to combat.4 Labbate and Snow found that 38% of respondents increased their alcohol consumption.12 In the present study, 30.4% of respondents indicated that their alcohol consumption had increased following their injury; this was significantly associated with a positive GHQ status. A significant association was also evident with tobacco use and both GHQ and BSI status, with an OR of 62 for the association between smoking and BSI-positive status. The significant association for tobacco and alcohol use with psychological morbidity is anticipated since alcohol and smoking are mutually associated behavioural conditions. Drugs and alcohol may be used to obtain solace from mental stress. However, indulgence in alcohol and other drugs may provide only temporary relief, and the harmful effects of dependence are well known. This result highlights the need for early detection of psychologi- cal stress and adoption of appropriate interventions.
Severity of injury categorised according to the ability of an individual to move with or without aid showed a signifi- cant association with positive GHQ status (Table 5). This finding was consistent with the findings of Ravesloot et al whereby the level of physical disability had an association with psychological health status.13 A comparison of disabled and non-disabled Gulf war veterans has also shown that the prevalence of psychiatric disorders for the disabled veter- ans was twice that for the non-disabled veterans.14
Because 59.6% of servicemen had a monthly income of 3000 to 6000 rupees (US$30 to US$60) and 25.6% owed money since the injury, there is a need to improve the finan- cial status of the servicemen. Financial help could be in the form of loan repayment schemes with low interest rates or medical benefit schemes.
Provision of special identity cards, medical camps, medi- cal benefit schemes, educational schemes for offspring, care homes, and vocational training are some of the services avail- able for disabled servicemen in India.15 In Sri Lanka, facili- ties are provided for disabled servicemen who have retired due to permanent disability, but not for servicemen who have been redeployed. All disabled servicemen should be equally provided for irrespective of their retirement status.
Not all stressful factors were included in this study, inclu- ding recall of events during combat. This factor was avoided to prevent precipitating acute psychological distress among vulnerable servicemen, for which event, debriefing sessions would be required. Symptoms related to post-traumatic stress disorder were also not studied. The correlates of psychological morbidity were identified based only on the univariate analysis. When carrying out multiple analyses on a single data set, the likelihood of obtaining a significant association is high. This was overcome by applying the Bonferroni correction, assuming that the maximum num- ber of times the analysis was carried out was 21. Ideally, multivariate analysis, which is helpful for the control of confounding effects, would have been applied. The above- mentioned factors are considered to be limitations of this study. However, since the study is representative of all redeployed disabled servicemen, the ability to generalise the findings to all such servicemen in the country is consid- ered to be a strength of this study.
Health is a combined state of physical, mental, and so- cial well-being. Therefore, the findings of this study may be useful for the adoption of a holistic approach for reha- bilitation of disabled servicemen. Physical and social as- pects of the servicemen's health need to be addressed if mental well-being is to be achieved. The study emphasises the need for early diagnosis and treatment of psychological distress. In addition, providing regular mental health ser- vices and improving servicemen's financial status would increase the quality of these individuals' lives. Whereas the physical status is the responsibility of health care providers, servicemen's social needs should be the responsibility of the government, because these individuals' disability is a direct result of their occupation, which is to protect the state and the interests of its people.
Acknowledgements
Gratitude is expressed to the Ministry of Defence for grant- ing permission to carry out this research, all the servicemen who willingly participated, and all other army personnel who assisted in making this study a success. A special word of thanks is extended to Dr A Sumathipala for his guidance and Dr S Warusavithana for her cooperation throughout the study.
References
- De Silva N, Samarasinghe D. Acceptance of psychiatric screening: Questionnaire by general practice attenders. Ceylon Med J 1990;35: 105-108.
- Sumathipala A, Hewege S, Hanwella R, Mann AH. Randomized con- trolled trials of cognitive behaviour therapy for repeated consultations for medically unexplained complaints: a feasibility study in Sri Lanka. Psychol Med 2000;30:747-757.
- Sumathipala A, Murray J. New approach to translating instruments for cross cultural research: a combined qualitative and quantitative approach for translation and consensus generation. Int J Methods Psychiatr Res 1999;9:87-95.
- Wards W. Psychiatric morbidity in veterans of the United Nations peace- keeping force in Somalia. Aust NZ J Psychiatry 1997;31:184-193.
- Simon GE, Vonkorff M, Piccinelli M, et al. An international study of the relation between somatic symptoms and depression. New Engl J Med 1999;341:1329-1335.
- Mumford DB, Bavington JT, Bhatnagar KS, Hussain Y, Mirza S, Naraghi MM. The Bradford Somatic Inventory. A multi-ethnic inven- tory of somatic symptoms reported by anxious and depressed patients in Britain and the Indo-Pakistan subcontinent. Br J Psychiatry 1991; 158:379-386.
- O'Brien LS, Hughes SJ. Symptoms of post traumatic stress disorder in Falkland veterans five years later the conflict. Br J Psychiatry 1991; 164:443-447.
- Weisaeth L. Stress of UN military peacekeeping, World Veteran Foundation. International Socio-Medical Information Center Newslet- ter 1990;2:15-18.
- Ismail K, Blatchley N, Hotopf M, et al. Occupational risk factors for ill health in Gulf veterans of the United Kingdom. J Epidemiol Commu- nity Health 2000;54:834-838.
- Macfarlane AC. The aetiology of posttraumatic morbidity: predisposing, precipitating and perpetuating factors. Br J Psychiatry 1989;154: 221-228.
- The Iowa Persian Gulf Study Group. Self-reported illness and health status among Gulf War Veterans. A population based study. JAMA 1997; 277:238-245.
- Labbate LA, Snow MP. Posttraumatic stress symptoms among soldiers exposed to combat in the Persian Gulf. Hosp Community Psychiatry 1992;43:831-833.
- Ravesloot C, Seekins T, Young QR. Health promotion for people with chronic illness and physical disabilities: the connection between health psychology and disability prevention. Clin Psychol Psychother 1998; 5:76-85.
- Ismail K, Kent K, Brugha T, et al. The mental health of UK Gulf war veterans: phase 2 of a two phase cohort study. Br Med J 2000;325:576.
- Indian Army. Welfare activities. http://indianarmy.nic.in/arwelf3.htm
Call for Papers
The Hong Kong Journal of Psychiatry invites authors to submit manuscripts on subjects relating to clinical practice and research in the specialty of psychiatry and in related disciplines. The Journal publishes Original Articles, Review Articles, Case Reports, Book Reviews, and Letters to the Editor.
Interested authors should refer and adhere to the Journal's Instructions for Authors, included in this issue and available online (at www.hkjpsych.com). All manuscripts submitted for publication will be assessed by peer review, and acceptance of any paper cannot be guaranteed.
Manuscripts should be sent to: The Chief Editor, Hong Kong Journal of Psychiatry, c/o Department of Psychiatry, Queen Mary Hospital, Pokfulam Road, Hong Kong, China (E-mail: admin@hkjpsych.com).
The Hong Kong Journal of Psychiatry is indexed in EMBASE/Excerpta Medica and PsycINFO, and can be accessed online at www.hkjpsych.com.