Hong Kong J Psychiatry 2004;14(3):7-14
ORIGINAL ARTICLE
Dr Ghassemi Gholam Reza, PhD, Behavioural Sciences Research Centre, Isfahan University of Medical Sciences, Isfahan, Iran.
Dr Mallik Shikha, PhD, Zenderood Clinic of Social Work, Isfahan, Iran. Dr Taban Habibollah, MD, School of Medicine, Isfahan University of Medical Sciences, Isfahan, Iran.
Dr Assadollahi Ghorban Ali, MD, Department of Psychiatry, School of Medicine, Isfahan University of Medical Sciences, Isfahan, Iran.
Address for correspondence: Dr Ghassemi Gholam Reza, PO Box 81465-819, Isfahan, Iran. E-mail: ghassemi@med.mui.ac.ir
Submitted: 15 August 2003; Accepted: 7 September 2004
Abstract
Objective:To study the effectiveness of a family psychoeducational programme for social adjustment of individuals with schizophrenia and mood disorders and to determine whether the intervention had an impact on the family dynamics and caregivers’ knowledge and experiences.
Patients and Methods:Using Solomon’s experimental design, 170 patients with schizophrenia and 174 patients with the diagnosis of mood disorders were assigned to 2 experimental and 2 control groups. Family members from the experimental groups participated in a weekly educational programme for 6 months. Tests were used to determine and compare family charac-teristics and social adjustment of patients at baseline and after 6 and 18 months.
Results: More attitudinal, cognitive, and behavioural changes among families and enhanced performance abilities were observed among patients from the experimental groups.
Conclusions: These observations reinforce the hypothesis that a cognitive-behavioural programme changes family dynamics in favour of patients with severe psychiatric disturbances, especially for their adjustment in the family and community.
Key words: Family, Mood disorders, Schizophrenia, Social adjustment
Introduction
The presence of a mentally ill patient in the home imposes several limitations on the family such as social burden, financial strain, and psychological stress.1-5 The family dynamics may be affected, and tolerance of the patient may be reduced. Several studies have focused on families’ responses to mental illness and living with a mentally ill family member, resulting in several promising clinical approaches.6-16 Liberman and Corrigan introduced tech-niques for interpersonal problem solving therapy for the better social adjustment of people with schizophrenia.17 It has been observed that relapse rates of mentally ill patients after discharge are significantly lower for those patients whose families were exposed to behavioural interventions than for those who received routine treatment.18 Similarly, family therapy and group therapy techniques have reduced the levels of overinvolvement, hostility, and criticism in the family, reducing relapse rates.19 Some authors have claimed that family intervention can help to reduce patients’ nega-tive and positive symptoms.20 In addition, improvement of family communication has been associated with desirable changes in patients’ interpersonal functioning.21
Family education and family therapy have a promis-ing role in minimising the relapse rates of mentally ill patients.22,23 An evaluation of a family psychoeducation programme by de Groot et al has determined the positive role of family intervention in increasing people’s knowl-edge and understanding of mental health services in the community.24 Family intervention for dual disorders not only improved the course of the illness for patients with psychiatric disorders and substance abuse but also promoted collaboration between their families and professionals.25 Montero et al compared the impact of 2 family intervention strategies on families of patients with schizophrenia in a Mediterranean environment, which yielded equally significant results for the outcome of the illness.26
An attempt has been made by Pollio et al to bring to-gether mentally ill people and their family members with the intention of sharing their experiences and ameliorating their problems.27 Participants in this programme expressed satisfaction with learning different coping strategies and problem-solving skills. Cassidy et al predicted fewer days of hospitalisation for patients with schizophrenia whose relatives attended a family psychoeducation programme, as well as significant attitudinal and cognitive changes in their families and improved knowledge about their medication.28 Hospital staff who underwent a training course on cogni-tive behavioural family intervention knew more about family dynamics and demonstrated more regular inclusion of family members in their routine clinical practice after training.29 These researchers reported that this intervention reduced the family burden. However, McDonell et al’s study did not bring about significant changes in the family burden for those who underwent multiple family group treatment compared with those families who received standard care.30 To enhance the patients’ compliance, some authors have prescribed complex intervention methods that combine information, counselling, reminders, self-monitoring, reinforcement, and family therapy.31
During the past 2 decades, Iranian society has under-gone several upheavals, resulting in the emergence of new social institutions. International and national movements have influenced the overall approach to mental illness and shaping of the Iranian mental health policy (IMHP). Em-phasis on promotion of mental health, clarity of referral system, and demarcation of 3 levels of intervention are the main features of the IMHP.32 The IMHP also recognises the needs of disadvantaged groups and focuses on integration of mental health into the general health programme in both rural and urban areas.33,34 With the emphasis on deinstitut-ionalisation and community-oriented methods, sporadic attempts have been made to determine the efficacy of cog-nitive behavioural methods for helping families of mentally ill patients.35 In practice, research findings have helped in designing innovative intervention methods based on team-work and interdisciplinary approaches.36,37 Nonetheless, in the Iranian context, systematic data to support these hypoth-eses are lacking and management of patients’ verbal and non-verbal behaviours remains a problem for their families and the presence of mentally ill patients in the community continues to be a challenge for policymakers and mental health professionals. In view of the existing gap in know-ledge, this study examined the effectiveness of a family psychoeducational programme for the social adjustment of individuals with psychiatric disorders, and determined the impact on the family dynamics and caregiving skills.
Patients and Methods
Solomon’s experimental design was adopted as the research tool to test the hypotheses with greater confidence and mini-mum influence of confounding variables.38 Adhering to Solomon’s research formula, each diagnostic category (schizophrenia and mood disorders) comprised 2 experimen-tal and 2 control groups. Subsequently, every experimental and control group was further divided into 2 subgroups: 1 with pretest and post-test and the other without pretest and with post-test. The main variables in this study included ‘family functioning’, ‘attitude towards mentally ill patients’, ‘skills in management of the patient’, and ‘patient’s social adjustment’.
The participants were psychiatric patients discharged from 2 major psychiatric centres in Isfahan, Iran, between September and November 1998, who were followed up from January 1999 to March 2000. The study group comprised 170 patients with schizophrenia and 174 with mood disorders. Forty five patients with schizophrenia were as-signed to the experimental group with pretest and 42 were assigned to the experimental group with only the post-test. The control group for the pretest group for the same diag-nostic category had 43 patients and the control group for post-test only had 40 patients. For patients with mood disorders, the experimental group with pretest contained 44 patients and the experimental group with post-test only had 43 patients The control group for the same diagnostic cate-gory with pretest included 44 patients and the control group for post-test only included 43 patients. All patients were randomly selected and assigned to their respective subgroups. Patients were matched for type of disorder, relapse rate, frequency of admission to hospital, age, and sex. All patients received psychiatric treatment from 2 senior psychiatrists as outpatients. The main eligibility for the key family members were willingness to participate in the study, ability to read and write, living with the patient, playing a key role in decision-making regarding the patient’s treatment, and providing necessary support for the patient. None of the key family members had any psychiatric dis-order or a history of mental illness.
Five investigators with a nursing background underwent special training for 1 month and were employed for data collection. While paying home visits and establishing rap-port with the families, they interviewed the key family members. None of the investigators were involved in the intervention programme. Psychiatric medication was adminstered by 2 senior psychiatrists while the family edu-cation programme was carried out by a clinical social worker and a psychiatric nurse.
Tests measuring the main variables were administered to key family members of the exerimental and control groups. The family atmosphere was determined by Bloom’s Family Functioning Scale (FFS).39 This instrument contains 75 items that measure 15 aspects of family functioning. Participants’ responses to each item were rated on the basis of Likert’s 5-point scale. The score for each item ranged from 0 to 4, while a respondent’s score ranged between 0 and 300 overall for the 75 items. The reliability of the FFS was established by a test-retest method among 40 families who were not included in the study, yielding a Cronbach
value of 0.76. Family’s Attitude Towards Mentally Ill (FAM), a self-developed index with 30 items, was used to determine the families’ attitudes towards their relative. The respondent could answer each question by saying ‘Yes’ or ‘No’. The score for each item was 0 or 1, while the overall score for the 30 items ranged from 0 to 30. This index was tested for validity using the content method. For this purpose, 42 statements were prepared and distributed among 12 psychiatrists, 5 clinical psychologists, and 2 social workers. After several revisions, the panel reached consensus on 30 items, which were administered to 52 families who were not included in the study. The Cronbach ά value yielded patient from the test-retest method was 0.73, which is significant and acceptable.
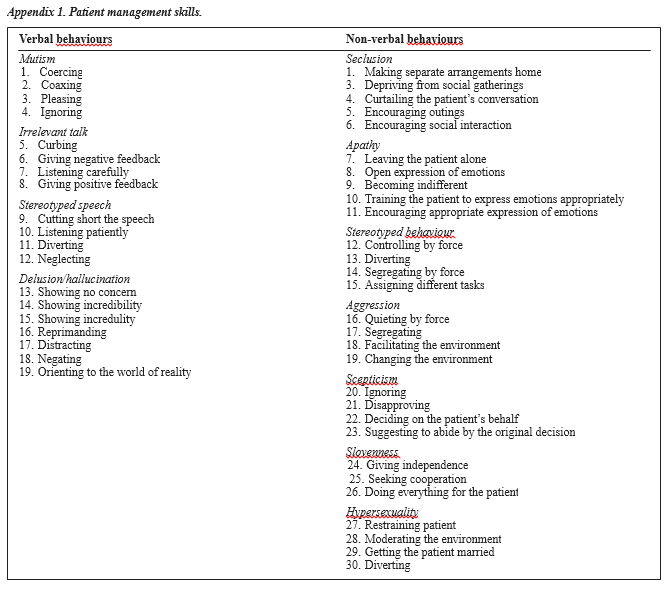
Families’ skills in managing their relatives was deter-mined by the Patient Management Skills Index (PMSI). This self-developed index contained 49 items, of which 19 items measured skills in managing a relative’s verbal behaviours and the remaining 30 items measured skills in managing their relative’s non-verbal behaviours. The responses to each item could be in 2 forms, namely ‘applicable’ and ‘not applicable’. While the score for each item ranged from 0 to 1, the participant’s overall score for items pertaining to verbal behaviours ranged from 0 to 19 and 0 to 39 for non-verbal behaviours. Overall scores for this index ranged from 0 to 49. Higher scores indicated a respondent’s skill in man-aging their relative.
Initially, the PMSI consisted of 52 items, which was tested for validity using the content method. A panel of 12 senior psychiatrists, 3 psychiatric nurses, and 4 social workers approved the content of this instrument. The expert committee reviewed the 52 statements and reached con-sensus for 49 items. The reliability of this insturment was established by the test-retest method among a group of 40 families, yielding a Cronbach ά value of 0.89. The potential of this instrument has been demonstrated in community studies and it is extensively used as part of a training programme in Iranian community mental health centres.37 Appendix 1 explains this instrument in detail. Patients’ social functioning was viewed as the major depen-dent variable in this study. A revised version of Weissman’s Social Adjustment Scale (SAS) with 41 items measuring an individual’s level of functioning for various areas, includ-ing work, home, school, and community was used for this study.40 Responses to each item were rated on the basis of Likert’s 5-point scale. The reliability of the SAS was estab-lished by the test-retest method for 60 patients, yielding a Cronbach ά value of 0.82.
The training course for the families was based on a curriculum that was conducted biweekly for 6 months. The subject matter in this package pertained to the nature of the mental illness, its probable causes, associated symptoms, patients’ psychosocial needs, basic skills in managing a patient’s behaviour, implications of a disturbed family environment, and the importance of medication. The ma-terial was drawn from psychiatric texts and clinical experi-ence.1,14,41,42 Every effort was made to prepare the materials in simple language, which was easily understood by patients and their families. By means of lectures, group discussion, and case illustrations, the trainers demonstrated the neces-sary skills for the management of a patient’s verbal and non-verbal behaviours. The first session was allocated to mental illness, its causes and symptoms, and the implications for interpersonal relationships within the family. The partici-pants had the opportunity to explain their concepts of men-tal illness and describe typical symptoms of their relatives. Pretest assessment was made by the investigators using specific devices. During the second workshop, verbal and non-verbal symptoms and behaviours of a typical patient with psychosis were described. The participants were in-volved in sharing their experiences. Five workshops were conducted in which several issues such as patients’ self-care, general feelings and emotions, delusions, hallucinations, speech disturbances, stereotyped behaviour, aggressive behaviours, and impulsive behaviour and sexual urges were discussed. The third and fourth workshops were specifically devoted to learning skills, including rapport building with patients and management of inappropriate mood, stereotyped behaviour, aggressive behaviour, self-care, and impulsive behaviours. In the final workshop, using case illustrations the participants demonstrated their ability to manage their relatives’ behaviours. The trained investigators made post-test assessment by administering their evaluation criteria for the key family members. No family members dropped out of the study.
The completed interview schedules were reviewed and prepared for data entry. The data were analysed using the Statistical Package for the Social Sciences. Frequency per-centages and measures of central tendency, including mean, skewness, and standard deviation, were calculated by means of descriptive analysis. Analysis of variance (ANOVA) and t-paired test were used for significance for the dependent variables
Results
The patients’ ages ranged from 25 to 29 years. The average age for patients with schizophrenia was 27.35 ± 6.05 years and 23.92 ± 4.26 years for those with mood disorders. Nearly 52% of patients with schizophrenia and 64% of patients with mood disorders were women. Most of the women were housewives. The patients lived with their families. Most patients were educated to primary level, were unmarried, had an illness duration of less than 1 year, had been admitted to hospital once or twice, and had never attempted suicide.
Patients’ Family Environment
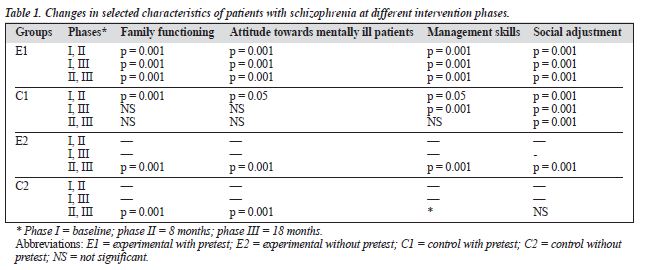
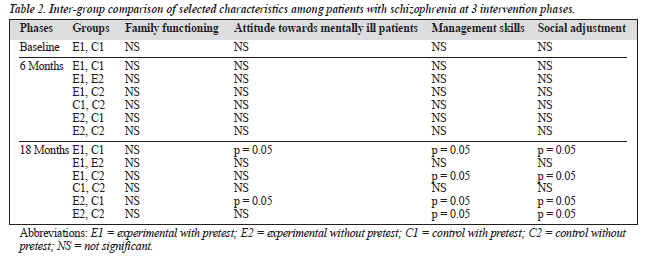
Comparison of family functioning scores of patients with schizophrenia showed significant changes for the experi-mental group with pretest (E1) at each successive phase, between the first and second phase for the control group with pretest (C1), and between second and third phases for the experimental (E2) and control (C2) groups without pretest (Table 1). Family functioning scores between the experimental and control groups did not change significantly after 8 and 18 months of follow-up (Table 2).
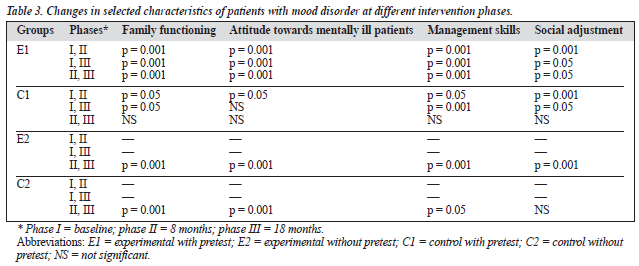
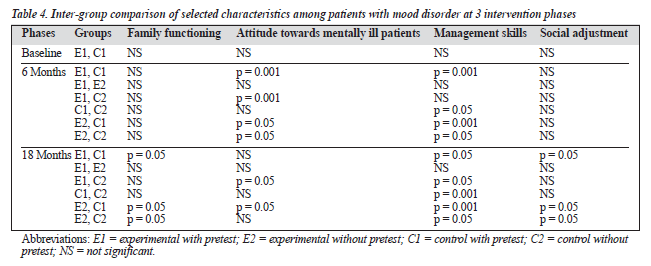
Comparison of family functioning scores for patients with mood disorder also showed significant changes for the E1 group at each successive phase, between the first and second phases between the first and third phases for the C1 group, and between the second and third phases for the E2 and C2 groups (Table 3). Additionally, comparison of family functioning scores between the experimental and control groups showed significant differences between E1 and C1, E2 and C1, and E2 and C2 after 18 months of follow-up. However, no significant change was observed after 8 months of follow-up (Table 4).
Attitudes of Families Towards Patients
Attitudes of families towards patients with schizophrenia changed for the E1 group at each successive phase, between the first and third phases for the C1 group, and between the second and third phases for the E2 and C2 groups (Table 1). Attitude scores between the experimental and control groups showed significant differences between E1 and C1, E1 and E2, and E1 and C2 after 18 months of follow-up. No attitudinal change was observed after 8 months of follow-up (Table 2). Attitude scores for families of patients with mood disor-
der showed significant changes for the E1 group at each successive phase, between the first and second phases for the C1 group, and between the second and third phases for the E2 and C2 groups (Table 3). Families’ attitudes towards the patients showed significant differences between E1 and C1, C1 and C2, E2 and C1, and E2 and C2 after 6 months of follow-up. The attitude of family members after 18 months of follow-up showed significant differences for the control group (Table 4).
Families’ Management Skills
As indicated in Table 1, family management scores for pa-tients with schizophrenia showed significant changes for the E1 group at each successive phase, between the first and second, and first and third phases for the C1 group, and between the second and third phases for the E2 and C2 groups. As indicated in Table 4, after 18 months of follow-up, families’ management skills for the experimental and control groups showed significant differences between E1 and C1, E1 and E2, E1 and C2, and C1 and C2. No signifi-cant change was noted in the management skills of these families after 8 months (Table 4).
Comparison of family management scores for patients with mood disorder showed significant changes for the E1 group at each successive phase, between the first and second, first and third phases, and second and third phases for the C1 group, and between the second and third phases for the E2 and C2 groups (Table 3). Comparison of family man-agement scores between the experimental and control groups showed significant differences between E1 and C1, C1 and C2, E2 and C1, and E2 and C2 after 8 months. Significant changes were also observed after 18 months of follow-up between E1 and C1, E1 and C2, C1 and C2, E2 and C1, and E2 and C2 (Table 4).
Social Adjustment of Patients
Comparison of social adjustment scores for patients with schizophrenia also showed significant changes for the E1 and C1 groups, as well as the E2 group at each successive phase. However, no significant change was observed for the C2 group (Table 1). No significant change was observed in the social adjustment of patients with schizophrenia after 8 months of follow-up. However, significant changes were seen in the social adjustment between E1 and C1, E1 and E2, E1 and C2, and C1 and C2 after 18 months of follow-up (Table 2).
Analysis of data pertaining to social adjustment scores of patients with mood disorder showed significant changes for the E1 group at each successive phase and between the first and second, and first and third phases for the C1 group. Significant changes were observed in the E2 group at the second and third phases of intervention (Table 3). No sig-nificant changes were observed in the social adjustment scores of patients with mood disorder after 8 months while social adjustment scores for patients in this category changed after 18 months of follow-up between E1 and C1, E2 and C1, and E2 and C2 (Table 4).
Discussion
This study investigated attitudinal and behavioural changes in the family dynamic of patients with psychiatric disorders. The ultimate aim was to describe the impact of a family psychoducational programme on the social adjustment of patients with schizophrenia and mood disorder. By expos-ing families of mentally ill patients to a training programme, they have been helped to reduce the burden of the disease and to learn basic skills to manage patients’ verbal and non-verbal behaviours.
Solomon’s experimental design has been engineered to manipulate the phenomenon and present the research find-ings with greater confidence. In this study, the units of analy-sis were the families and individuals who were classified as experimental and control groups with pretest and without pretest. Inter- and intra-comparisons of families and patients were made across several features, including family func-tioning, attitudes towards mentally ill patients, management skills, and patient’s social adjustment. Different statistical methods were used to highlight the changes that occurred as a result of intervention.
Analysis of the data indicates that with successive phases of intervention, families became more functional and tolerant. This trend was more prominent for families of pa-tients with mood disorder than for those with schizophrenia (Tables 1 to 4). These differences could partly be attributed to the family environment of patients with schizophrenia, characterised by high expressed emotion, disengagement, and poor locus of control.11,12,14 This observation serves as a warning for mental health professionals to be sensitive to families of patients with schizophrenia. While observing a strong association between family adversity and levels of psychiatric symptomatology, Goebert et al advocated rou-tine assessment of family environment and family-oriented interventions.6 Change in the family environment may be partly attributed to the efficacy of this intervention programme and partly to the duration of illness. A compre-hensive review of psychiatric research into schizophrenia by Penn and Muser led to the conclusion that family educa-tion is highly effective for reducing families’ expressed emotion.43 Long duration of illness has been associated with positive communication among families of patients with schizophrenia.8 Pollio et al believe that family psycho-educational programmes help families to become cohesive and make the family environment more conducive for its members.27 It is also argued that the trauma of mental illness often induces families to revise their function and interactions.44
The presence of an individual with mental illness in the family is difficult. Many families feel shameful and guilty, and consider themselves removed from mainstream society.5 With this knowledge, this study was designed to induce attitudinal changes in families through education. Interestingly, analysis of the data showed that families’ atti-tudes became more favourable over time. This change may be an indicator for acceptance of the illness by the family, and may also show how families have resigned themselves to the situation. However, this change may be partly attrib-uted to the emotional and social components of the training programme, with its dual role of reducing social burden and increasing the families’ social involvement. The programme also aimed to increase the knowledge base of families to-wards better understanding of the phenomenon of mental illness and acceptance of mentally ill patients at home. Magliano et al reported that the attitude of the family to-wards the patient changes with time and their communica-tion becomes more effective.8 While describing the poten-tial of a psychoeducational model, Pollio et al concluded that families tend to change their attitudes and cope with an undesirable situation.27 The findings of Cassidy et al are also in line with the present observations and reinforce the belief that psychoeducational intervention is accompanied by cognitive and attitudinal changes in the family.28 Laube and Highson have demonstrated the efficacy of cognitive behavioural family education in inculcating positive attitudes of families towards mentally ill patients.29 The cur-rent observations are reinforced by the earlier findings of Brooker et al,20 Atwood,22 Birchwood et al,23 and Fowler41 who attributed attitudinal changes among families to family psychoeducational programmes.
While researchers have focused on the disabling nature of severe mental disorders2,45 some have studied the extent of the family burden and its implicaions for psychiatric symptomatology.4-6,46-48 In this study, families were exposed to a training programme to learn the necessary skills for the management of patients’ non-verbal and verbal behaviours. This training programme aimed to ameliorate the pathologi-cal interaction styles that act as obstacles to the treatment process. Analysis of the data indicated that at every succes-sive phase, families gained more confidence and became more independent in managing their relatives at home. It was observed that the majority of the patients visited the psychiatric outpatient department on their own. This change may be attributed to the community-based approach of this study, which was experienced by Magliano et al.49 Their study of obsessive compulsive disorder showed progressive involvement of families caring for patients, with the shift from hospital-based to community-oriented management.49 Penn and Muser hold the view that expressed emotion in families reduces in direct proportion to the family educa-tional level.43 It is also possible that families’ knowledge levels increase and they learn the necessary skills for the management of their relatives. This observation is similar to the reports of Cassidy et al28 and Laube and Highson29 of using a psychoeducational programme to improve relatives’ knowledge about schizophrenia.28,29
Severe psychiatric illness affects role performance and, with family overinvolvement and criticism, a patient’s chances of adjustment decline. In this respect, several studies show the implications of critical comments and emo-tional overinvolvement on part of the family for social ad-justment of patients in the community.0,50,51 The findings of this study also show significant changes in the overall per-formance of those patients whose families participated in the training programme. In other words with every succes-sive phase of intervention, families expressed more satis-faction about the patients’ role in the home, school, college, and community. These observations are supported by sev-eral other studies. Magliano et al have argued that social involvement of the patient is subject to the family’s positive outlook towards the illness and effecive communication with the patient.8 In support of this hypothesis, Penn and Muser believe that family education is highly effective in improv-ing patients’ relapse rates and outcomes.43 Family interven-tion is also effective for reducing the chances of patients being readmitted to hospital.28 Glynn et al’s study of the effects of skills training for outpatients with schizophrenia also led to significant improvements in role functioning, social relationships, and overall adjustment.52 The findings of this study complement previous observations and provide a new platform for future research in the Iranian context.
In conclusion, the findings of this sudy show that attitudinal, cognitive, and behavioural elements conjointly influence the process of an individual’s role performance and social adjustment. The triangle of family dynamics, at-titudes towards mentally ill people, and skills in manage-ment of patients’ behaviours appear to have a dominant role in the outcome of the illness. The findings of this study have implications for health policy, delivery of mental health services in the community, and health system research. To induce families to become responsible caretakers, it is essential to remove their biases and misconceptions about mental illness and the behaviour of mentally ill patients in the home. This involves mutual participation of family and clinicians in activities that are beneficial for the patient. Undertaking training programmes for families of mentally ill people, when supplemented with psychiatric medication, can ensure a better outcome for patients with a psychiatric illness. Based on professional experiences and research findings, several researchers have emphasised routine imple-mentation of family-oriented interventions9,10 and commu-nity-based programmes.29,52,53 In view of cultural diversity, the financial cost of mental illness, and lack of resources, Iranian society needs multi-dimensional mental health mod-els that are based in the community and encourage people’s participation in the health delivery system. Community mental health will play a dual role of removing social stigma and democratising the delivery of services.54
References
- Sadock BJ, Sadock VA, editors. Synopsis of psychiatry. 8th ed. New York: Williams & Willkins; 2003:456-491.
- Lay B, Blanz B, Hartmann M, Scmidt MH. The psychosocial outcome of adolescent-onset of schizophenia: a 12-year followup. Schizophr Bull 2000;26:801-816.
- Schlosberg A. Psychiatric stigma and mental health professionals. Med Law 1993;12:409-416.
- Robertson HA, Kutcher SP, Bird D, Grasswick L. Impact of early onset bipolar disorder on family functioning: adolescents’ perceptions of family dynamics, communication and problems. J Affect Dis 2001; 66:25-37.
- Heru AM. Family functioning, burden, and reward in the caregiving for chronic mental. Ill Fam Syst Health 2000;18:91-103.
- Goebert D, Nahulu L, Nishinuma E, et al. Cumulative effects of family environment on psychiatric symptomatology among multiethnic adolescents. J Adolesc Health 2000;27:34-42.
- Hogarty GE, Anderson CM, Reiss DJ, et al. Family psychoeducation, social skills training and maintenance chemotherapy in the aftercare treatment of schizophrenia: two-year effects of a controlled study on relapse and adjustment, environmental-personal indicators in the course of schizophrenia (BPICS) research group. Arch Gen Psychiatry 1991; 48:340-347.
- Magliano L, Veltro F, Guarneri M, Marasco C. Clinical and socio-demographic correlates of coping strategies in relatives of schizophrenic patients. Eur Psychiatry 1995;10:155-158.
- Laidlaw TM, Coverdale JH, Falloon IR, Kydd RR. Caregivers’ stresses when living together or apart from patients with chronic schizophrenia. Community Ment Health J 2002;38:303-310.
- Dixon L, Adams C, Lucksted A. Update on family psychoeducation for schizophrenia. Schizophr Bull 2000;26:5-20.
- Vaughn CE, Leff JP. The influence of family and social factors on the course of psychiatric illness. A comparison of schizophrenics and de-pressed neurotic patients. Br J Psychiatry 1976;129:125-137.
- Leff JP, Vaughn C. The role of maintenance therapy and relatives’ ex-pressed emotion in relapse of schizophrenia: a two-year followup. Br J Psychiatry 1981;139:102-104.
- Bhugra D, McKenzie K. Expressed emotion across cultures. Adv Psychiatr Treat 2003;9:342-348.
- Ghassemi GhR. Schizophrenics and the family. Bombay: Tata Insti-tute of Social Sciences; 1992:120-125.
- Velligan DI, Miller AL, Eckert SL, et al. The relationship between pa-rental communication deviance and relapse in schizophrenic patients in the 1-year period after hospital discharge: a pilot study. J Nerv Ment Dis 1996;184:490-496.
- Leff J, Dayson D, Gooch C, Thornicroff G, Wills W. Quality of life of long stay patients discharged from two psychiatric institutions. Psychiatr Serv 1996;47:62-67.
- Liberman RP, Corrigan PW. Designing new psychosocial treatment for schizophrenia. Psychiatry 1993;56:238-249.
- Tarrier N, Barrowclough C, Vaughn C, et al. Community management of schizophrenia: a two-year follow up of a behavioural intervention with families. Br J Psychiatry 1989;154:625-628.
- Leff JP, Berkowitz R, Shavit N, Strachan A, Glass I, Vaughn C. A trial of family therapy versus a relatives group for schizophrenia. Br J Psychiatry 1989;154:58-66.
- Brooker C, Falloon I, Butterworth A, Goldberg D, Graham-Hole V, Hillier V. The outcome of training community psychiatric nurses to deliver psychosocial intervention. Br J Psychiatry 1994;165:222-230.
- Greer LA, Weerasekar P, Linder B, Goldberg JO. Use communication skills training for schizophrenia. Can J Psychiatry 1997;42:666-667.
- Atwood N. Integrating individual and family treatment for outpatients vulnerable to psychosis. Am J Psychother 1990;44:247-255.
- Birchwood M, Smith J, Coohrance R. Specific and non specific effedts of educational intervention for family living with schizophrenia. Br J Psychiatry 1992;157:853-859.
- De Groot L, Lioyd C, King R. An evaluation of a family psycho-education program in community mental health. Psychiatr Rehab J 2003;27:18-23.
- Muser KT, Fox L. A family intervention programme for dual disorders. Community Ment Health J 2002;38:253-270.
- Montero I, Asencio A, Hernandez I, et al. Two strategies for family intervention in schizophrenia: a randomized trial in a Mediterranean environment. Schizophr Bull 2001;27:661-670.
- Pollio DE, North CS, Osborne V, Kap N, Foster DA. The impact of psychiatric diagnosis and family system relationship on problems iden-tified by families coping with a mentally ill member. Fam Proc 2001; 40:199-209.
- Cassidy E, Hills G, Callaghan E. Efficiency of a psychoeducational intervention in improving relatives’ knowledge about schizophrenia and reducing rehospitalization. Eur Psychiatry 2001;16:446-450.
- Laube RE, Highson FM. Staff training in cognitive-behavioral family intervention in mental illness using the multiple-family group approach: a pilot study. Community Ment Health J 2000;36:477-490.
- McDonell MG, Short RA, Berry CM, Dyck DG. Burden in schizo-phrenia caregivers: impact of family psychoeducation and awareness of patient suicidality. Fam Proc 2003;42:91-103.
- McDonald HP, Grag AX, Haynes RB. Interventions to enhance patient adherence to medication prescriptions. JAMA 2002;288:2868-2879.
- National Mental Health Committee. Iranian mental health policy.Tehran: Ministry of Health, Treatment and Medical Education; 1982:4-8.
- Shahmohamadi D. Integration of mental health in primary health care in Sharekurd, Iran. Tehran: Ministry of Health, Treatment and Medical Education; 1989:2-12.
- Ghassemi GR, Asadollahi GhA. Integration of mental health in urban health system. Isfahan: Isfahan University of Medical Education and Health Services; 2003:1-15.
- Asadollahi GA, Ghassemi GhR, Mehrabi T. Training families to better manage schizophrenics’ behaviour. East Med Health J 2000;6:118-127
- Ghassemi GR. Isfahan child guidance clinic schema. Isfahan: Isfahan University of Medical Sciences and Health Services; 1985:4-9.
- Ghassemi G Community mental health model. Isfahan: Isfahan Uni-versity of Medical Sciences and Health Services; 1986:3-9.
- Campbell DT, Stanley JC. Experimental and quasi experimental de-signs for research. Palo Alto: Hougron Mifflin Company; 1966:35-46.
- Bloom M. A factor analysis of self report measures of family functioning. Fam Proc 1980;24:225-239.
- Weissman MM, Prusoff BA. Social adjustment hadbook: rationale, reliability, validity, scoring and training guide. California: California University; 1987:1-44.
- Fowler Family psychoeducation: chronic psychiatrically ill Carib-bean patients. J Psychosoc Nurs Ment Health Serv 1992;30:27-32.
- Anderson CM, Reiss DJ, Hogarty GE. Schizophrenia in the family: a guide to education and management. New York: Guilford Press; 1986:25-68.
- Penn DL, Muser KT. Research update on the psychosocial treatment of schizohrenia. Am J Psychiatry 1996;153:607-617.
- Robertson HA, Kutcher SP, Bird D, Grasswick L. Impact of early onset bipolar disorder of family functioning: adolescents’ perceptions of family dynamics, communication, and problems. J Affect Dis 2001;66:25-37.
- Kruger A. Schizophrenia: recovery and hope. Psychiatr Rehab J 2000; 4:29-37.
- Magliano L, Fadden G, Fiorillo A, et al. Family burden and coping strategies in schizophrenia: are key relatives really different to other relatives? Acta Psychiatr Scand 1999;99:10-15.
- Binou-Nakou I, Dikaiou M, Bairactaris C. Psychosocial dimensions of family burden among two groups of carers looking after psychiatric Soc Psychiatry Psychiatr Epidemiol 1997;32:104-108.
- Loukissa DA. Family burden in chronic mental illness:a review of re-search studies. J Adv Nurs 1995;21:248-255.
- Magliano L, Tosini P, Guarneri M, Marasco C, Catano F. Burden on the families of patients with obsesive-compulsive disorder: a pilot study. Eur Psychiatry 1996;11:192-197.
- 50. Bernstein GA, Warren SL, Massie ED, Thuras PD. Family dimensions in anxious-depressed school refusers. J Anxiety Disord 1999;13:513-528.
- Tamplin A, Goodyer IM, Herbert J. Family functioning and parent gen-eral health in families of adolescents with major depressive disorder. J Affect Disord 1998;48:1-13.
- Glynn SM, Marder SR, Liberman RP, et al. Supplementing clinical-based skills training with manual-based community support session: effects on social adjustment of patients with schizophrenia. Am J Psychiatry 2002;159:829-839.
- Heinssen RK, Liberman RP, Kopelowicz Psychological skills train-ing for schizophrenia: lessons from the laboratory. Schizophr Bull 2000; 26:21-46.
- Falloon IR, Shanham WJ. Community management of schizophrenia. Br J Hosp Med 1990;48:62-66.