East Asian Arch Psychiatry 2020;30:52-6 | https://doi.org/10.12809/eaap1885
ORIGINAL ARTICLE
Shahrbanoo Ghahari, PhD, Department of Mental Health, School of Behavioral Sciences and Mental Health (Tehran Institute of Psychiatry), Iran University of Medical Sciences, Tehran, Iran
Kourosh Mohammadi-Hasel, PhD, Department of Psychology, Roodehen Branch, Islamic Azad University, Damavand, Iran
Seyed Kazem Malakouti, MD, Department of Social Psychiatry, Center of Excellence in Psychiatry, School of Behavioral Sciences and Mental Health (Tehran Institute of Psychiatry), Iran University of Medical Sciences, Tehran, Iran
Mohsen Roshanpajouh, MD, Addiction Researches Department, Center of Excellence in Psychiatry, School of Behavioral Sciences and Mental Health (Tehran Institute of Psychiatry), Iran University of Medical Sciences, Tehran, Iran
Address for correspondence: Mohsen Roshanpajouh, Addiction Researches Department, Center of Excellence in Psychiatry, School of Behavioral Sciences and Mental Health (Tehran Institute of Psychiatry), Iran University of Medical Sciences, Tehran, Iran
roshanpajouh.m@iums.ac.ir
Submitted: 3 October 2018 Accepted: 9 January 2020
Abstract
Background: Generalised anxiety disorder (GAD) has harmful effects on physical and mental health and quality of life. Mindfulness-based cognitive therapy (MBCT) is a treatment option for GAD. This meta- analysis was conducted to determine the effectiveness of MBCT on GAD.
Methods: Two authors independently performed the eligibility, quality assessment, and data extraction processes, and consensus was reached in case of discrepancies. Electronic databases were searched for eligible studies (randomised controlled trials, randomised trials, cluster randomised controlled trials, and clinical trials) up to November 2018 using keywords: mindfulness-based cognitive therapy OR mindfulness based cognitive therapy OR MBCT AND general anxiety disorder OR GAD*. The methodological quality of studies was assessed using the revised Jadad scale. Cohen’s formula was used to determine the effect size based on the mean and standard deviation of the changes in the study groups before and after the intervention.
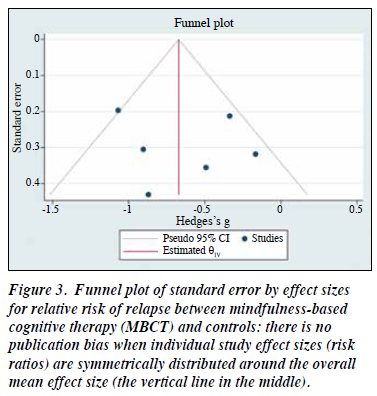
Results: Six studies that compared the effectiveness between MBCT and controls were included for analysis. The mean revised Jadad score of the six studies was 4.3 (range, 3-6). The overall mean effect size was -0.65. The funnel plot of effect sizes in relation to the effect size standard error showed a symmetrical distribution. Compared with controls, MBCT significantly improved the treatment outcome of GAD in all studies, except one.
Conclusion: MBCT was effective for treating GAD.
Key words: Anxiety disorder; Cognitive behavioural therapy; Meta-analysis; Mindfulness
Introduction
Generalised anxiety disorder (GAD) is characterised by extreme and uncontrollable worries and is associated with other anxiety disorders, depression, and a range of physical health disorders.1 GAD often occurs in early adulthood and is twice as likely to occur in women as in men.2 The prevalence of GAD in the Iranian population aged 18 to 65 years is 2.5%3 and 0.6% to 4.3% in other countries. The risk of its lifetime prevalence is 9%.4 GAD has more harmful effects than other anxiety disorders on physical and mental health and quality of life.5,6 All these disorders use considerable healthcare services and cause functional disruptions.7
Pharmacotherapy is the first treatment option.8,9 However, it is associated with a relatively high rate of relapse and uncertain lasting effects after discontinuation of medication.10,11 Thus, psychological treatments are necessary.
Mindfulness-based cognitive therapy (MBCT) can reduce general anxiety symptoms and anxiety sensitivity (the main components of GAD), with a specific mental orientation towards experience and awareness about the present time in a non-judgmental style by minimising the involvement in thoughts and feelings.12 MBCT is effective in treating patients with GAD.13 MBCT is an effective adjuvant to pharmacotherapy in patients with panic disorderor GAD.14 MBCT is more efficacious than a training programme for treating anxiety disorder.15 Therefore, we conducted a meta-analysis on the effectiveness of MBCT on GAD.
Methods
The PRISMA guideline for reporting systematic reviews and meta-analyses was used.16 Inclusion criteria for studies were: (1) randomised controlled trials, randomised trials, cluster randomised controlled trials, and clinical trials of MBCT for the treatment of GAD reported in English or Persian languages and published in peer-reviewed journals. (2) Participants aged ≥18 years diagnosed with GAD or GAD symptoms according to any diagnostic classification system who underwent MBCT, with anxiety scores measured according to a standard test.
Two authors independently performed the eligibility, quality assessment, and data extraction processes, and consensus was reached in case of discrepancies. Electronic databases (PsycINFO, PubMed, Embase, ProQuest, Scopus, Web of Science, Google Scholar, and Medline) were searched for eligible studies up to November 2018 using keywords: mindfulness-based cognitive therapy OR mindfulness based cognitive therapy OR MBCT AND general anxiety disorder OR GAD*. Papers in clinical psychology journals and other journals that had the most relevant early studies were also searched manually. In addition, reference lists of found articles and other reviews were inspected, and leading researchers in the field of MBCT were contacted to identify further relevant studies. Duplicates were removed from the total number of identified records. Abstracts from the remaining records were screened to retrieve full-text articles for assessment of eligibility. Studies fulfilling inclusion criteria were selected for meta-analytic evaluation. The retrieval process was checked by authors.
A data extraction sheet was developed for participant
characteristics (including age, sex, baseline anxiety score, and medication), group characteristics (including intervention, comparison condition, number of group participants and dropouts, and use of non-study treatments for anxiety within groups), and diagnosis and therapeutic characteristics (including diagnostic classification system, length of sessions and therapy period).
The methodological quality of studies was assessed using the revised Jadad scale based on six criteria: (1) the study was described as randomised; (2) the randomisation procedure was described and appropriate, ie, study participants were randomly allocated independent of the investigators “by methods allowing each participant to have the same chance of receiving each intervention”; (3) blind outcome assessments were reported (blindness of participants and therapists, as required by the original Jadad criteria, are not possible); (4) the blinding method was appropriate, (5) the number and reasons of withdrawals and dropouts were provided for each group, and (6) there was a description of inclusion/exclusion criteria. One point was assigned for each of the six fulfilled criteria; the maximum Jadad score was 6. Disagreements between raters were resolved by discussion.
Statistical analyses were conducted using the STATA (version 16). Forest plot statistics and a funnel plot of individual study effect sizes were used for detecting potential biases in the publication of study results.
Results
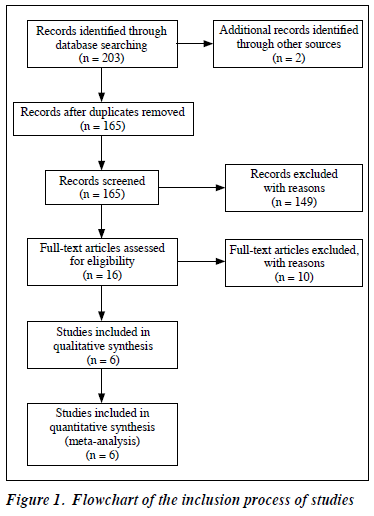
The flowchart for the inclusion process of studies is shown in Figure 1. The title and methodology of each eligible study were independently assessed. Of 203 papers evaluated, 197 were excluded owing to repetition (n = 38), MBCT not being used or no inclusion criteria (n = 149), or not conducted specifically for GAD (n = 10). The remaining six studies that compared the effectiveness between MBCT and controls were included for analysis.14,15,17-20
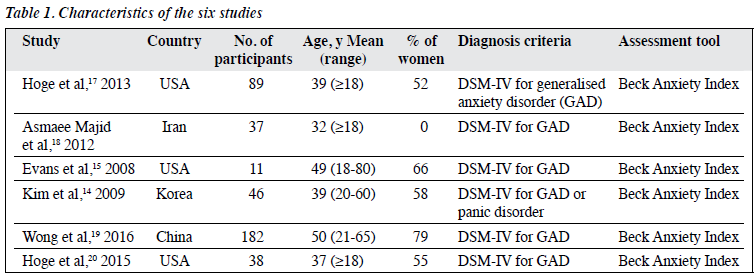
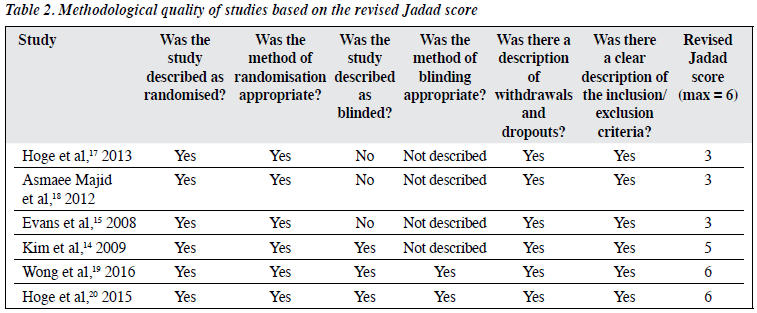
Among the six studies, the sample sizes ranged from 11 to 182; the mean age of participants ranged from 32 to 50 years; and percentage of women ranged from 0% to 79% (Table 1). The assessment tool used was the Beck Anxiety Index. The diagnosis of GAD was made according to the DSM-IV. The mean revised Jadad score of the six studies was 4.3 (range, 3-6) [Table 2].
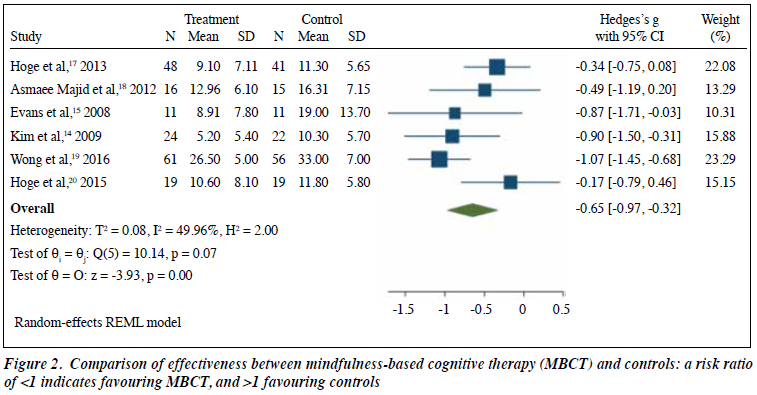
Effect sizes (Hedge’s g) and weights of six studies are shown in Figure 2. The overall sample size was 403. Effect sizes varied from -0.017 to -1.07, with an overall mean of -0.65 (95% confidence interval, -0.97 to -0.32; z = -3.93, p = 0.001). Heterogeneity was considerable (I2 = 49.96). This effect (d = 0.65) was significant (p < 0.001) and can be considered as a good effect indicating that the finding is robust. The fail-safe N analysis indicated that 14 missing equal sample size studies with no effect of MBCT compared with controls (ie, a risk ratio of 1.0) would be needed to reduce the overall risk of relapse effect size to a non- significant level (p > 0.05). The funnel plot of effect sizes in relation to the effect size standard error had a symmetrical distribution (Figure 3).
Discussion
In the present meta-analysis, the overall risk ratio for GAD in MBCT versus controls was 0.65, which indicates that MBCT is an effective intervention for GAD. The methodological quality of the six studies was high, with a mean revised Jadad score of 4.3. There was no evidence of publication bias according to tests of funnel plot. Fourteen missing studies of comparable sample size with an effect size of zero would be needed to nullify the result. Therefore, this meta-analysis is considered credible. Evidence of heterogeneity between individual studies can be neglected because of vast cultural differences between countries of studies.
A study of the effect of MBCT on GAD reported significant improvement in pathological concerns, stress, quality of life, and a number of other symptoms that remained after treatment, although the effect size on the improvement of pathologic concerns was very small.21 In MBCT, owing to the awareness exercises and being in the moment as well as awareness of physical sensations and psychological sensations, participants realise that when they are anxious, their heart rate and respiration changes. By MBCT, participants focus their attention on their body and thus increase the awareness of the body, feelings, and thoughts associated with anxiety, which increases the sense of symptom controllability, leading to anxiety reduction.
MBCT is effective in the treatment of GAD by integrating elements of philosophy, dialectics, mindfulness, acceptance, and communication, and taking advantage of mediating as a pivotal domain, as well as focusing on attention control in the treatment.22
The present study has some limitations. The number of studies included was small. The quality and type of methodology of the studies differed. In some studies, the MBCT group was compared with the non-intervention group, whereas in other studies, the MBCT group was compared with other-treatment group. This complicated the analysis and limited the power of results.23 In addition, the present study did not report the required data in the studies. In case of no access to full paper, the abstracts of studies were excluded. There was no access to some information sources and some required papers.
Conclusion
MBCT was effective for treating GAD.
Declaration
The authors have no conflict of interest to disclose.
References
- Shihata S, McEvoy PM, Mullan BA. Pathways from uncertainty to anxiety: an evaluation of a hierarchical model of trait and disorder- specific intolerance of uncertainty on anxiety disorder symptoms. J Anxiety Disord 2017;45:72-9. Crossref
- Narimani M, et al. Prevalence of generalized anxiety disorder and gender differences in the prevalence of generalized anxiety disorder. Fourth International Psychosomatic Congress. 2012. Isfahan, Islamic Azad University, Khorasgan Branch.
- Vandad Sharifi M, Amin-Esmaeili M, Hajebi A, et al. Twelve-month prevalence and correlates of psychiatric disorders in Iran: the Iranian Mental Health Survey, 2011. Arch Iran Med 2015;18:76-84.
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-5). 2013. Crossref
- Comer JS, Olfson M, Mojtabai R. National trends in child and adolescent psychotropic polypharmacy in office-based practice, 1996-2007. J Am Acad Child Adolesc Psychiatry 2010;49:1001-10. Crossref
- Revicki DA, Travers K, Wyrwich KW, et al. Humanistic and economic burden of generalized anxiety disorder in North America and Europe. J Affect Disord 2012;140:103-12. Crossref
- Clark DA, Beck AT. Cognitive Therapy of Anxiety Disorders: Science and Practice. Guilford Press: 2011.
- Mennin DS, Heimberg RG, Turk CL. Clinical presentation and diagnostic features. In: Heimberg RG, Turk CL, Mennin DS, editors. Generalized Anxiety Disorder: Advances in Research and Practice. Guilford Press: 2004: 3-28.
- School of Health and Related Research (ScHARR), University Studies of Sheffield. Clinical Guidelines for the Management of Anxiety: Management of Anxiety (Panic Disorder, with or without Agoraphobia, and Generalised Anxiety Disorder) in Adults in Primary, Secondary and Community Care. London: National Collaborating Centre for Primary Care (UK); 2004.
- Roy-Byrne PP, Craske MG, Stein MB, et al. A randomized effectiveness trial of cognitive-behavioral therapy and medication for primary care panic disorder. Arch Gen Psychiatry 2005;62:290-8. Crossref
- Fava GA, Ruini C, Rafanelli C, et al. Well-being therapy of generalized anxiety disorder. Psychother Psychosom 2005;74:26-30. Crossref
- Arch JJ, Ayers CR, Baker A, Almklov E, Dean DJ, Craske MG. Randomized clinical trial of adapted mindfulness-based stress reduction versus group cognitive behavioral therapy for heterogeneous anxiety disorders. Behav Res Ther 2013;51:185-96. Crossref
- Sharma MP, Mao A, Sudhir PM. Mindfulness-based cognitive behavior therapy in patients with anxiety disorders: a case series. Indian J Psychol Med 2012;34:263-9. Crossref
- Kim YW, Lee SH, Choi TK, et al. Effectiveness of mindfulness- based cognitive therapy as an adjuvant to pharmacotherapy in patients with panic disorder or generalized anxiety disorder. Depress Anxiety 2009;26:601-6. Crossref
- Evans S, Ferrando S, Findler M, Stowell C, Smart C, Haglin D. Mindfulness-based cognitive therapy for generalized anxiety disorder. J Anxiety Disord 2008;22:716-21. Crossref
- Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med 2009;6:e1000100. Crossref
- Hoge EA, Bui E, Marques L, et al. Randomized controlled trial of mindfulness meditation for generalized anxiety disorder: effects on anxiety and stress reactivity. J Clin Psychiatry 2013;74:786-92. Crossref
- Asmaee Majid S, Seghatoleslam T, Homan H, Akhvast A, Habil H. Effect of mindfulness based stress management on reduction of generalized anxiety disorder. Iran J Public Health 2012;41:24-8.
- Wong SY, Yip BH, Mak WW, et al. Mindfulness-based cognitive therapy v. group psychoeducation for people with generalised anxiety disorder: randomised controlled trial. Br J Psychiatry 2016;209:68-75.Crossref
- Hoge EA, Bui E, Goetter E, et al. Change in decentering mediates improvement in anxiety in mindfulness-based stress reduction for generalized anxiety disorder. Cognit Ther Res 2015;39:228-35. Crossref
- Craigie MA, Rees CS, Marsh A, Nathan P. Mindfulness-based cognitive therapy for generalized anxiety disorder: a preliminary evaluation. Behav Cogn Psychother 2008;36:553-68. Crossref
- Bayrami M, Movahedi Y, Alizadeh GJ. The effectiveness of cognition- based mindfulness therapy on the reduction of social anxiety and dysfunctional attitude in adolescents. Soc Cogn 2015;4:41-52.
- Gould RA, Safren SA, O’Neill Washington D, Otto MW. A meta- analytic review of cognitive-behavioral treatments. In: Heimberg RG, Turk CL, Mennin DS, editors. Generalized Anxiety Disorder: Advances in Research and Practice. New York: Guildford Publications; 2004.