Hong Kong J Psychiatry 2006;16:144-9
Original Article
The Impact of Painful Somatic Symptoms on Depressive Disorder: a Selected Literature Review
軀體性疼痛對抑鬱症的影曹:選擇性文獻研究
KL Lee, KC Tso
李嘉蓮、曹國柱
Ms KL Lee, The Chinese University of Hong Kong, Hong Kong, China.
Dr KC Tso, Department of Psychiatry, Queen Mary Hospital, Pokfulam, Hong Kong, China.
Tel: (852) 2855 3067; Fax: (852) 2819 3851;
E-mail: tsokc@hotmail.com
Submitted: 11 December 2006; Accepted: 22 January 2007
Abstract
Objective: To review the prevalence of painful somatic symptoms in depressed patients, and to evaluate the significance of such symptoms in modulating the course and outcome of the disorder.
Methods: Online databases including PubMed, Ovid, and Medline were searched using the key words: 'depression', 'dysthymia', 'hypochondriasis', 'pain', 'painful somatic symptoms', 'somatoform disorders', and 'somatisation'. Clinical studies published in recent 20 years (1986-2006) related to the co-occurrence of unexplained pain and depression were selected and reviewed.
Results: Six reviews and 11 original articles were selected. Among them, 6 recent clinical studies showed the prevalence of painful symptoms in diagnosed depressive western populations ranged from 43.4 to 92%, depending on the study setting and adopted research scales. Wide variations in the assessment of pain and depression were observed. Three longitudinal studies showed a negative effect of co-morbid pain on depression in respect of treatment response, quality of life, functional and economic burdens.
Conclusion: Co-morbid pain and depression is common in western populations, but its prevalence remains unknown in other communities. Despite its clinical importance, the lack of evidence to conclude the significance of co-morbid pain in modulating depressive symptomatology suggests the need for more clinical research in this area.
Key words: Comorbidity; Depressive disorder, major; Pain; Somatoform disorders
摘要
目的:探討軀體性疼痛病徵出現在抑鬱症病人的普及性,以及評估這些病徵對抑鬱症的影響。
方法:資料的來源包括網上資料庫(PubMed、Ovid及Medline) ,搜尋時用的關鍵字有「抑鬱症」、「輕抑症」、「疑病症」、「疼痛」、「身體形式症」、「軀體性疼痛病徵」及「身體化障礙」,以選出近二十年( 1986-2006) 有關未明的疼痛症及抑鬱症的共現性的臨床研究。
結果:共病性疼痛及抑鬱症在西方國家很普遍,但在其他社區仍是一個未知的範疇。鑑於其臨床重要性,加上目前缺乏共病性疼痛對抑鬱症所產生影響的證據,所以需要進行更多循證臨床研究來為此作進一步探討。
關鍵詞:共病性、抑鬱症、疼痛、軀體性疼痛病徵
Introduction
It is now well-established that pain and depression are related.1-3 The frequent co-occurrence of depression and somatic symptoms poses a continuing challenge to clinicians and researchers.3,4 A large proportion of patients with a somatoform disorder also satisfied the criteria for other psychiatric disorders, especially affective disorder.3,5
Somatisation is the process by which psychological distress is experienced and communicated in the form of somatic symptoms but has no pathophysiological explanation.6
Persistent somatisation is associated with a broad spectrum of heterogeneous psychiatric diagnoses and syndromes, imposing a serious burden on the mental health care system.7,8 Regarding personal burdens, since within these somatic symptoms, painful physical symptoms without diagnosed pathology (including headaches and backaches) are common, they can result in distress, dysfunction, and even disability.9-11
Although the underlying mechanism of the reciprocal relationship between painful somatic symptoms and depression is still unclear, different theories of the pain- depression relationship suggest the possibility of multiple levels involvement including different neurobiological, psychological, and behavioural mechanisms.3,4,12 Clinically, there was a high prevalence of anxiety, depression, and severe impairment in health-related quality of life in Hong Kong among Chinese patients with chronic non- cancer pain.13 Despite the fact that depressive symptoms in patients with chronic pain have been well-researched in a wide range of clinical settings, pain which can be one of the medically unexplained somatic symptoms in people with depression has attracted much less attention, as shown by the limited number of existing retrospective or cross-sectional studies.14,15 Most of the studies concerned the prognostic value of depression for poor pain outcomes but not the reverse.14 Although pain can be a predictor of depressive symptoms in some specific groups in primary care such as American women,15 and Chinese elderly,16 there is no conclusion about the significance of coexistence of painful somatic and depressive symptoms in clinical settings. In short, besides the lack of prospective studies, other problems include ill-defined and poorly targeted study sampling.11,15
In addition to the overlap among different psychiatric diagnoses and a lack of well-designed clinical studies, cultural effects further complicate evidence-based evaluation of co- morbid pain in modulating depressive symptoms. Cross- cultural epidemiological studies suggest that somatisation of depression is a common phenomenon in non-western societies.17 Meanwhile, Cheung et al18 suggested that Chinese patients suppress or disguise their deep feelings owing to fear of the powerful social stigma attached to mental illness in our culture. Similarly, in South India a study demonstrated that higher levels of depression are experienced as more stigmatisation resulting in patients’ emphasis of somatic pain.19 Kleinman20 drew similar conclusions: “Depression effect is socially and culturally unsanctioned, whereas suppressed. Somatisation is sanctioned and expressed, and carries both a cultural cachet and social efficacy.” Yet, there is no recent epidemiological study concerning the prevalence of somatisation in depressive patients in our locality.
Owing to the heavy burden of co-morbid pain and depression on both individuals as well as the mental health system, clinical research is necessary to evaluate the reciprocal relationship of these 2 debilitating symptoms and shed light on improving their diagnosis and management.
The objectives of this selected review were to highlight the important findings of recent literature in terms of (i) prevalence of co-morbid pain (which here refers to medically explained painful somatic symptoms) in depressive patients, (ii) sampling and assessment of co-morbid pain in depression, and (iii) significance of co- morbid pain on depressive symptomatology and related outcome measurement, in order to pave the way for feasible, representative longitudinal studies of the significance of co- morbid pain in modulating depressive symptomatology in our locality.
Methods
Databases searched included PubMed, Ovid, and Medline, using the key words ‘depression’, ‘dysthymia’, ‘hypochondriasis’, ‘pain’, ‘painful somatic symptoms’, ‘somatoform disorders’, and ‘somatisation’. Human studies (described in original and review articles) that reported in English and related to the co-occurrence of pain and depression were selected. Literature addressing pain due to diagnosed pre-morbid disease processes and symptom syndromes (e.g. rheumatism or arthritis, migraine, irritable bowel syndrome, or fibromyalgia) was excluded. Reference lists of selected articles were reviewed for additional papers of interest. Detailed qualitative analysis of papers was limited to those published in the last 20 years (1986-2006) and with online full text available.
Results
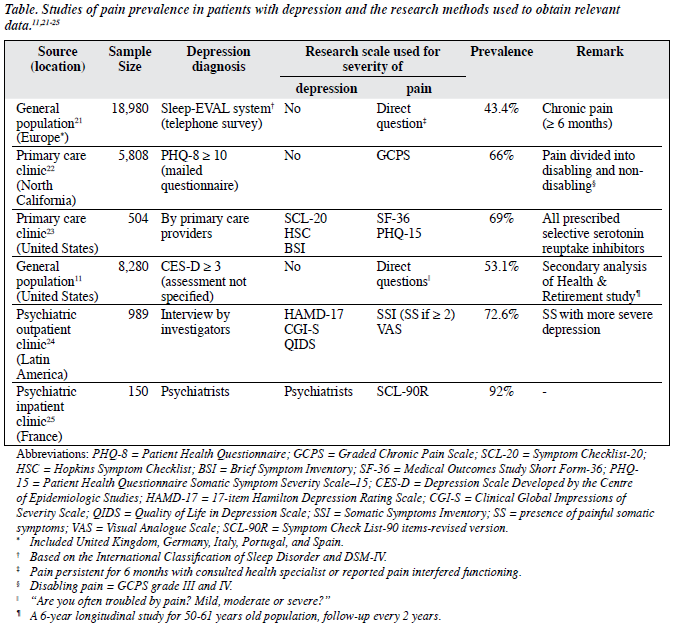
With the objective of highlighting prevalence of co-morbid pain in depressive patients, and evaluating the significance of co-morbid pain in modulating depressive symptomatology, a total of 6 reviews and 11 clinical studies were identified. They were published between 1996 and 2006 reported by different independent research groups worldwide. Six primary studies11,21-25 provided baseline prevalence measurements and mentioned research methods in detail. The related information was summarised in the Table.
Prevalence of Co-morbid Pain in Depressive Patients
Most of the literature addressed the prevalence of painful symptoms in the respective studied population by cross- sectional assessment, whenever baseline depressive and pain symptoms were measured. They included 6 European countries, namely: the United Kingdom, Germany, Italy, Portugal, Spain, and France.21,25 The rest of the studies referred to sample populations in the United States. In short, they all concerned western populations. The respective prevalence rates were all higher than 40%, ranging from 53.1%11 to 72.6%24 in the United States, and 43.4% in a large sample study in Europe.21 The highest prevalence of co-morbid pain in depressive patients was 92%,25 described in a study of psychiatric inpatients in France. Concerning different sampling methods, the prevalence of painful symptoms in diagnosed depressive population in primary care ranged from 43.4 %21 to 69%,23 while those in psychiatric outpatient clinics and inpatient groups showed higher prevalences of 72.6% and 92% respectively.24,25
The figure quoted in one study23 was 43 to 65%. A large-scale literature review14 published in 2003 showed the prevalence of co-morbid pain and depression ranged from 15 to 100% with a mean prevalence of 65%. It was quoted in a recent review12 published in 2006. This result came from 14 clinical studies, 12 of them with prevalences ranging from 41 to 85%, while the remaining studies yielded extremes of 15% and 100%, reported in 2 studies, published more than 20 years ago, with sample sizes of 100 and 16 respectively.
Sampling and Assessment of Co-morbid Painful Symptoms in Depression
As shown in the Table, 4 of 6 studies had their data sampled in non-psychiatric settings such as the general population and primary care clinics; only 2 were conducted in psychiatric settings involving either an outpatient or hospitalised sample. The assessment methods for depression diagnosis can be divided into 2 main groups. For studies conducted in the general population, the survey methods involved telephone interviews,21 mailed questionnaires,22 and self-administrated questionnaires.11 Whereas, interviews involving primary care providers,23 investigators,24 and psychiatrists25 were conducted in corresponding clinical settings. There was a great diversity in the research scales used. For depression and its severity, they included: the 17-item Hamilton Depression Rating Scale measuring severity of depression
and pain (HAMD-17), the Brief Symptom Inventory. For pain and its severity, they entailed the Graded Chronic Pain Scale and a Visual Analogue Scale as shown in the Table.
Significance of Co-morbid Pain on Depressive Symptomatology and Related Outcome Measurement
There were 3 recent reports addressing the longitudinal effects of pain on depressive symptom outcomes.Asecondary analysis23 of the Randomized Trial Investigating Serotonin Specific Reuptake Inhibitors (SSRI) Treatment (ARTIST) was primarily designed to compare the effectiveness of 3
SSRI (fluoxetine, paroxetine, and sertraline) in clinically depressed patients diagnosed by primary care providers. It analysed baseline and 3-month data obtained by computer- assisted telephone interviews, and revealed that compared to patients without pain, the odds ratios of a poor treatment response were 2.0 (95% confidence interval, 1.1-4.0) in those with moderate pain at baseline, and 4.1 (1.9-8.8) in those with severe pain. Concerning secondary outcomes, each incremental increase in pain severity doubled the odds of a poor health-related quality of life (HRQL) outcome. The investigators therefore concluded that pain is a strong predictor of poor depression and HRQL outcomes at 3 months. The Health and Retirement Study (HRS) tracked the national trends biennially in health and economic well- being among retired and near-retired Americans,11 which sampled an older population (aged 50-61 years). Instead of assessing the primary outcomes like depressive symptom severity, outcomes measurements focused on long-term functional and socio-economic aspects, e.g. onset of work disability, medical expenditures etc. The study concluded that relative to depression alone, depression plus pain were associated with significant functional limitations and economic burdens. Denninger et al26 sampled 170 outpatients enrolled in the Depression Clinical and Research Program at the Massachusetts General Hospital. These patients were aged 18 to 65 years, and had major depressive disorders and co-morbid somatic symptoms, including various types of pain. The somatic symptom scores derived from Symptom Questionnaire (Kellner) at baseline did not predict the degree of reduction in the HAMD-17 scores after 8 weeks of open-label treatment with fluoxetine.26 However they found that patients whose depression did not completely remit (responded but HAMD-17 score ≥ 6 at endpoint) had significantly more somatic symptoms (p < 0.03) than in other responders (≥ 50% reduction in HAMD-17 scores). This finding suggested that failing to adequately treat co- morbid somatic symptoms may make it more difficult to treat depression to complete remission.
Similarly, 2 interventional studies concluded that pain was a marker for a more difficult-to-treat depression.27,28 However, the latter studies were limited to late-life and recurrent depression respectively. By contrast, a cross-sectional study by Muñoz et al24 mentioned that there was no significant difference in the duration of current major depressive episode between patients with and without painful somatic symptoms, but their report mentioned no follow-up method and end- point measurement.
Discussion
The 43 to 92% prevalence of pain in depression noted in the 6 selected original articles published in the last decade agreed with figures mentioned in another large-scale review14 and primary studies,29-31 so long as the 2 extreme results were excluded. Although this review included large cross-sectional studies from different countries, the prevalence of painful somatic symptoms in depression among Asians was not addressed. Besides stigmatisation, as concluded in an international study,32 substantial variations in the prevalence of somatic symptoms (including headache and back pain) may reflect the characteristics of physicians and health care systems, as well as cultural differences among patients. As intimated earlier, some studies suggest that patients in non-western countries are more likely to report somatic symptoms than those in the West. Hence it is worth to conducting a study into such prevalence in Asian populations.
A qualitative review14 commented that “the prevalence rates do not appear to be influenced by the study setting”, in that there does not seem to be a difference between psychiatric versus primary care settings. Yet the primary studies selected here did show a difference in prevalence in respect of the sampled population; a higher prevalence among those who were hospitalised. However, great discrepancies in sample size, differences in diagnostic methods and definitions of depressive and painful symptoms mean that it is unreliable to conclude that in tertiary settings, depressed patients are more likely to have painful symptoms than those in primary care. However, studies have shown the presence of painful symptoms was associated with more severe depression at baseline.23,24
The differences in prevalence noted may be due to variations in the definitions of pain and depression across different study designs and subject populations, as suggested in some reviews.12,33 In these studies, although the diagnostic criteria for depression were all based on Diagnostic and Statistical Manual of Mental Disorders, 4th Edition (DSM-IV), assessment of depressive symptoms was mainly conducted by phone survey or self-administrated questionnaires in primary care, as face-to-face clinical interview by health professions was not feasible for such large samples. Possible over-diagnosis of depression in patients with painful symptoms may be another reason for such differences.21 Hence, it is necessary to plan rigorous comparative studies including patients attending primary care, psychiatric outpatient clinic, and those who are hospitalised. This could enable fair comparison of prevalence using the same study design. To obtain a precise diagnosis of depression instead of by imprecise screening (that introduces false-positive diagnoses), specialists in psychiatric outpatient clinics could provide a good start for baseline interviews.
As mentioned, most diagnostic criteria used in studies reviewed depended either directly on DSM-IV or on scales derived from it, and for this reason the term ‘major depressive disorder’ was commonly used.12,24,34 Research scales chosen differed in various clinical settings. For psychiatric outpatient clinics, a study from Latin America24 used the HAMD-17, which is a clinician-rated instrument completed following a thorough clinical interview.35 This instrument has been employed to assess depressive symptom severity, particularly in studies conducted in similar outpatient settings.27,28,34 However, there is no conclusion about the choice of research scale regarding other related domains like painful somatic symptoms, functional impairment, and quality of life, for which there is a great diversity of instruments.
Concerning painful symptoms, clear terminology is a particular problem. First, painful symptoms involve mainly subjective perception and experiences, for which there is no ideal objective measurement. Second, research scales used to differentiate painful and non-painful patients as well as for measuring the severity of pain were all different among reviewed studies. Studies that examined the concordance between subjective reports and external measures of pain have found good agreement between the two.21 Since we wanted to study the prognostic value of pain in depression, an objective and widely used scale needed to be employed. Some research scales for depression target painful symptoms. Separating the painful symptoms from depression assessment scores during statistical analysis can facilitate focusing the study on the significance of co-morbid pains that modulate other non-pain depressive symptoms. Although painful symptoms are not diagnostic in depression, the overlap of both painful and depressive symptoms is so common that 2 recent reviews suggested treating their coexistence as the rule rather than the exception. This might lead to better terminology and classification in forthcoming revisions of diagnostic criteria.4,33
There are relatively few studies specifically designed to assess the effect of pain on depression outcomes. Our observations agreed with the findings in other large literature reviews.14,33 Pain prevalence can be measured from cross-sectional study, while longitudinal study is necessary to find out the significance of co-morbid pain in modulating depressive symptomatology. However, only 3 studies were prospective and longitudinal, with follow-up of depression being at intervals of 8 weeks,26 3 months,23 and 2 years.11 However, none of them were designed specifically to examine the effect of pain on depression. Bair et al23 was a secondary analysis of the ARTIST study, which was primarily designed to compare the effectiveness of 3 SSRI, while Emptage et al11 analysed HRS, which was initiated to track national trends biennially among retired and near-retired Americans. Denninger et al26 recruited psychiatric outpatients, painful somatic symptoms were not specifically assessed and quantitatively graded. Although a large sample was involved, and other medical conditions remained more or less constant during analysis in Emptage et al’s study,11 the findings were not conclusive. It entailed a crude assessment of mental health and a self-administered questionnaire (depression being diagnosed if the Depression Scale Developed by the Centre of Epidemiologic Studies score was ≥ 3, sensitivity was 70%, and specificity 80%) for the diagnosis of depression. Generalising the study results from such a specific age-group to other depressed patients was also questionable.
The duration of follow-up for end-point measurement was another challenge to be tackled for our study to be representative. Obviously, 2 years11 would be too long for measuring the effect of co-morbid pain on depression to derive improved management. Muñoz et al24 mentioned that there was no significant difference in duration of current major depressive episodes between patients with and without painful somatic symptoms. This conclusion can be due to their poorly defined end-point; a cutoff at 6 months for current depressive episodes may be too long to reveal a significant difference in depression prognosis between the 2 groups. A longitudinal study36 indicates that core depressive and other related somatic symptoms including pain improve rapidly within first month of SSRI treatment before gradually attaining a plateau. Thus, to undertake a meaningful comparison of depression prognosis in relation to pain symptoms, patient follow-up every month rather than after 6 months may be more appropriate.23
As our objective was to explore the prognostic value of pain in depression rather than the effects of an intervention, management of patients with and without pain needed to be optimal to exclude any treatment effect on outcomes. Although duloxetine was claimed to be more effective than placebo as a treatment of painful symptoms in depression,34 when compared to treatment with other available anti- depressants in relieving pain symptoms, it was not superior.4
Similarly, no meta-analyses have examined the relative or absolute efficacy of different classes of anti-depressants for treating pain in patients with depression.33 Hence it appears reasonable to conduct a naturalistic, observational study, there being no consensus management for painful symptoms in depressed patients that can alter the prognosis of depression.
In short, 3 longitudinal studies showed that co-morbid pain had no effect on depression in respect of treatment response, quality of life, functional and economic burden. However, these studies were not specifically designed for this purpose. Moreover, other important outcomes of depression such as severity and chronicity, as well as suicidality were not addressed. Only literature published in the last decade addressed these issues and was therefore selected for this review. Other relevant literature may have been missed due to the limitation that only an online search was performed. Despite the high prevalence of co- morbid pain and depressive symptoms worldwide, current knowledge about their relationship and management is limited to conceptual and empirical aspects. Owing to the possible effect of cross-cultural difference on pain expression and depressive symptomatology, it appears worthwhile to perform local longitudinal follow-up studies from both psychiatric outpatient and inpatient settings. Hopefully, the evidence on how co-morbid pain can modulate depressive symptoms may pave the way for more suitable diagnosis and management strategies for these unfortunate patients.
References
- Romano JM, Turner JA. Chronic pain and depression: does the evidence support a relationship? Psychol Bull 1985;97:18-34.
- Katon W. The epidemiology of depression in medical care. Int J Psychiatry Med 1987;17:93-112.
- Von Korff M, Simon G. The relationship between pain and depression. Br J Psychiatry Suppl 1996;(30):101-8.
- Henningsen P, Lowe B. Depression, pain, and somatoform disorders. Curr Opin Psychiatry 2006;19:19-24.
- Bass C. Somatization, physical symptoms and psychological illness. Oxford: Blackwell Scientific; 1991.
- Lipowski ZJ. Somatization: the concept and its clinical application. Am J Psychiatry 1988;145:1358-68.
- Fink P. Psychiatric illness in patients with persistent somatisation. Br J Psychiatry 1995;166:93-9.
- Demopulos C, Fava M, McLean NE, Alpert JE, Nierenberg AA, Rosenbaum JF. Hypochondriacal concerns in depressed outpatients. Psychosom Med 1996;58:314-20.
- Barsky AJ, Borus JF. Somatization and medicalization in the era of managed care. JAMA 1995;274:1931-4.
- Lobo A, Garcia-Campayo J, Campos R, Marcos G, Perez-Echeverria MJ. Somatisation in primary care in Spain: I. Estimates of prevalence and clinical characteristics. Working Group for the Study of the Psychiatric and Psychosomatic Morbidity in Zaragoza. Br J Psychiatry 1996;168:344-8.
- Emptage NP, Sturm R, Robinson RL. Depression and comorbid pain as predictors of disability, employment, insurance status, and health care costs. Psychiatr Serv 2005;56:468-74.
- Williams LJ, Jacka FN, Pasco JA, Dodd S, Berk M. Depression and pain: an overview. Acta Neuropsychiatrica 2006;18:79-87.
- Lee S, Chen PP, Lee A, Ma M, Fong CM, Gin T. A prospective evaluation of health-related quality of life in Hong Kong Chinese patients with chronic non-cancer pain. Hong Kong Med J 2005;11:174-
- Erratum in: Hong Kong Med J 2005;11:280.
- Bair MJ, Robinson RL, Katon W, Kroenke K. Depression and pain comorbidity: a literature review. Arch Intern Med 2003;163:2433-45.
- Terre L, Poston WS, Foreyt J, St Jeor ST. Do somatic complaints predict subsequent symptoms of depression? Psychother Psychosom 2003;72:261-7.
- Chou KL, Chi I. Reciprocal relationship between pain and depression in elderly Chinese primary care patients. Int J Geriatr Psychiatry 2005;20:945-52.
- Jablensky A, Sartorius N, Gulbinat W, Ernberg G. Characteristics of depressive patients contacting psychiatric services in four cultures. A report from the WHO collaborative study on the assessment of depressive disorders. Acta Psychiatr Scand 1981;63:367-83.
- Cheung FM, Lau BW, Waldmann E. Somatization among Chinese depressives in general practice. Int J Psychiatry Med 1980-81;10:361-74.
- Raguram R, Weiss MG, Channabasavanna SM, Devins GM. Stigma, depression, and somatization in South India. Am J Psychiatry 1996;153:1043-9.
- Kleinman A. Social origins of distress and disease: depression, neurasthenia, and pain in modern China. New Haven, Conn: Yale University Press; 1986:178.
- Ohayon MM, Schatzberg AF. Using chronic pain to predict depressive morbidity in the general population. Arch Gen Psychiatry 2003;60:39- 47.
- Arnow BA, Hunkeler EM, Blasey CM, Lee J, Constntino MJ, Fireman B, et al. Comorbid depression, chronic pain, and disability in primary care. Psychosom Med 2006;68:262-8.
- Bair MJ, Robinson RL, Eckert GJ, Stang PE, Croghan TW, Kroenke K. Impact of pain on depression treatment response in primary care. Psychosom Med 2004;66:17-22.
- Muñoz RA, McBride ME, Brnabic AJ, López CJ, Hetem LA, Secin R, et al. Major depressive disorder in Latin America: the relationship between depression severity, painful somatic symptoms, and quality of life. J Affect Disord 2005;86:93-8.
- Corruble E, Guelfi JD. Pain complaints in depressed inpatients. Psychopathology 2000;33:307-9.
- Denninger JW, Papakostas GI, Mahal Y, Merens W, Alpert JE, Nierenberg AA, et al. Somatic symptoms in outpatients with major depressive disorder treated with fluoxetine. Psychosomatics 2006;47:348-52.
- Karp JF, Weiner D, Seligman K, Butters M, Miller M, Frank E, et al. Body pain and treatment response in late-life depression. Am J Geriatr Psychiatry 2005;13:188-94.
- Karp JF, Scott J, Houck P, Reynolds CF, Kupfer DJ, Frank E. Pain predicts longer time to remission during treatment of recurrent depression. J Clin Psychiatry 2005;66:591-7.
- Hollifield M, Katon W, Morojele N. Anxiety and depression in an outpatient clinic in Lesotho, Africa. Int J Psychiatry Med 1994;24:179- 88.
- Lindsay PG, Wyckoff M. The depression-pain syndrome and its response to antidepressants. Psychosomatics 1981;22:571-3,576-7.
- Vaeroy H, Merskey H. The prevalence of current major depression and dysthymia in a Norwegian general practice. Acta Psychiatr Scand 1997;95:324-8.
- Simon GE, VonKorff M, Piccinelli M, Fullerton C, Ormel J. An international study of the relation between somatic symptoms and depression. N Engl J Med 1999;341:1329-35.
- Katona C, Peveler R, Dowrick C, Wessely S, Feinmann C, Gask L, et al. Pain symptoms in depression: definition and clinical significance. Clin Med 2005;5:390-5.
- Brannan SK, Mallinckrodt CH, Brown EB, Wohlreich MM, Watkin JG, Schatzberg AF. Duloxetine 60 mg once-daily in the treatment of painful physical symptoms in patients with major depressive disorder. J Psychiatr Res 2005;39:43-53.
- Nezu CM, Nezu AM, Foster SL. Practitioner’s guide to empirically based measures of depression—AABT clinical assessment series. In: Measure of depression, depressive symptomatology, and depressive mood. New York: Kluwer Academic/Plenum Publishers; 2000:58.
- Greco T, Eckert G, Kroenke K. The outcome of physical symptoms with treatment of depression. J Gen Intern Med 2004;19:813-8.