East Asian Arch Psychiatry 2017;27:56-62
ORIGINAL ARTICLE
Dr T. S. Jaisoorya, MD, MRCPsych, DCP (Irl), Department of Psychiatry, National Institute of Mental Health and Neurosciences, Bangalore, India.
Dr G. Desai, MD, DNB, PhD, Department of Psychiatry, National Institute of Mental Health and Neurosciences, Bangalore, India.
Dr K. V. Beena, MBBS, MPH, National Rural Health Mission (Kerala), Thiruvananthapuram, Kerala, India.
Dr M. Beena, MBBS, State Mission Director, National Rural Health Mission (Kerala), Thiruvananthapuram, Kerala, India.
Dr K. Ellangovan, MBBS, MS, Department of Health & Family Affairs (Kerala), Thiruvananthapuram, Kerala, India.
Prof. K. Thennarasu, PhD, Department of Health & Family Welfare, Government of Kerala, India.
Address for correspondence: Dr T. S. Jaisoorya, Department of Psychiatry, National Institute of Mental Health and Neurosciences, Bangalore, India.
Tel: (91) 9495600084; Email: tsjaisoorya@gmail.com
Submitted: 20 June 2016; Accepted: 25 February 2017
Abstract
Objective: There are limited data on the prevalence and correlates of psychological distress among adolescents in India. This study assessed psychological distress among adolescents who attended school in Kerala, India.
Methods: A total of 7560 students from 73 schools, aged 12 to 19 years completed a self-administered questionnaire that included Kessler Psychological Distress Scale and other standardised instruments to assess various domains.
Results: Mild psychological distress was reported by 10.5%, moderate distress by 5.4%, and severe distress by 4.9% of students. Older age, not living with both parents, and urban residence were significantly associated with psychological distress (p < 0.05). Students who experienced psychological distress had a higher risk of reporting academic failure, alcohol and tobacco use, suicidality, and sexual abuse. Increasing severity of psychological distress was associated with higher odds of these correlates.
Conclusions: Psychological distress is common among adolescents and its correlates with negative outcomes suggest the need for early recognition and treatment.
Key words: Adolescent; India; Prevalence; Stress, psychological
Introduction
Adolescence is a period of transition associated with many challenges, both physical and psychological. Although the majority of adolescents overcome these challenges, there is a significant proportion who exhibit depression, anxiety, suicidality, and self-destructive behaviours.1
Mental health problems in adolescence have a significant impact on academic and social achievements, with negative consequences extending into adulthood. There is also evidence that a substantial proportion of mental health problems in adolescence persist into adulthood.2,3
Regional surveys in the US have shown that about 1 in every 3 to 4 children experience mental health problems and about 1 in 10 children have a serious emotional disturbance.4,5
The National Comorbidity survey–Adolescence from the US reported a 31.9% prevalence of anxiety disorders and 14.3% prevalence of mood disorders.6 In a review of mental health in young people aged 12 to 24 years across high-income countries, the prevalence of mental disorders assessed using structured instruments ranged from 8% in the Netherlands to 57% in California.7 Epidemiological studies of the prevalence of mental health problems among children and adolescents in low-middle-income countries (LMIC) have shown a prevalence of 10% to 20%.8
Depression and anxiety are the most common mental health problems among adolescents. Between 20% and 50% of adolescents self-report depressive symptoms with significant and regular co-occurrence of anxiety symptoms.9
This co-occurrence is often described as psychological distress and is associated with poor mental health that negatively impacts level of functioning.10 Previous Indian studies of non-specific psychological distress have reported prevalence rates between 13% and 45%.11 Despite the high prevalence rates, only about 1 in every 4 to 5 youths with psychological distress fulfil the criteria for a lifetime mental disorder that is associated with severe role impairment and / or distress.6
Various risk factors for psychological distress have been identified across studies. Increasing age and female gender are associated with higher rates of psychological distress.9,11,12 Poverty, family dysfunction, and social disadvantage have been strongly associated with psychological distress among adolescents.13-15 Violence, abuse, and academic stress have also been reported to increase the risk.11,12,16-18 Substance use including alcohol and tobacco is higher in adolescents who experience psychological distress.19,20 One of the distressing outcomes of psychological distress is suicide. Depression and dysthymia were associated with a 12-fold risk of suicidal attempts.21
In a large Indian study that evaluated the cause of death among those aged 10 to 19 years, suicide accounted for about a quarter of all deaths in males and between 50% and 75% in females,22 with another study from India reporting psychological distress to be independently associated with suicidal behaviour.17
India has the largest national population of adolescents (243 million) who comprise 21.4% of the total population.23
Previous studies of psychological distress and its correlates in India have been conducted among limited subjects. Structured assessments were used only for assessing stress, not its correlates.11 It is in this context that we examined the prevalence of psychological distress in a large sample of school-going adolescents along with key clinical correlates in the socio-demographic and psychological domains. Data for the study were collected as part of a larger study by the National Rural Health Mission, a government initiative to study psychological issues including substance use among school-going adolescents in the State of Kerala, India. Kerala, a state in southern India, is well known for its egalitarian policies in terms of health care, redistributive actions and social reforms, with its health and literacy indicators close to those of high-resource countries despite a poor per capita income.
Methods
This was a cross-sectional epidemiological survey conducted in a single division of Classes (year) 8, 10, and 12 of 73 schools in the District of Ernakulam of the State of Kerala, India. The schools were selected by cluster random sampling from the 168 high (classes up to year 10) and higher secondary schools (classes up to year 12) in the District. Most schools in India have a large number of students with multiple divisions in each school year / class with each division accommodating 40 to 45 students. In the selected schools, a single division was randomly selected for the survey.
The questionnaire was self-administered. School Junior Public Health Nurses (JPHNs) who had been trained were present to supervise the survey and clarify any doubts. To ensure privacy, students were seated sufficiently far apart so that they could complete their questionnaires without being overlooked by other students.
In addition to psychological distress, other domains assessed included the lifetime use of substances (alcohol and tobacco), suicidality, sexual abuse, and attention- deficit hyperactivity disorder (ADHD). In areas that were assessed, standardised instruments or parts of standardised instruments were identified. The questionnaire was initially prepared in English, translated into Malayalam (the vernacular language), and then back-translated to check for accuracy.
Ethical Considerations
Institutional ethical approval was received from the Government Medical College, Ernakulam and administrative approval was received from the school authorities prior to the survey. Information about the survey was provided to the parent-teacher association. Students were informed that the survey was anonymous and had no impact on their school work. The questionnaires were administered only to consenting students. Students who did not wish to take part could either leave the classroom (none did) or return the questionnaire unanswered, which constituted 3.1% of the total.
Students were also told that if they required any help with any of the issues surveyed, they could approach the School JPHNs who had received appropriate training. All student responses were anonymised so they could not be traced even if their responses indicated a need for intervention.
Assessment Tools
Socio-demographic profile (age, gender, area of residence, economic indicators, religion, academic performance) was assessed using a checklist. Several other assessments were also completed.
Psychological Distress
Psychological distress was assessed using Kessler Psychological Distress Scale (K10) that screens for non- specific psychological distress. The K10 is a 10-item questionnaire developed on the basis of item response theory models.24 This instrument has been widely used in population-based epidemiological studies including world mental health surveys to measure current (1-month) distress severity associated with psychological symptoms in the form of “how often in the past month did you feel...” and offer specific symptoms, such as ‘tired out for no good reason’, ‘nervous’, and ‘sad or depressed’. The 5 possible responses for each question ranged from ‘none of the time’ (score 1) to ‘all of the time’ (score 5). All the responses were collated to obtain a total score. A total score of < 20 was considered normal; 20-24 mild distress; 25-29 moderate distress; and 30-50 severe distress.25 The tool has been validated to screen for common mental disorders in developing countries,26 including India.27 The instrument has also been validated in an adolescent sample.28
Tobacco and Substance Use
For assessment of substance use, the ASSIST (Alcohol, Smoking and Substance Involvement Screening Test), a well-validated instrument developed by the World Health Organization was used.29,30 Only current use of alcohol and tobacco was considered in this study.
Suicidality
Two questions were asked to assess lifetime suicidality: (1) “Have you ever thought of killing yourself?” and (2) “Have you ever made an attempt to kill yourself?”
Sexual Abuse
Four questions regarding lifetime exposure to sexual abuse were taken from ISPCAN Child Abuse Screening Tool Children’s version,31 an instrument validated in India. Questions 1 and 2 are related to non-contact sexual abuse whereas questions 3 and 4 to contact sexual abuse:
- Has someone misbehaved with you sexually against your will?
- Has someone forced you to look at pornographic materials against your will?
- Has someone forced you to fondle or fondled you against your will?
- Has someone forced you into a sexual relationship against your will?
Statistical Analysis
The SPSS (Windows version 16.0; SPSS Inc., Chicago [IL], US) was used for analysis. The 1-month prevalence of psychological distress (mild / moderate / severe) in both genders was determined. As there is strong evidence of the co-occurrence of alcohol and psychological distress and its preponderance in males,20,32 the confounding effect of alcohol use was controlled to report gender differences in prevalence rates.
The socio-demographic variables and academic performance were compared between those who had psychological distress and those who had not, using Chi- square and Fisher’s exact tests, as necessary. Yates correction factor for Chi-square test was applied where appropriate. Substance use, suicidality, sexual abuse, and ADHD were compared between the psychological distress and non- psychological distress groups using logistic regression analysis. Odds ratios were calculated after controlling for socio-demographic variables that were significant. All tests were 2-tailed and statistical significance was set at p < 0.05.
Results
A total of 7560 (97.7%) of 7740 eligible students from 73 schools took part in the survey (the initial sample size calculated to identify 1% prevalence with 95% confidence interval with a 5% error and 50% response distribution was 3520). Of the questionnaires, 231 (3.1%) were discarded as they were incomplete and the rest (n = 7329) were analysed.
The mean (± standard deviation) age of the sample was 15.3 ± 1.7 years (range, 12-19 years). Mild psychological distress was reported by 768 (10.5%) students (374 males and 394 females), moderate distress by 397 (5.4%; 197 males and 200 females), and severe distress by 357 (4.9%; 179 males and 178 females). There was no gender difference in prevalence of psychological distress (p = 0.45). Nonetheless when the confounding effects of alcohol use were controlled, females had a significantly higher prevalence of psychological distress (p = 0.01).
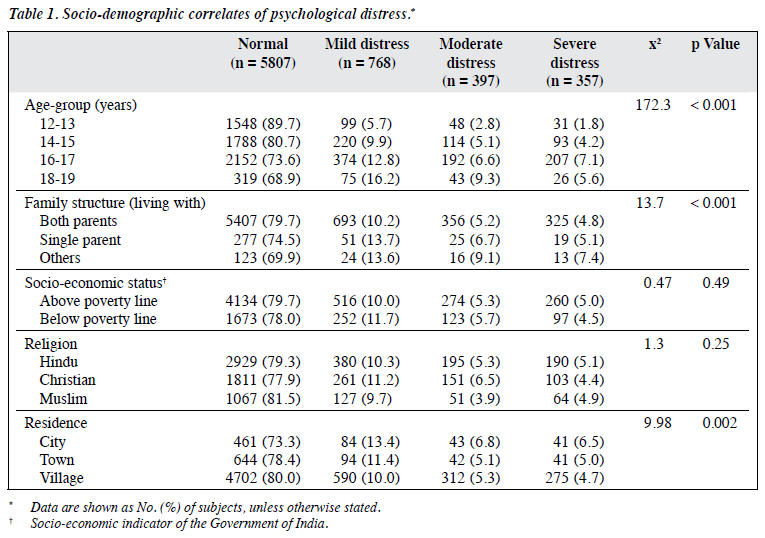
Table 1 shows the socio-demographic variables of the subjects. Older age, not living with both parents, and urban residence were significantly associated with psychological distress (p < 0.05). There was no significant association with socio-economic status or religion.
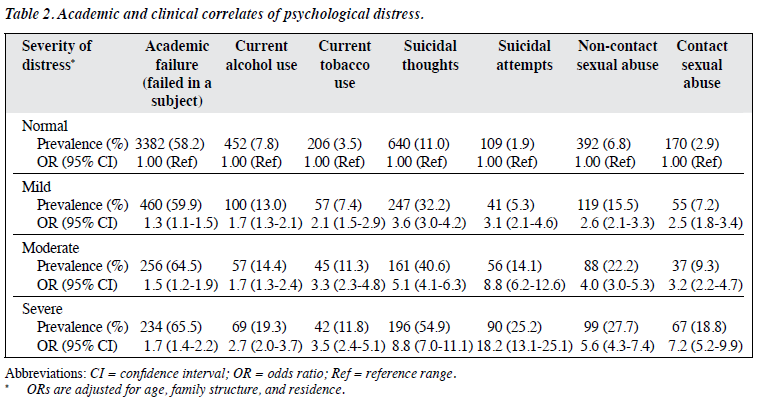
Students with psychological distress had a higher risk of reporting academic failure, current alcohol and tobacco use, suicidal thoughts, suicidal attempts, and contact or non-contact sexual abuse, even after controlling for socio- demographic variables that were significant (Table 2). Further, increasing severity of psychological distress was associated with higher odds of these correlates.
Discussion
This is one of the largest studies of the prevalence of psychological distress and its correlates from India among adolescent school students. Although psychological distress is not diagnostic for mental illness, it is useful for identifying symptoms that are associated with various psychological disorders (e.g. depressed mood, anxiety).33 Research has shown a strong association between a high score on the K10 and a current Composite International Diagnostic Interview diagnosis of anxiety and affective disorders.27
The prevalence of psychological distress in our sample was 20.8%, similar to prevalence rates reported in earlier studies. The prevalence reported from studies across high- income countries varies from 8% to 57%,7 and for LMIC from 10% to 20%.8 Studies from India have reported rates between 13% and 45%.11 The varying prevalence rates could be due to different methodological approaches, including varying definitions of psychological distress; clinical versus community samples; and different assessment measures (e.g. structured interviews, self-report, self-made items). The cultural contexts of expression of these problems and different exposures to risk and protective factors across countries have also been postulated as possible reasons for this variance.8
Increasing age positively correlated with psychological distress with distress increasing from 10.3% at the age of 12 to 13 years to 30.7% at the age of 18 to 19 years. The pattern of increasing prevalence in our study is similar to other results from India11 and across the world.9,13
Our study found a higher prevalence of psychological distress in females when the confounding effects of alcohol were controlled, replicating the consistent findings of previous studies.9,11 In Kerala, alcohol use among adolescent males was significantly higher compared with females (22.5% vs. 6.5%).32 The rate of co-morbidity for depression and alcohol use is among the highest for any combination of diagnoses for adolescents.34 Hence, its confounding effects owing to significantly higher differential distribution in the sample contributed to the lack of gender differences in prevalence in the initial uncontrolled analysis.
This study also replicated many of the previous findings with regard to the association of socio-demographic characteristics and psychological distress. In our study, students who lived with a single parent or with significant others, a possible indication of family dysfunction, had higher psychological distress. Family dysfunction has been linked to psychological distress in previous studies.14,15
Although the mechanisms underlying the impact of non- intact homes on psychological distress have not been delineated, current evidence suggests that a combination of genetic vulnerability and indirect influences on disruptions in the home environment play a role.35,36
Psychological distress was higher among adolescents residing in urban areas compared with rural areas. The findings from previous studies have been heterogeneous with studies reporting a higher prevalence in urban areas,37 rural areas,38 or no difference in prevalence rates.39 Socio-economic disadvantage was not associated with psychological distress in our study. Although most studies have shown that poverty increases psychological distress,13-15 others have reported no such link.1,40 The lack of strong and consistent findings with regard to many of the socio-demographic variables has been attributed to the significant interactions among several of these socio- demographic characteristics. This raises the possibility that all may have independent effects on the mental health of adolescents.
In this study students with academic failures had significantly higher psychological distress. This is further evidence of a strong and consistent association between adolescent mental health and academic achievement.11,41
Another consistent finding in our study was the co-occurrence of psychological distress and alcohol and tobacco use. There have been conflicting reports about how substance use and psychological distress influence each other. Studies have reported that individuals use various substances, including alcohol and tobacco, as ‘self- medication’ to alleviate psychological distress.42,43 Substance use has also been reported to lead to psychological distress due to its neurodepressant effects or via the increased risk of poor outcomes such as educational failure, unemployment, criminal arrests, and disruption of social relationships that characterise repeated alcohol use.44,45 Researchers have also reported that psychological distress and substance use share common aetiological factors, such as poverty, neighbourhood disadvantage, familial vulnerability, or behavioural problems leading to higher co-occurrence.46,47
In our study, subjects with psychological distress had more lifetime suicidal thoughts and suicidal attempts. Further, increasing severity of distress was associated with increased suicidality. More than 90% of adolescents who die by suicide have been diagnosed with at least one psychiatric disorder with multiple studies reporting depression and anxiety the most common.11,21,48
In our sample, students with psychological distress reported higher rates of both contact and non-contact sexual abuse. The relationship of sexual abuse and depression is quite robust with data suggesting that psychological distress is higher among subjects exposed to sexual abuse.49,50
Existing studies, however, also suggest that this relationship is not specific since borderline personality disorder, eating disorder, substance use, suicidal behaviours, and somatisation may develop as a consequence of sexual abuse.49-51 A causal relationship between sexual abuse and psychiatric disorder has not been substantiated as there are 2 alternative explanations for this association. The first, a shared familial, environmental, or temperamental structure may contribute both to the risk for sexual abuse and psychiatric disorder. Second, there is recall bias in those with a psychiatric disorder who are more prone to report or disclose sexual abuse.49-51
The co-occurrence of various psychiatric disorders with psychological distress in our adolescent students is similar to findings across the world. In our sample, increasing severity of psychological distress was associated with worsening odds of reporting negative outcomes. The high co-occurrence of psychological disorders in adolescence has been reported previously with the National Comorbidity Survey Replication reporting around 40% of adolescents with more than one class of lifetime disorder, and mood disorders the most likely to co-occur with other classes.6
Previous studies suggest that about 1 in every 4 to 5 youths fulfil the criteria for a lifetime mental disorder associated with severe role impairment and / or distress.6 Nonetheless in our sample, increasing severity of distress was associated with proportionately greater academic failure, suggesting that our students were either more impaired or that this issue requires further study.
The findings of the study should be interpreted in light of its limitations. Psychological distress and its correlates reported in this study are based only on students’ self- reported responses. No diagnostic interview was conducted. The consequent estimate of prevalence may not be accurate. We report non-specific symptoms of psychological distress and have not made a syndromal diagnosis. The cross- sectional design of the study precludes any conclusion about psychological distress and the correlates examined. The assessment of academic failure was not objective as it was defined by any failure in one subject. For assessment of suicidality, only lifetime suicidality was assessed, not current. Sexual abuse and suicidality were assessed using only selected questions from structured instruments. The findings from Kerala may not be generalised to students from other regions of India or other countries with different cultures. Nonetheless the strengths of our study include the assessment of a large sample, the use of structured instruments for assessment, and the reporting for the first time of many of the correlates in a community sample in India.
To conclude, psychological distress is common among adolescents in Kerala, India. The correlation of psychological distress with poor academic performance, substance use, suicidality, and exposure to sexual abuse suggests that adolescents with psychological distress are often exposed to a constellation of risks. These findings have important public health implications. India has a significant shortfall of mental health professionals and spending for mental health is just 0.06% of the total health budget.52
School mental health programmes in many states are non- existent. This study indicates an urgent need to sensitise health administrators, teachers, parents, and children to the problem of psychological distress among adolescents and should lead to the introduction of measures that will improve early recognition and treatment of adolescent mental health problems.
Acknowledgements
The study was partly funded by National Rural Health Mission (NRHM). The authors would like to thank the Junior Public Health Nurses and Block Public Relations Officers of NRHM (Ernakulam) who were involved in administering the questionnaire, as well as Mr Ajayakumar and his team who helped with data entry.
Declaration
All authors have disclosed no conflicts of interest.
References
- Merikangas KR, He JP, Brody D, Fischer PW, Bourdon K, Koretz DS. Prevalence and treatment of mental disorders among US children in 2001-2004 NHANES. Pediatrics 2010;125:75-81.
- Kessler RC, Angermeyer M, Anthony JC, DE Graaf R, Demyttenaere K, Gasquet I, et al. Lifetime prevalence and age-of-onset distributions of mental disorders in the World Health Organization’s World Mental Health Survey Initiative. World Psychiatry 2007;6:168-76.
- Kim-Cohen J, Caspi A, Moffitt TE, Harrington H, Milne BJ, Poulton R. Prior juvenile diagnoses in adults with mental disorder: developmental follow-back of a prospective-longitudinal cohort. Arch Gen Psychiatry 2003;60:709-17.
- Brauner CB, Stephen CB. Estimating the prevalence of early childhood serious emotional / behavioral disorders: challenges and recommendations. Public Health Rep 2006;121:303-10.
- Jane Costello E, Erkanli A, Angold A. Is there an epidemic of child or adolescent depression? J Child Psychol Psychiatry 2006;47:1263-71.
- Merikangas KR, He JP, Burstein M, Swanson SA, Avenevoli S, Cui L, et al. Lifetime prevalence of mental disorders in U.S. adolescents: results from the National Comorbidity Survey Replication–Adolescent Supplement (NCS-A). J Am Acad Child Adolesc Psychiatry 2010;49:980-9.
- Patel V, Flisher AJ, Hetrick S, McGorry P. Mental health of young people: a global public-health challenge. Lancet 2007;1369:1302- 13.
- Kieling C, Baker-Henningham H, Belfer M, Conti G, Ertem I, Omigbodun O, et al. Child and adolescent mental health worldwide: evidence for action. Lancet 2011;378:1515-25.
- Kessler RC, Avenevoli S, Ries Merikangas K. Mood disorders in children and adolescents: an epidemiologic perspective. Biol Psychiatry 2001;49:1002-14.
- Ridner SH. Psychological distress: concept analysis. J Adv Nurs 2004;45:536-45.
- Kumar V, Talwar R. Determinants of psychological stress and suicidal behavior in Indian adolescents: a literature review. J Indian Assoc Child Adolesc Ment Health 2014;10:47-68.
- Patel V, Andrew G. Gender, sexual abuse and risk behaviours in adolescents: a cross-sectional survey in schools in Goa. Natl Med J India 2001;14:263-7.
- Meltzer H, Gatward R, Goodman R, Ford T. Mental health of children and adolescents in Great Britain. Int Rev Psychiatry 2003;15:185-7.
- Patel V, Kleinman A. Poverty and common mental disorders in developing countries. Bull World Health Organ 2003;81:609-15.
- Prinstein MJ, Boergers J, Spirito A, Little TD, Grapentine WL. Peer functioning, family dysfunction, and psychological symptoms in a risk factor model for adolescent inpatients’ suicidal ideation severity. J Clin Child Psychol 2000;29:392-405.
- Briere J, Jordan CE. Violence against women: outcome complexity and implications for assessment and treatment. J Interpers Violence 2004;19:1252-76.
- Pillai A, Andrews T, Patel V. Violence, psychological distress and the risk of suicidal behaviour in young people in India. Int J Epidemiol 2009;38:459-69.
- Sansone RA, Songer DA, Miller KA. Childhood abuse, mental healthcare utilization, self-harm behavior, and multiple psychiatric diagnoses among inpatients with and without a borderline diagnosis. Compr Psychiatry 2005;46:117-20.
- Couwenbergh C, van den Brink W, Zwart K, Vreugdenhil C, van Wijngaarden-Cremers P, van der Gaag RJ. Comorbid psychopathology in adolescents and young adults treated for substance use disorders: a review. Eur Child Adolesc Psychiatry 2006;15:319-28.
- Zorick T. Psychiatric comorbidities in adolescent substance use disorders. In: Rosner R, editor. Clinical handbook of adolescent addiction. John Wiley & Sons; 2013: 88-98.
- Nock MK, Green JG, Hwang I, McLaughlin KA, Sampson NA, Zaslavsky AM, et al. Prevalence, correlates, and treatment of lifetime suicidal behavior among adolescents: results from the National Comorbidity Survey Replication Adolescent Supplement. JAMA Psychiatry 2013;70:300-10.
- Aaron R, Joseph A, Abraham S, Muliyil J, George K, Prasad J, et al. Suicides in young people in rural southern India. Lancet 2004;363:1117-8.
- United Nations (UN): Department of Economic and Social Affairs. World population prospects: The 2012 revision. Available from: http:// esa.un.org/wpp/. Accessed 20 May 2016.
- Kessler RC, Andrews G, Colpe LJ, Hiripi E, Mroczek DK, Normand SL, et al. Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychol Med 2002;32:959-76.
- Andrews G, Slade T. Interpreting scores on the Kessler Psychological Distress Scale (K10). Aust N Z J Public Health 2001;25:494-7.
- Kessler RC, Üstün TB. The WHO world mental health survey: global perspectives on the epidemiology of mental disorders. UK: Cambridge University Press; 2008.
- Patel V, Araya R, Chowdhary N, King M, Kirkwood B, Nayak S, et al. Detecting common mental disorders in primary care in India: a comparison of five screening questionnaires. Psychol Med 2008;38:221-8.
- Huang JP, Xia W, Sun CH, Zhang HY, Wu LJ. Psychological distress and its correlates in Chinese adolescents. Aus N Z J Psychiatry 2009;43:674-81.
- WHO ASSIST Working Group. The Alcohol, Smoking and Substance Involvement Screening Test (ASSIST): development, reliability and feasibility. Addiction 2002;97:1183-94.
- Humeniuk R, Ali R, Babor TF, Farrell M, Formigoni ML, Jittiwutikarn J, et al. Validation of the Alcohol Smoking and Substance Involvement Screening Test (ASSIST). Addiction 2008;103:1039-47.
- Zolotora AJ, Runyan DK, Dunne MP, Jain D, Péturs HR, Ramirez C, et al. ISPCAN Child Abuse Screening Tool Children’s Version (ICAST- C): instrument development and multi-national pilot testing. Child Abuse Negl 2009;33:833-41.
- Jaisoorya TS, Beena KV, Beena M, Ellangovan K, Jose DC, Thennarasu K, et al. Prevalence and correlates of alcohol use among adolescents attending school in Kerala, India. Drug Alcohol Rev 2016;35:523-9.
- Goldberg DP, Gater R, Sartorius N, Ustun TB, Piccinelli M, Gureje O, et al. The validity of two versions of the GHQ in the WHO study of mental illness in general health care. Psychol Med 1996;27:191-7.
- Brière FN, Rohde P, Seeley JR, Klein D, Lewinsohn PM. Comorbidity between major depression and alcohol use disorder from adolescence to adulthood. Compr Psychiatry 2014;55:526-33.
- Fergusson DM, Horwood LJ. The Christchurch health and development study: review of findings on child and adolescent mental health. Aus N Z J Psychiatry 2001;35:287-96.
- Shanahan L, Copeland W, Costello EJ, Angold A. Specificity of putative psychosocial risk factors for psychiatric disorders in children and adolescents. J Child Psychol Psychiatry 2008;49:34-42.
- Peen J, Schoevers RA, Beekman AT, Dekker J. The current status of urban-rural differences in psychiatric disorders. Acta Psychiatr Scand 2010;121:84-93.
- Kovess-Masféty V, Alonso J, de Graaf R, Demyttenaere K. A European approach to rural-urban differences in mental health: the ESEMeD 2000 comparative study. Can J Psychiatry 2005;50:926-36.
- Breslau J, Marshall GN, Pincus HA, Brown RA. Are mental disorders more common in urban than rural areas of the United States? J Psychiatr Res 2014;56:50-5.
- Ford T, Goodman R, Meltzer H. The relative importance of child, family, school and neighbourhood correlates of childhood psychiatric disorder. Soc Psychiatry Psychiatr Epidemiol 2004;39:487-96.
- Tan JB, Yates S. Academic expectations as sources of stress in Asian students. Soc Psychol Educ 2011;14:389-407.
- Danzo S, Connell AM, Stormshak EA. Associations between alcohol- use and depression symptoms in adolescence: examining gender differences and pathways over time. J Adolesc 2017;56:64-74.
- Mcgee R, Williams S. Does low self-esteem predict health compromising behaviours among adolescents? J Adolesc 2000;23:569- 82.
- Fothergill K, Ensminger ME, Doherty EE, Juon HS, Green KM. Pathways from early childhood adversity to later adult drug use and psychological distress: a prospective study of a cohort of African Americans. J Health Social Behav 2016;57:223-39.
- Conway KP, Swendsen J, Husky MM, He JP, Merikangas KR. Association of lifetime mental disorders and subsequent alcohol and illicit drug use: results from the National Comorbidity Survey– Adolescent Supplement. J Am Acad Child Adolesc Psychiatry 2016;55:280-8.
- Green KM, Doherty EE, Stuart EA, Ensminger ME. Does heavy adolescent marijuana use lead to criminal involvement in adulthood? Evidence from a multiwave longitudinal study of urban African Americans. Drug Alcohol Depend 2010;112:117-25.
- Staff J, Patrick ME, Loken E, Maggs JL. Teenage alcohol use and educational attainment. J Stud Alcohol Drugs 2008;69:848-58.
- Hawton K, Saunders KE, O’Connor RC. Self-harm and suicide in adolescents. Lancet 2012;379:2373-82.
- Lindert J, von Ehrenstein OS, Grashow R, Gal G, Braehler E, Weisskopf MG. Sexual and physical abuse in childhood is associated with depression and anxiety over the life course: systematic review and meta-analysis. Int J Public Health 2014;59:359-72.
- Chu DA, Williams LM, Harris AW, Bryant RA, Gatt JM. Early life trauma predicts self-reported levels of depressive and anxiety symptoms in nonclinical community adults: relative contributions of early life stressor types and adult trauma exposure. J Psychiatr Res 2013;47:23-32.
- Hankin BL. Depression from childhood through adolescence: risk mechanisms across multiple systems and levels of analysis. Curr Opin Psychol 2015;4:13-20.
- World Health Organization. Mental health atlas: Department of Mental Health and Substance Abuse. World Health Organization; 2011.