East Asian Arch Psychiatry 2017;27:63-70
ORIGINAL ARTICLE
Dr Vincent M. C. Leung, FHKCPsych, FHKAM (Psychiatry), Department of Psychiatry, Shatin Hospital / Prince of Wales Hospital, Shatin, Hong Kong SAR, China.
Ms L. F. Chan, MHealthMan, MNurs, Department of Psychiatry, Shatin Hospital / Prince of Wales Hospital, Shatin, Hong Kong SAR, China.
Address for correspondence: Dr Vincent M. C. Leung, Psychiatric Department, Shatin Hospital / Prince of Wales Hospital; Honorary Clinical Assistant Professor, Department of Psychiatry, Faculty of Medicine, The Chinese University of Hong Kong, Shatin, Hong Kong SAR, China.
Email: lmc027@ha.org.hk
Submitted: 14 September 2016; Accepted: 5 May 2017
Abstract
Objectives: To examine the prevalence, co-morbidities, and correlates of attention-deficit hyperactivity disorder (ADHD) among adult patients who attended the Li Ka Shing psychiatric outpatient clinic (LKSPC), Hong Kong.
Methods: This study was a cross-sectional cohort study of patients consecutively referred to LKSPC over a 3-month period for evaluation of adult ADHD in 2 phases. In the screening phase, the Adult ADHD Self-Report Scale–v1.1 (ASRS-v1.1) Screener and Symptom Checklist and Sheehan Disability Scale (SDS) were used in the evaluation. In the interview phase, ADHD diagnosis was ascertained using the Diagnostic Interview for ADHD in Adults, version 2.0 (DIVA 2.0), with the DSM-5 criteria, in patients who exceeded the cut-off point of either the ASRS-v1.1 Screener or Symptom Checklist.
Results: The study included 254 patients of whom 49 were diagnosed with ADHD. Patients with ADHD were aged 18 to 60 (mean, 40.1) years, and 63.3% were women. The estimated prevalence of ADHD in adult psychiatric patients, by sensitivity analysis, was 13% to 19.3% with a higher prevalence in men than women (24.7% vs. 17.1%). Adult ADHD was highly co-morbid with substance / alcohol use disorders and forensic record, and associated with functional impairment. In the ADHD combined presentation group, there was additional co-morbidities of bipolar disorder, active substance use and chronic alcohol use, and a higher associated risk of suicidal attempt.
Conclusions: Efforts are needed to increase the detection and treatment of adult ADHD that affects a relevant proportion of our adult psychiatric outpatient population, and was associated with adverse social outcomes and functional impairment.
Key words: Attention deficit disorder with hyperactivity; Comorbidity; Hong Kong; Prevalence
Introduction
Attention-deficit hyperactivity disorder (ADHD) is a persisting pattern of inattention and / or hyperactivity- impulsivity that interferes with functioning or development. The worldwide prevalence of ADHD in the adult population has been reported to be 4.4%, a level only slightly less than the 5.3% estimated worldwide prevalence in children.1
The meta-analysis study from Faraone et al2 indicated that around two thirds of children with ADHD continue to have impairing levels of ADHD symptoms as an adult. Furthermore, ADHD has been associated with a number of co-morbid psychiatric disorders, such as mood, anxiety, and substance use disorders, and higher rates of suicidal attempts and criminality.3-5 Nonetheless a US-based study showed that about 50% of patients with ADHD had obtained treatment for other co-morbid mental and substance-related disorders and only about 10% had received treatment for ADHD.6 Prevalences of ADHD among adult psychiatric outpatient samples, applying DSM-IV-TR criteria, have been estimated to be 15.9%, 16.8% and 22% in Turkey, Mexico and North East England, respectively.7-9 A multinational cross-sectional study in Europe, based on Diagnostic Interview for ADHD in Adults (DIVA) and applying DSM-5 criteria, revealed that 17.4% of outpatients were diagnosed with ADHD.10
To the best of our knowledge, there has been no local study of the prevalence of ADHD among adult psychiatric outpatients. Nonetheless there is growing awareness that undiagnosed and untreated ADHD can result in several negative impacts on the individual’s life as well as society.11 Knowledge of the prevalence of ADHD in the adult outpatient psychiatric clinic can enable clinicians to treat the ADHD as well as co-morbid conditions, and also to consider ADHD a possible differential diagnosis. The present study aimed to examine the prevalence of ADHD in adult psychiatric outpatients and to compare the socio-demographic characteristics, DSM-5 Axis I-II co- morbidities, correlates, and functional impairments in those with and without ADHD.
Methods
This was a cross-sectional cohort study of adult patients aged between 18 and 64 years seen at the Li Ka Shing psychiatric outpatient clinic (LKSPC) of Prince of Wales Hospital, Hong Kong between 12 March 2015 and 17 June 2015. This study was approved by the Joint Chinese University of Hong Kong–New Territories East Cluster Clinical Research Ethics Committee. Informed and written consent was obtained from all participants. Patients were excluded if they refused to give informed consent, had major neurological disease, or could not understand and complete the questionnaires. During the recruitment period, patients were identified at the registration counter when they recorded their first attendance at the LKSPC. Subsequently, their electronic medical notes were scrutinised with the help of a case report form with regard to socio-demographic data, correlates, and the DSM-5 Axis I-II disorder diagnoses, according to the usual standards of clinical practice at LKSPC, i.e. all new outpatients’ history and mental state examination were entered electronically into a standardised admission summary template of the psychiatric clinical information system, and all admission summaries were later reviewed by the corresponding supervising consultant psychiatrist.
The participants were evaluated for a diagnosis of ADHD in 2 phases. In the screening phase, on their first visit to LKSPC, participants were asked to complete the following 3 self-report questionnaires before seeing their clinician: (1) Adult ADHD Self-Report Scale–v1.1 (ASRS-v1.1) Screener and Symptom Checklist (traditional Chinese version)12; (2) childhood symptoms and family history enquiries: 2 dichotomous yes-or-no questions on the experience of any one of the symptoms covered by the ASRS-v1.1 Symptom Checklist before the age of 12 years, and the family history of ADHD; and (3) Sheehan Disability Scale (SDS) in Cantonese Chinese version.13
The ASRS-v1.1 is an 18-item self-report scale based on the symptom list of the DSM-IV, developed by the Workgroup on Adult ADHD in conjunction with the World Health Organization. Six of the 18 questions, found to be the most predictive of ADHD, captured abnormalities in domains related to follow-through, procrastination, organisation, memory, restlessness, and hyperactivity over the past 6 months. This screening tool has performed well in studies with a sensitivity of 68.7%, specificity of 99.5%, and total classification accuracy of 97.9%.14 A positive screen according to the ASRS screener requires at least 4 of 6 responses to exceed the threshold.
For the 18-item ASRS-v1.1 Symptom Checklist (traditional Chinese version), physicians were instructed to ask respondents about the presence of any ADHD symptoms from the checklist during their childhood, and any associated dysfunction(s) in their daily life. A positive screen required a combination of 3 entities in our study: (1) inattention or hyperactivity / impulsivity symptoms subscale score of ≥ 17 over the past 6 months; (2) retrospective report of any one of the ADHD symptoms from the Checklist before the age of 12 years as captured by a positive answer to the dichotomous yes-or-no question of the childhood symptoms enquiry; and (3) functional impairment as identified by any SDS subscale score of ≥ 5 indicating impairment in that subscale area of the SDS.
The SDS was a self-rated questionnaire designed to measure the extent to which a patient’s illness- or health problem–related disability caused changes in performance at work / school, family life / home responsibilities, or social life / leisure activities. Responses for each item ranged from 0 to 10 and higher values indicated greater disruption. The 3 items were summed to give a single dimensional measure of global functional impairment that ranged from 0 (unimpaired) to 30 (highly impaired). A psychometric evaluation study of the SDS in adult patients with ADHD supports the use of SDS subscales and the total score in the ADHD population.15
In the interview phase, the ADHD diagnosis was ascertained using the DIVA 2.0,16 according to the DSM-5 criteria, in patients who exceeded the cut-off point for either the ASRS-v1.1 Screener or Symptom Checklist. The DIVA 2.0 is a semi-structured interview that encompasses childhood and adult DSM-IV symptoms for ADHD, and provides examples of impairments usually associated with the symptoms in 5 areas of everyday life for each age-group: education / work; family life / relationship; social contacts; free time / hobbies; and self-image / self-confidence. As far as possible, the DIVA 2.0 was completed with the patient in the presence of a partner, friend or family member, to ascertain the retrospective and collateral information. Information received via telephone from patients and their informants were also accepted if they were unavailable for in-person interview.
Statistical Analyses
Statistical analyses were performed using SPSS (Windows version 20.0; IBM Corp, Armonk [NY], US). The Chi- square test and the Fisher’s exact test were used to compare categorical data, the t test or analysis of variance for continuous data, and the linear regression test to determine any correlation. All p values were 2-tailed, and statistical significance was set at p < 0.05.
Results
Patient Characteristics
Of 376 outpatients seen at the LKSPC during the recruitment period and approached to participate in the study, 254 (67.6%) were consented and included. Respondents were aged 18 to 64 (mean, 42) years and 71.3% were women. Non- respondents (mean age, 44.8 years) were significantly older than respondents (p = 0.04) but were not statistically different to the non-ADHD group (mean, 42.6 years) [p = 0.11]. There was no significant difference in gender among the respondents, non-respondents, or non-ADHD groups. Of the 254 respondents included in the study, 94 (37.0%) screened positive for ADHD, 78 (30.7%) by ASRS Screener and 16 (6.3%) by ASRS Symptom Checklist. Among them, 3 (all with a negative childhood history of ADHD symptoms and without significant difference to the non-ADHD group) were either lost to follow-up or refused the DIVA 2.0 interview, and were therefore assigned to the non-ADHD group.
Prevalence of Attention-deficit Hyperactivity Disorder
Based on the DIVA 2.0 (using DSM-5 criteria), 19.3% (95% confidence interval [CI], 18.9%-19.7%) of all participating patients had ADHD. The prevalence rate, by sensitivity analysis, assuming all non-respondents to be non-ADHD as there were no significant differences in gender or age distribution between the non-respondents and the non-ADHD group, was estimated to lie between 13% and 19.3%. Patients with ADHD aged from 18 to 60 years (mean, 40.1 years) and 63.3% were women. The prevalence of ADHD in men was greater (24.7% [95% CI, 24.3%- 25.1%]) compared with women (17.1% [95% CI, 16.7%- 17.5%]). The majority of these patients (51.0%) exhibited predominantly inattentive presentation, 40.8% combined presentation, and 8.2% hyperactive-impulsive presentation. A larger proportion of patients with ADHD combined presentation (70%) displayed all criteria of DSM-5 symptoms when compared with predominantly inattentive (52%) and hyperactive-impulsive presentations (50%). Of the 49 patients with ADHD, only 15 (30.6%) received the diagnosis of ADHD from the clinician, 1 (2.0%) had been diagnosed and treated since childhood, and 10 (20.4%) reported a family history of ADHD that was in accordance with a familial rate of ADHD.17
Psychiatric Diagnoses and Correlates
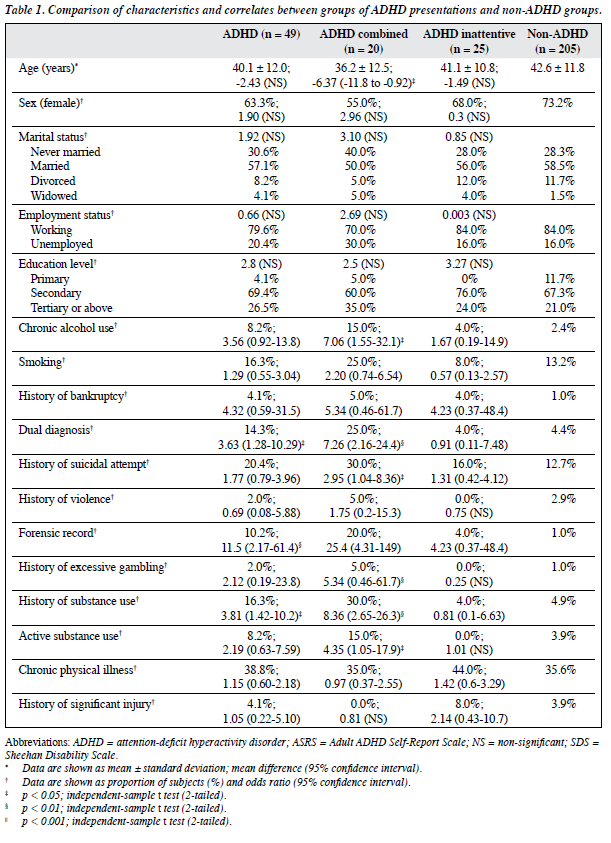
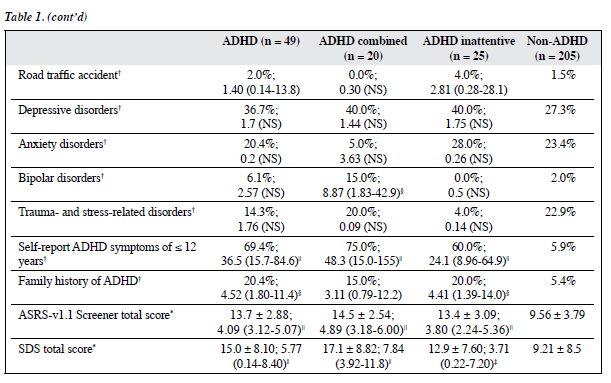
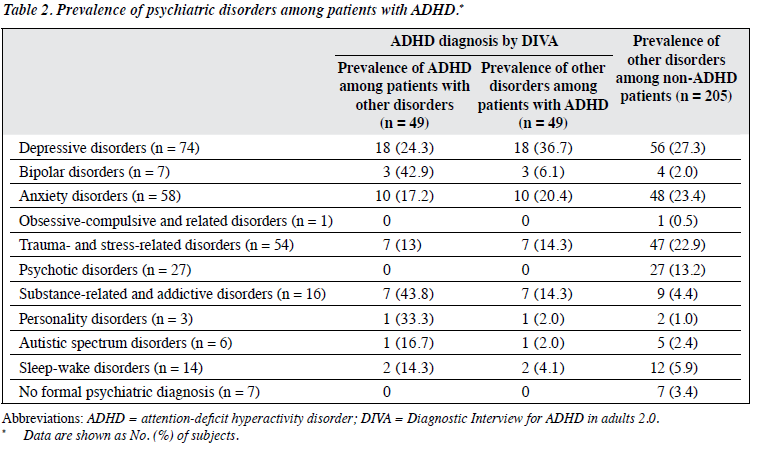
The ADHD and non-ADHD groups did not differ in age, gender, marital or employment status, or education level as shown in Table 1. Differences between groups in the assessed features were likely the result of demographic differences. The most common type of co-morbid psychiatric disorder among patients with ADHD, as shown in Table 2, was depression (36.7%) followed by anxiety disorder (20.4%), trauma- and stress-related disorders (14.3%), substance- related and addictive disorder (14.3%), and bipolar disorder (6.1%).
In the present study, several factors demonstrated a higher prevalence in the ADHD group compared with the non-ADHD group: chronic alcohol use (8.2% vs. 2.4%), cigarette smoking (16.3% vs. 13.2%), history of bankruptcy (4.1% vs. 1%), history of suicidal attempt (20.4% vs. 12.7%), forensic record (10.2% vs. 1%), problematic gambling (2% vs. 1%), history of substance use (16.3% vs. 4.9%), active substance use (8.2% vs. 3.9%), dual diagnosis (14.3% vs. 4.4%), childhood symptoms of ADHD (69.4% vs. 5.9%), family history of ADHD (20.4% vs. 5.4%), and higher risks (odds ratio [OR]) for forensic record (11.5 [95% CI, 2.2-61.4]), history of substance use (3.8 [95% CI, 1.4- 10.2]), dual diagnosis (3.6 [95% CI, 1.3-10.3]), childhood symptoms of ADHD (36.5 [95% CI, 15.7-84.6]), and family history of ADHD (4.5 [95% CI, 1.8-11.4]) [Table 1]. When comparisons were made between the ADHD combined presentation and the non-ADHD groups, the former was additionally associated with a higher risk of chronic alcohol use (OR = 7.06, 95% CI, 1.55-32.1), history of suicidal attempt (2.95, 1.04-8.36), active substance use (4.35, 1.05- 17.9), and bipolar disorder (8.87, 1.83-42.9).
The mean ASRS-v1.1 Screener total score was higher in ADHD combined presentation group (14.5) than those with predominantly inattentive presentation (13.4), hyperactive-impulsive presentation (11.5), and non-ADHD (9.56). Spearman’s correlation coefficient was 0.41.
The mean SDS total scores for the ADHD combined presentation, predominantly inattentive presentation, hyperactive-impulsive presentation and the non-ADHD groups were 17.1, 12.9, 17.5 and 9.2, respectively. The ADHD combined presentation group, by one-way analysis of variance test, had a significantly higher level of functional impairment compared with the non-ADHD group. The mean total SDS scores for ADHD-full-criteria, ADHD-in-partial-remission, and non-ADHD groups were 15.03, 14.90 and 9.21, respectively. The 2 former groups displayed a greater degree of functional impairment than the non-ADHD group, but no significant difference was noted between the 2 ADHD groups.
Discussion
This study had 2 main aims: first, to estimate the prevalence of ADHD among new referrals to a psychiatric outpatient clinic; second, to explore the correlates and co-morbidities of ADHD in our sample population. The prevalence of ADHD in the present study was between 13% and 19.3%, comparable with results of previous studies.7-9 With the prevalence in the general population reported to be about 4.4%, a 3- to 4-fold higher prevalence of ADHD in a psychiatric outpatient clinic is not unexpected. The male-to-female prevalence ratio in the present study was 1.4:1, comparable with the 1.6:1 in a US-based National Comorbidity Survey6 and the ORs found in studies of children and adolescents.18 It revealed that childhood ADHD was no more likely to persist into adulthood among girls than boys.19 Nonetheless the higher proportion of women in the adult ADHD group might be due to differences in readiness to seek help or recognition bias.20 In addition, the ADHD combined presentation group (mean age, 36.2 years) was significantly younger than the non-ADHD group (mean age, 42.6 years). This might be because the former group is more willing to seek help after being distressed by their co- morbidities and functional impairments. The most common presentation of ADHD in our sample was predominantly inattentive presentation (51%), compatible with the finding of a meta-analytic review that the most common form of ADHD in the general adult population is of the inattentive type.21 For global functional impairment, fewer symptoms in the partial remission group did not coincide with better functioning as shown by previous study.22
In this study, 98% of the participants with ADHD (two thirds were female) had not received a prior diagnosis or treatment of ADHD. This confirms the results from previous studies that less than half of children who fulfil the DSM-IV ADHD criteria had a prior diagnosis of ADHD or regular medication treatment.23 In addition, girls, who have less disruptive hyperactive ADHD symptoms than boys, were less likely than boys, who have higher total psychiatric morbidity, to be identified and referred for assessment.24,25
Children with mainly inattention problems were more likely to be referred for intensive remedial care at school rather than for child psychiatry service.26 Previous studies suggest that their care pathway may be influenced by the parents’ decision to seek care and their knowledge of ADHD.27-29 The level of mental health literacy in the general public, especially among adolescents, and mental health service utilisation have been shown by local studies to remain suboptimal.30,31
Efforts are needed to safeguard the children and adolescents from suffering due to mental health problems.
In the present study, depressive disorder was found to be the most common DSM-5 Axis I co-morbidity in the ADHD group, and there were reports that 16% to 31% of adults with ADHD had depressive disorder.32,33 Moreover, the rate of co-morbid bipolar disorder was higher in the ADHD combined presentation group (OR = 8.9, p = 0.001), comparable with the result of the US National Comorbidity Survey (OR = 7.4).6 Consistent with similar findings from a recent study that examined suicidal behaviour in 51,707 patients with an ADHD diagnosis (OR = 3.62-5.9),4 we also found a higher rate of suicidal attempt among the ADHD combined presentation group (OR = 2.95). Patients with ADHD combined presentation seemed to be at greater suicide risk, perhaps because of an increased level of impulsivity.34 Nonetheless the relationship between ADHD and suicide risk might also be modified by the co-morbid depressive disorder, bipolar disorder, active substance use, or chronic alcohol use as observed in the present study. In the context of suicide prevention, it is important to observe for these co-morbidities among patients with ADHD combined presentation.
Similar findings from a recent follow-up study of ADHD combined type from childhood to young adulthood showed that substance use and police contact were more common among patients with ADHD.35 A higher rate of co- morbid dual diagnoses (substance / alcohol use disorders) among the ADHD group (OR = 3.6) in our study also replicated similar findings from the US National Comorbidity Survey (OR = 3.0).6 In the present study, we also examined previous and active use of substance separately, and the rates of both active substance use and chronic alcohol use were found to be higher in the ADHD combined presentation group but not among the other 2 presentations. Similar findings from a previous study showed that the number of inattention and hyperactivity / impulsivity symptoms exhibited was positively correlated with risk of substance use.36 It is therefore imperative to observe for incipient substance / alcohol use among patients with ADHD and, conversely, to screen for co-morbid ADHD among patients with substance / alcohol use disorders. In the present study, the higher rate of forensic record (OR = 11.5) among the ADHD group might be an adverse social outcome from the impulsivity, sensation seeking, and boredom of untreated ADHD that may lead to poor judgement37 or self-medication with illicit drugs. The relationship between untreated ADHD and criminality cannot be overemphasised since previous study has shown that ADHD medications can reduce the risk of criminality among patients with ADHD by 32% in men and 41% in women.38
Strengths and Weaknesses
The present study results should be interpreted in the context of its limitations and strengths. First, we could not draw any conclusions about causality with this observational study. In other words, we do not know if ADHD directly caused the detected co-morbidities or simply complicated the existing mental illnesses. Second, the response rate of 67.6% limited the generalisability of the ADHD prevalence rate to other psychiatric outpatient clinics, although there were no significant differences in gender and age between the non- respondents and the non-ADHD group, and the sensitivity analysis of the prevalence rate was made conservatively based on this observation to avoid overestimation. Third, recall bias, especially for ADHD patients with forgetfulness and distractibility, was unavoidable as the screening questionnaires and the diagnostic interview were both based on self-report, and 30% of patients with ADHD, on their own, failed to recall any childhood ADHD symptoms in the first instance. Unlike childhood ADHD, informant assessment and documentations were less likely to be available for adults, and previous study comparing adult self-report and informant reports of ADHD symptoms indicate underestimation in self-reports by adults as in those by children.39 Therefore, our prevalence estimate was probably conservative even though efforts were made to gather collateral information. Fourth, although the ASRS was a very sensitive screening instrument and a negative screen on recall of any experience of symptoms from the ASRS Symptom Checklist before the age of 12 years further reduced the chance of false negatives, the ADHD diagnosis could still be missed as those negatively screened
participants were not further tested with DIVA 2.0. If this study is replicated, negatively screened participants could be re-examined with the ASRS 6 months later so that they would be more likely to be screened out after their co-morbid psychiatric symptoms, which might have previously masked their ADHD symptoms in the first instance, had subsided. Fifth, in regard to a substance use disorder, the present study employed a simplification of reality as many patients used multiple substances and there was no clear distinction between primary and non-primary substance of abuse from the case notes review. Nonetheless information on previous and current substance use was obtained separately and allowed us to reveal the higher risk of active substance use in the ADHD combined presentation group. Sixth, the DIVA 2.0 was the English version. A validated Chinese version was not yet available at the time for clinical or research use. Although the ASRS Mandarin Chinese version was easily understood by our patients, a Cantonese Chinese version could help improve its validity and reliability for local use, especially by ADHD patients with deficits in attention and follow-through.
The current study was unique methodologically in employing both ASRS-v1.1 Screener and Symptom Checklist in the screening phase, and in adding a dichotomous yes-or-no follow-up question to enquire about the presence of any symptoms covered by the ASRS before the age of 12 years in order to comply with the instructions of the ASRS Symptom Checklist that determined presence of ADHD symptoms in childhood rather than over the past 6 months only. This manoeuvre could help discriminate those false-positive overlapping symptoms from other mental disorders of adult onset as the ASRS could be over-sensitive when used in a psychiatric outpatient clinic rather than the general population or a general outpatient clinic.
In conclusion, a relevant proportion of the adult psychiatric outpatients had ADHD that was shown to be associated with adverse psychosocial outcomes of forensic record and substance abuse, more suicidal attempts complicating existing mental disorders, and impairment of an individual’s global functioning. Further research is required to determine whether ADHD treatment can affect the severity and persistence of co-morbid disorders, and whether dysfunction in daily life is related to the executive dysfunction of ADHD.
Acknowledgments
We would like to thank all the patients who participated in this study. Our appreciation also goes to the nursing and support staff of LKSPC for their assistance in data collection. Finally, we would like to thank Ms Mandy Yu from Department of Psychiatry, The Chinese University of Hong Kong, as well as Dr CM Leung and Dr W Lin of LKSPC, for their invaluable advice on our study.
Declaration
All authors have disclosed no conflicts of interest.
References
- Polanczyk G, de Lima MS, Horta BL, Biederman J, Rohde LA. The worldwide prevalence of ADHD: a systematic review and metaregression analysis. Am J Psychiatry 2007;164:942-8.
- Faraone SV, Biederman J, Mick E. The age-dependent decline of attention deficit hyperactivity disorder: a meta-analysis of follow-up studies. Psychol Med 2006;36:159-65.
- Fayyad J, De Graaf R, Kessler R, Alonso J, Angermeyer M, Demyttenaere K, et al. Cross-national prevalence and correlates of adult attention-deficit hyperactivity disorder. Br J Psychiatry 2007;190:402-9.
- Ljung T, Chen Q, Lichtenstein P, Larsson H. Common etiological factors of attention-deficit / hyperactivity disorder and suicidal behavior: a population-based study in Sweden. JAMA Psychiatry 2014;71:958-64.
- Young S, Moss D, Sedgwick O, Fridman M, Hodgkins P. A meta- analysis of the prevalence of attention deficit hyperactivity disorder in incarcerated populations. Psychol Med 2015;45:247-58.
- Kessler RC, Adler L, Barkley R, Biederman J, Conners CK, Demler O, et al. The prevalence and correlates of adult ADHD in the United States: results from the National Comorbidity Survey Replication. Am J Psychiatry 2006;163:716-23.
- Duran Ş, Fistikci N, Keyvan A, Bilici M. Prevalence and co morbidity of adult ADHD in psychiatric outpatient admissions. Eur Psychiatry 2013;28(Suppl 1):1.
- Almeida Montes LG, Hernández García AO, Ricardo-Garcell J. ADHD prevalence in adult outpatients with nonpsychotic psychiatric illnesses. J Atten Disord 2007;11:150-6.
- Rao P, Place M. Prevalence of ADHD in four general adult outpatient clinics in North East England. Prog Neurol Psychiatry 2011;15:7-10.
- Deberdt W, Thome J, Lebrec J, Kraemer S, Fregenal I, Ramos-Quiroga JA, et al. Prevalence of ADHD in nonpsychotic adult psychiatric care (ADPSYC): a multinational cross-sectional study in Europe. BMC Psychiatry 2015;15:242.
- Garcia CR, Bau CH, Silva KL, Callegari-Jacques SM, Salgado CA, Fischer AG, et al. The burdened life of adults with ADHD: impairment beyond comorbidity. Eur Psychiatry 2012;27:309-13.
- Adler LA, Kessler RC, Spencer T. Adult ADHD Self-Report Scale (ASRS-v1.1) symptom checklist. New York, NY: World Health Organization; 2003.
- Sheehan DV. The anxiety disease. New York, NY: Charles Scribner’s Sons; 1984.
- Kessler RC, Adler L, Ames M, Demler O, Faraone S, Hiripi E, et al. The World Health Organization Adult ADHD Self-Report Scale (ASRS): a short screening scale for use in the general population. Psychol Med 2005;35:245-56.
- Coles T, Coon C, DeMuro C, McLeod L, Gnanasakthy A. Psychometric evaluation of the Sheehan Disability Scale in adult patients with attention-deficit / hyperactivity disorder. Neuropsychiatr Dis Treat 2014;10:887-95.
- Kooij JJ, Francken MH. Diagnostic Interview for ADHD in adults 2.0 (DIVA 2.0). DIVA Foundation, The Netherlands; 2010.
- Faraone SV, Biederman J, Monuteaux MC. Toward guidelines for pedigree selection in genetic studies of attention deficit hyperactivity disorder. Genet Epidemiol 2000;18:1-16.
- Scahill L, Schwab-Stone M. Epidemiology of ADHD in school-age children. Child Adolesc Psychiatr Clin N Am 2000;9:541-55, vii.
- Biederman J, Faraone SV, Monuteaux MC, Bober M, Cadogen E. Gender effects on attention-deficit / hyperactivity disorder in adults, revisited. Biol Psychiatry 2004;55:692-700.
- Arcia E, Conners CK. Gender differences in ADHD? J Dev Behav Pediatr 1998;19:77-83.
- Willcutt EG. The prevalence of DSM-IV attention-deficit / hyperactivity disorder: a meta-analytic review. Neurotherapeutics 2012;9:490-9.
- Biederman J, Mick E, Faraone SV. Age-dependent decline of symptoms of attention deficit hyperactivity disorder: impact of remission definition and symptom type. Am J Psychiatry 2000;157:816-8.
- Froehlich TE, Lanphear BP, Epstein JN, Barbaresi WJ, Katusic SK, Kahn RS. Prevalence, recognition, and treatment of attention-deficit / hyperactivity disorder in a national sample of US children. Arch Pediatr Adolesc Med 2007;161:857-64.
- Martényi F, Zheng Y, Huang YS, Lee YS, Walton R, Harrison G, et al. A prospective observational study of attention-deficit hyperactivity disorder in Asia: baseline characteristics of symptom severity and treatment options in a paediatric population. East Asian Arch Psychiatry 2010;20:76-86.
- Gau SS, Chong MY, Chen TH, Cheng AT. A 3-year panel study of mental disorders among adolescents in Taiwan. Am J Psychiatry 2005;162:1344-50.
- Lau V, Liu S, Lee F. Attention deficit/hyperactivity disorder — An epidemiological study in Hong Kong from 2003 to 2009. Brainchild 2012;13:5-11.
- So CY, Leung PW, Hung SF. Treatment effectiveness of combined medication / behavioural treatment with Chinese ADHD children in routine practice. Behav Res Ther 2008;46:983-92.
- Ho SW, Chien WT, Wang LQ. Parents’ perceptions of care-giving to a child with attention deficit hyperactivity disorder: an exploratory study. Contemp Nurse 2011;40:41-56.
- Xiang YT, Luk ES, Lai KY. Quality of life in parents of children with attention-deficit-hyperactivity disorder in Hong Kong. Aust N Z J Psychiatry 2009;43:731-8.
- Siu BW, Chow KK, Lam LC, Chan WC, Tang VW, Chui WW. A questionnaire survey on attitudes and understanding towards mental disorders. East Asian Arch Psychiatry 2012;22:18-24.
- Lam LC, Wong CS, Wang MJ, Chan WC, Chen EY, Ng RM, et al. Prevalence, psychosocial correlates and service utilization of depressive and anxiety disorders in Hong Kong: the Hong Kong Mental Morbidity Survey (HKMMS). Soc Psychiatry Psychiatr Epidemiol 2015;50:1379-88.
- Fischer AG, Bau CH, Grevet EH, Salgado CA, Victor MM, Kalil KL, et al. The role of comorbid major depressive disorder in the clinical presentation of adult ADHD. J Psychiatr Res 2007;41:991-6.
- Biederman J, Faraone SV, Spencer T, Wilens T, Norman D, Lapey KA, et al. Patterns of psychiatric comorbidity, cognition, and psychosocial functioning in adults with attention deficit hyperactivity disorder. Am J Psychiatry 1993;150:1792-8.
- Young S. Forensic aspects of ADHD. In: Fitzgerald M, Bellgove M, Gill M, editors. Handbook of attention deficit hyperactivity disorder. New York, NY: John Wiley & Sons; 2007: 91-108.
- Cadman T, Findon J, Eklund H, Hayward H, Howley D, Cheung C, et al. Six-year follow-up study of combined type ADHD from childhood to young adulthood: predictors of functional impairment and comorbid symptoms. Eur Psychiatry 2016;35:47-54.
- Gudjonsson GH, Sigurdsson JF, Sigfusdottir ID, Young S. An epidemiological study of ADHD symptoms among young persons and the relationship with cigarette smoking, alcohol consumption and illicit drug use. J Child Psychol Psychiatry 2012;53:304-12.
- Murphy KR, Barkley RA, Bush T. Young adults with attention deficit hyperactivity disorder: subtype differences in comorbidity, educational, and clinical history. J Nerv Ment Dis 2002;190:147-57.
- Lichtenstein P, Halldner L, Zetterqvist J, Sjölander A, Serlachius E, Fazel S, et al. Medication for attention deficit-hyperactivity disorder and criminality. N Engl J Med 2012;367:2006-14.
- Zucker M, Morris MK, Ingram SM, Morris RD, Bakeman R. Concordance of self- and informant ratings of adults’ current and childhood attention-deficit / hyperactivity disorder symptoms. Psychol Assess 2002;14:379-89.