East Asian Arch Psychiatry 2011;21:157-163
ORIGINAL ARTICLE
Dr Rohit Verma, MD, Department of Psychiatry, Post Graduate Institute of Medical Education and Research at Dr Ram Manohar Lohia Hospital, New Delhi, India.
Dr Yatan Pal Singh Balhara, MD, DNB, MNAMS, Department of Psychiatry and De-addiction, Lady Hardinge Medical College and Smt. S. K. Hospital, New Delhi, India.
Prof. Smita N Deshpande, MD, Department of Psychiatry, Post Graduate Institute of Medical Education and Research at Dr Ram Manohar Lohia Hospital, New Delhi, India.
Address for correspondence: Dr Yatan Pal Singh Balhara, Department of Psychiatry and De-addiction, Lady Hardinge Medical College and Smt. S. K. jnlAuthAff, New Delhi 110001, India.
Tel: (91-0) 9868976365; Email: ypsbalhara@gmail.com
Submitted: 22 June 2011; Accepted: 5 August 2011
Abstract
Objectives: Inhalant use has been considered one of the most dangerous forms of substance abuse leading even to serious accidents and death. The current study explored the correlates of inhalant abuse in subjects from a drug de-addiction clinic.
Methods: The study was conducted at a tertiary-level multi-specialty hospital in India, which entailed a chart review of patients with inhalant abuse / dependence presenting to the clinic over a 2-year period. All the treatment records of the de-addiction clinic were reviewed and information gathered regarding these patients.
Results: The study involved the records of 36 subjects, with a mean age of 16 years (standard deviation, 4; range, 11-26 years). Most subjects (86%) were adolescents; three-quarters of whom had no family history of substance abuse. The mean (standard deviation) age of initiation of inhalant use was 14 (4) years. The commonest cause of first use reported by the subjects was experimentation (94%), and 97% of them came to know of inhalant from their inhalant-using friends.
Conclusions: These findings provide important information on a relatively under-researched area.
Key words: Adolescent; Inhalant abuse; Substance-related disorders
摘要
目的:使用吸入剂被视为其中一种最危险的滥药方式,可导致严重事故或致命。本研究检视一所药物脱瘾诊所内吸入剂滥用患者的相互关联。
方法:研究於印度一所第叁层护理多门专科医院进行,涵盖过去2年因吸入剂滥用或依赖入院患者的病历回顾,并回顾所有治疗纪录和收集患者相关资料。
结果:研究共纳入36名患者的病历纪录。他们的平均年龄为16岁(标準差为4岁;介乎11-26岁)。大部份患者为青少年(86%);75%患者没有家族药物滥用史。他们开始使用吸入剂的平均年龄为14岁(标準差为4岁),而首次使用吸入剂的最常见原因是出於尝试(94%),当中 97%受友人影响而开始使用吸入剂。
结论:基於针对这个範畴的研究十分不足,是次研究结果或为此提供重要信息和启示。
关键词:青少年、吸入剂滥用、药物滥用相关病患
Introduction
Inhalants refer to a group of psychoactive substances that get transformed to vapours and produce mind-altering effects. Inhalant use has been considered one of the most dangerous forms of substance abuse, even leading to death and serious accidents.1,2 Commonly used inhalants include: petrol, paint thinners, paint removers, glues, typewriter correction fluids, adhesives, and varnishes. The prevalence of inhalant abuse has been reported to vary from 9 to 20%.3,4
The general absence of knowledge5 is reflected in the
The current study therefore set out to explore the correlates of inhalant abuse of the subjects from a drug de- addiction clinic.
Methods
The study was conducted at a tertiary-level multi-specialty hospital. The study subjects were recruited from the drug dependence treatment clinic run in the institute’s Department of Psychiatry and De-addiction. The patients presenting to the treatment clinic were assessed in detail and diagnosed using the DSM-IV / ICD-10 nosological systems. Subsequently an individualised treatment plan was formulated for each patient. The predominant substances of abuse observed in the clinic included: tobacco, alcohol, cannabis, and opioids. However, among children and adolescents, inhalants constituted a major group of substances of abuse.
The current study was a chart review of the cases with inhalant abuse / dependence presenting to the clinic over the 2-year period, from January 2008 to December 2009. All the treatment records of the de-addiction clinic were reviewed, and information gathered regarding patients with inhalant abuse / dependence. The definition of inhalant abuse and dependence was that used in the DSM-IV — a maladaptive impairment or distress, as manifested by impairment in physical, occupational, legal and social domains, occurring within a 12-month period. Inhalant dependence was defined as a maladaptive pattern of inhalant use leading to clinically significant impairment or distress, as manifested by ≥ 3 of period.
Information on socio-demographic parameters, which included age, gender, marital status, education level, occupation, income, family type, religion, place of residence, and the support system, was collected. For the purpose of the current study, adolescence was defined as the period between the age of 10 and 19 years, according to the World Health Organization guidelines. The nuclear family was defined as the family structure where the unmarried children stayed with their parents. The joint family was defined as the family where 2 or more married couples stayed together. Conditions of anonymity and confidentiality were strictly adhered to during the course of the study.
Information was also gathered on the substance use duration of use, reason for initiation, amount used, type of inhalant used, family history of substance abuse / dependence, history of psychiatric illness, and the level of impairment attributed to inhalant use. Previous quitting attempts and reasons for seeking treatment were also looked into.
Data Analyses
Data analysis was carried out using the Statistical Package for the Social Sciences, Windows version 17.0. Descriptive analysis of the study variables was carried out. Inter-group analyses were also conducted for subjects with and without psychiatric co-morbidity, and those with and without previous abstinence attempts. For this purpose, independent sample t tests and the Mann-Whitney U test were respectively used for parametric and non-parametric analyses.
Results
Socio-demographic Profile
The study included records of 36 subjects, whose mean (standard deviation [SD]) age was 16 (4) years (range, 11-26 years); all of whom were male. The majority (86%) were adolescents (age range, 10-19 years); 35 (97%) were unmarried. Moreover, 11% were illiterate, 39% had studied up to high school, and 3% were university graduates. While 56% of the subjects were studying, 17% were engaged in some form of occupation. Almost all the subjects (95%) were from an urban background; 75% hailed from nuclear families, 19% from joint families, and around 6% were living alone (Table 1). Besides, 85% belonged to the lower socio-economic class and the rest were from the middle
Table 1. Socio-demographic profile of the subjects.

socio-economic class. About 75% of the subjects enjoyed fair social and family support. In all, 97% were brought for treatment by family members and the rest had come alone.
Family History
About 75% of the subjects had no family history of substance abuse. Co-morbid alcohol and tobacco abuse was present among 12% of those having a family history of substance abuse. There was no family history of psychiatric illness in any subject.
Inhalant Use
The mean (SD) age of initiation of inhalant use was 14 (4) years. The duration of inhalant use prior to coming to the treatment centre varied from 1 month to 120 months (mean [SD] = 27 [8] months). The mean (SD) amount of inhalant used per day was 3 (2) bottles.
The commonest reason for first use reported was experimentation (94%); 97% of the subjects came to know of the inhalants from their inhalant-using friends. Of the 36 subjects, 75% met the DSM-IV criteria for inhalant dependence and remainder met the criteria for harmful use. For 69% of the subjects, inhalant was the first psychoactive substance used and 42% reported it to be the only one. Also, 67% reported inhalants to be the most preferred psychoactive substance; 28% reported them to be the second most preferred substance (Table 2). The most common inhalant reported was typewriter erasing fluid (29%), whereas 26% reported using solvent. Other variants included adhesives, glue, thinners (11% for each), whitener fluid (6%), petrol and grease (both 3%) [Fig 1a].
Sniffing was the most common route used for inhaling and reported by 80% of the subjects. Other routes included bagging (by 3%), both sniffing and huffing (11%), and huffing and bagging (6%) [Fig 1b].
Table 2. Parameters related to inhalant use by the subjects.
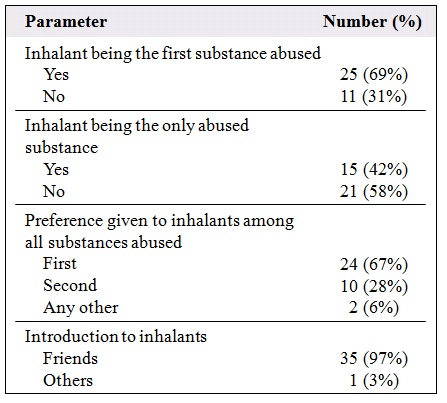
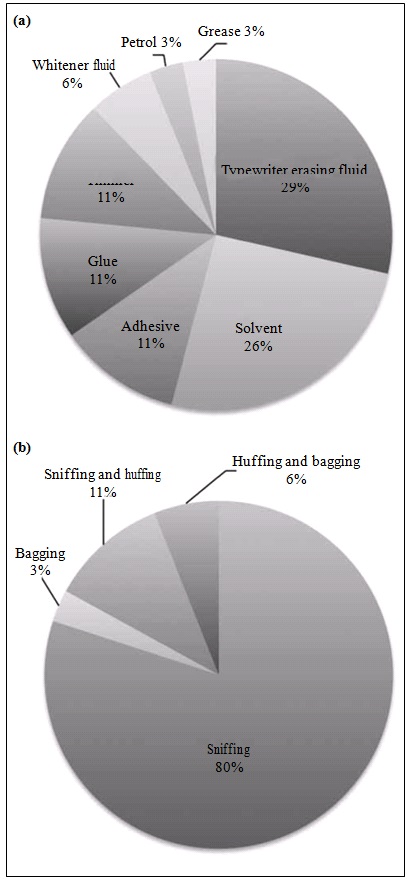
Figure 1. (a) Types of inhalant abused and (b) routes of inhalant abuse by the study subjects.
The most common reason for initiating inhalant use was curiosity (55%); 12% initiated use under peer pressure, and 19% as a substitute for other substances.
A feeling of intoxication following use of the inhalants was reported by 83% of the subjects. Other disturbances (100%), unsteadiness (100%), light- headedness (100%), and unresponsiveness (30%). A history of delirium was given by 5% of the subjects
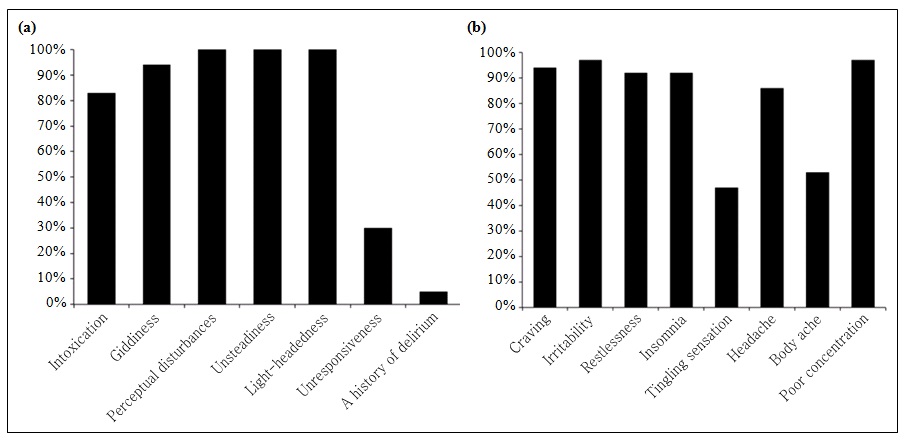
Figure 2. (a) Common side-effects attributed to inhalant use by our subjects; and (b) common withdrawal features attributed to inhalant use by our subjects.
(Fig 2a). Common withdrawal symptoms reported included: craving for the inhalants (94%), irritability (97%), restlessness (92%), insomnia (92%), tingling (47%), headache (86%), poor concentration (97%), and body ache (53%) [Fig 2b].
Abstinence Attempts
Only 16% had made an attempt to abstain in the past. Of the 36 subjects, 32 (89%) had come to seek treatment because of family pressure and 11% on their own accord. Comparison of subjects with and without a history of attempting abstinence did not reveal any significant differences (Table 3).
Co-morbidity
Co-morbid substance use ensued in 64% of the subjects, the most common being tobacco (n = 7 [19%]) and a combination of tobacco and alcohol (n = 6 [17%]). Co- morbid psychiatric disorder was present in 39% (n = 14) of the subjects. The most common of these included disorderly conduct (n = 11) and depression (n = 2). All 36 subjects had some kind of impairment in functioning. Comparison of subjects with and without co-morbidity revealed that the mean duration of inhalant use was significantly longer among those with psychiatric co-morbidity (t = 2.36, p = 0.02). These 2 groups did not differ with respect to any other parameters (Table 4).
Discussion
This study was conducted at a tertiary-level multi-specialty hospital and involved a detailed chart review.
In a study from India that reported 21 cases, 62% of the subjects belonged to the childhood and adolescent age- group, while 86% in the current study were adolescents. Inhalant use has been reported to begin during late childhood and adolescence. Young males appeared to be most vulnerable to the inhalant-associated mortality.12
The majority of our subjects (almost 90%) were literate. Most had attended school and consequently a school- based prevention programme could be of immense help in tackling this problem from a public health perspective.13
The finding of more than 50% of the users who were still enrolled in schools / colleges was not in keeping with earlier reports,8,14 for which there could be different explanations. First, the study cohort could have differed. Alternatively, we might have intercepted the subjects relatively earlier in the course of their substance use, and hence dysfunction was not severe enough to lead to school drop-out. Either way, this provides an excellent window of opportunity to undertake school-based interventions.
The finding of lower levels of substance use problems in those with higher levels of social, family, and parental support is also different from studies in the West15 as well as one previous study in a developing country setting.16
A higher prevalence of substance abuse among parents has been associated with high rates of similar behaviour in children. The findings of good social / family support are in keeping with previous work on substance use from developing countries. This phenomenon could be used with advantage when it comes to treatment planning for individuals with caregivers who could act as co-therapists. Resource-deficient developing country settings are likely to benefit immensely from such an approach. Thus, family support and a sense of togetherness among the family members appear to be protective against inhalant use by adolescents.17
Table 3. Between-group differences for the subjects with and without a history of abstinence attempts.
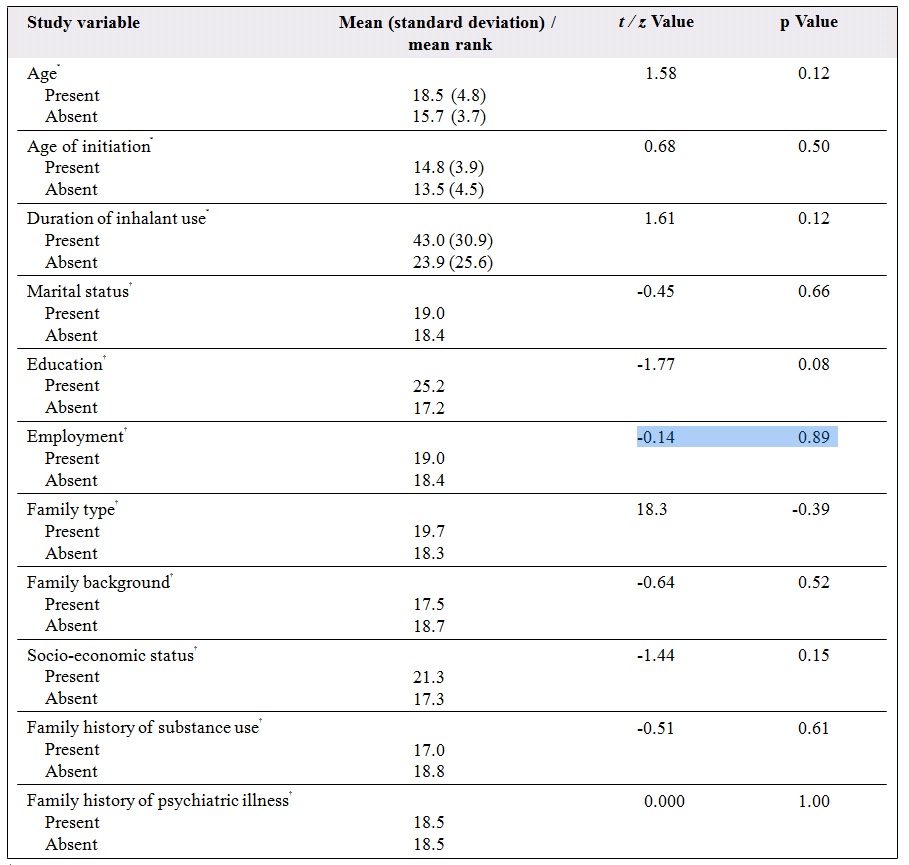
* Independent sample t test.
† Mann-Whitney U test.
A sense of experimentation with friends remains the commonest reason for initiation of different types of substance use, which was also corroborated by the current study. The most common reason was curiosity (55%); 20% initiated their use due to peer pressure, and 19% as a substitute for other substances. Curiosity about the inhalants was also the commonest reason for inhalant initiation reported by Perron et al.18 Appreciation of such reasons for initiation could be used to plan prevention strategies, such as social marketing.
In all, nearly 70% of the subjects reported inhalants as the first substance ever used. A significant proportion (42%) used inhalants as the only abused substance. Moreover, 95% of users reported inhalants as the most preferred substance. These are unusual findings as tobacco and cannabis have been reported as gateway drugs ultimately leading to the use of harder substances. Since a majority of the users in the current study were using only the inhalants, their role as potential gateway drugs needs to be explored.19 This possibility is supported by the fact that the majority of inhalant users were in their childhood or adolescence, and an association between inhalant use and future development of poly-drug use has been reported.20,21
The clinical features (symptoms) reported by our study subjects following inhalant use have been described earlier.22 Their withdrawal symptoms help us understand
Table 4. Between-group differences for subjects with and without a history of psychiatric co-morbidity.
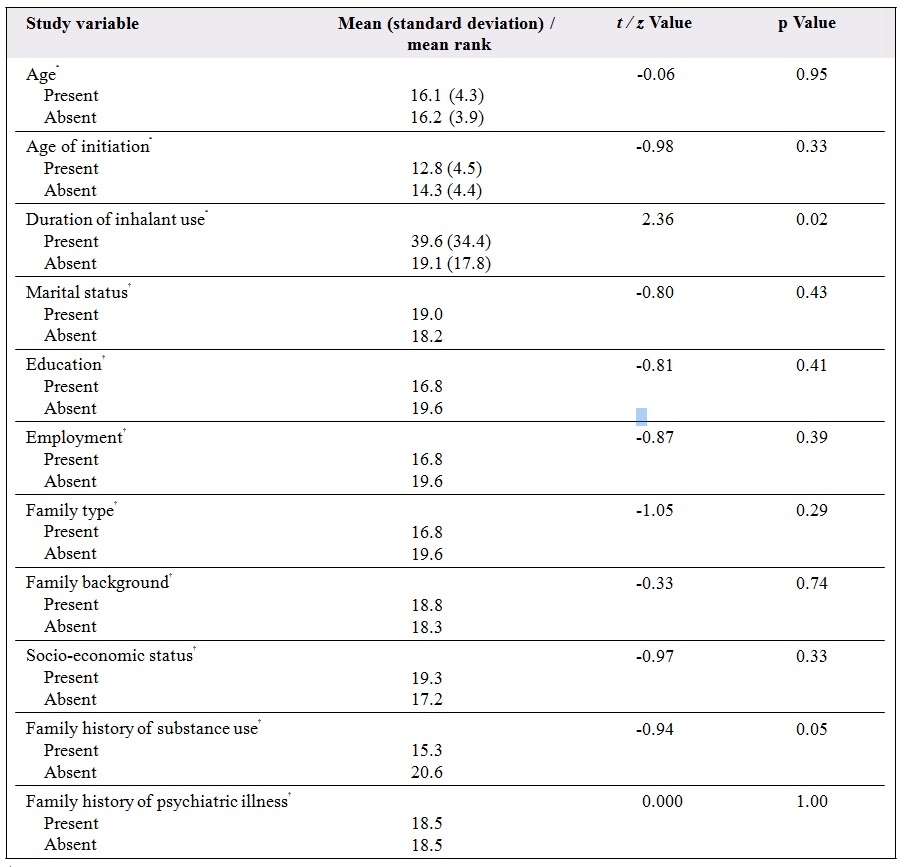
* Independent sample t test.
† Mann-Whitney U test.
the physiological and psychological concomitants of the phenomenon and may facilitate better management. This appears to be essential, in view of the high rate of substance use relapse. Concerns have been expressed over the validity of existing criteria for inhalant abuse and inhalant dependence.4 Phenomenological studies of the clinical symptoms and signs associated with inhalant intoxication and withdrawal, as explored in the current study, could help clarify these issues.
Inhalant use is often associated with delinquency, depression, and suicidal behaviour.23,24 The current study found high rates of conduct disorder and depression among our subjects.
The low percentage of subjects who were self- motivated to attempt abstinence highlights the need for motivation enhancement therapy (MET). Also, high levels of family pressure reflect the concern and support of family members that have the same objective. This could be used to advantage in the treatment plan. Both MET and family therapies have been found effective for substance users.25
Multi-system therapy could also be an effective strategy for these individuals, and has been particularly useful for children and adolescents in substance abuse.26
Notably, there was a lack of past abstinence attempts in most of our subjects, which reflects the importance of maximising the opportunity provided by current treatment-seeking behaviour. The current study provides insight and understanding into the patterns and profiles of patients using inhalants. For example, such information could be utilised towards planning of treatment services. The factors associated with the initiation and profiles of users could also provide input into planning appropriate prevention programmes. This assumes even greater importance, since the understanding in the inhalant use problems remains very limited, there being a dearth of literature on the topic, especially in developing countries.
The current study explores one of the under-studied phenomena in the Indian setting. Inhalant abuse remains incompletely understood with regard to its epidemiology, clinical presentation, aetiology and management. The present study provides some insights.
One limitation of our study was its reliance on chart review, rather than a prospective methodology. In addition, we did not use a standardised tool for assessing impaired functioning. Future studies should also explore the impact of different therapeutic interventions on outcomes.
References
- Pfeiffer H, Al Khaddam M, Brinkmann B, Köhler H, Beike J. Sudden death after isobutane sniffing: a report of two forensic cases. Int J Legal Med 2006;120:168-73.
- Chakroun R, Faidi F, Hedhili A, Charbaji K, Nouaigui H, Laiba MB. Inhalant abuse detection and evaluation in young Tunisians. J Forensic Sci 2008;53:232-7.
- Wu LT, Pilowsky DJ, Schlenger WE. Inhalant abuse and dependence among adolescents in the United States. J Am Acad Child Adolesc Psychiatry 2004;43:1206-14.
- Perron BE, Vaughn MG, Howard MO, Bohnert A, Guerrero E. Item response theory analysis of DSM-IV criteria for inhalant-use disorders in adolescents. J Stud Alcohol Drugs 2010;71:607-14.
- Young SJ, Longstaffe S, Tenenbein M. Inhalant abuse and the abuse of other drugs. Am J Drug Alcohol Abuse 1999;25:371-5.
- Diagnostic and statistical manual of mental disorders. 4th ed, text revision. Washington, DC; American Psychiatric Association; 2000.
- Das PS, Sharan P, Saxena S. Kerosene abuse by inhalation and ingestion. Am J Psychiatry 1995;149:710.
- Waraich BK, Chavan BS, Raj L. Inhalant abuse: a growing public health concern in India. Addiction 2003;98:1169.
- Shah R, Vankar GK, Upadhyaya HP. Phenomenology of gasoline intoxication and withdrawal symptoms among adolescents in India: a case series. Am J Addict 1999;8:254-7.
- Basu D, Jhirwal OP, Singh J, Kumar S, Mattoo SK. Inhalant abuse by adolescents: a new challenge for Indian physicians. Indian J Med Sci 2004;58:245-9.
- 1 Konghom S, Verachai V, Srisurapanont M, Suwanmajo S, Ranuwattananon A, Kimsongneun N, et al. Treatment for inhalant dependence and abuse. Cochrane Database Syst Rev 2010;(12):CD007537.
- Wick R, Gilbert JD, Felgate P, Byard RW. Inhalant deaths in South Australia: a 20-year retrospective autopsy study. Am J Forensic Med Pathol 2007;28:319-22.
- Botvin GJ, Griffin KW, Diaz T, Ifill-Williams M. Drug abuse prevention among minority adolescents: posttest and one-year follow- up of a school-based preventive intervention. Prev Sci 2001;2:1-13.
- Seth R, Kotwal A, Ganguly KK. Street and working children of Delhi, India, misusing toluene: an ethnographic exploration. Subst Use Misuse 2005;40:1659-79.
- Blatherwick CE. Understanding glue sniffing. Can J Public Health 1972;63:272-6.
- Kumar S, Grover S, Kulhara P, Mattoo SK, Basu D, Biswas P, et al. Inhalant abuse: a clinic-based study. Indian J Psychiatry 2008;50:117- 20.
- Pack R, Krishnamurthy G, Cottrell L, Stanton B, D’Alessandri D, Burns J. Caregiver predictors of adolescent inhalant abuse in rural Appalachia. Am J Health Behav 2005;29:331-41.
- Perron BE, Vaughn MG, Howard MO. Reasons for using inhalants: evidence for discrete classes in a sample of incarcerated adolescents. J Subst Abuse Treat 2008;34:450-5.
- Anderson CE, Loomis GA. Recognition and prevention of inhalant abuse. Am Fam Physician 2003;68:869-74.
- Bennett ME, Walters ST, Miller JH, Woodall WG. Relationship of early inhalant use to substance use in college students. J Subst Abuse 2000;12:227-40.
- Wu LT, Pilowsky DJ, Schlenger WE. High prevalence of substance use disorders among adolescents who use marijuana and inhalants. Drug Alcohol Depend 2005;78:23-32.
- National Institute of Drug Abuse. Research report series: inhalant abuse. NIH Publication Number 05-3818, Revised March 2005.
- Borges G, Walters EE, Kessler RC. Associations of substance use, abuse, and dependence with subsequent suicidal behavior. Am J Epidemiol 2000;151:781-9.
- Kelder SH, Murray NG, Orpinas P, Prokhorov A, McReynolds L, Zhang Q, et al. Depression and substance use in minority middle- school students. Am J Public Health 2001;91:761-6.
- Ozechowski TJ, Liddle HA. Family-based therapy for adolescent drug abuse: knowns and unknowns. Clin Child Fam Psychol Rev 2000;3:269-98.
- Dhawan A, Balhara YPS, Mohan I. Adolescent substance abuse. In: Lal R, editor. Substance use disorder — manual for physicians. New Delhi: National Drug Dependence Treatment Centre, All India Institute of Medical Sciences; 2005: Chapter 18.


