East Asian Arch Psychiatry 2012;22:49-56
ORIGINAL ARTICLE
Obesity in Multiracial Schizophrenia Patients Receiving Outpatient Treatment in a Regional Tertiary Hospital in Malaysia
马来西亚一所地区叁级医院接受门诊治疗的多种族精神分裂症 兼肥胖症患者
Dr A. Talib Norlelawati, MD, Department of Basic Medical Sciences, Faculty of Medicine, International Islamic University Malaysia, Malaysia.
Dr Abdullah Kartini, MD, MMed, Department of Psychiatry, Faculty of Medicine, International Islamic University Malaysia, Malaysia.
A/Prof. Musa Ramli, MD, MMed, Department of Psychiatry, Faculty of Medicine, International Islamic University Malaysia, Malaysia.
Dr Kuzaifah Norsidah, MD, PhD, Department of Basic Medical Sciences, Faculty of Medicine, International Islamic University Malaysia, Malaysia.
Dr Wan Sulaiman Wan Azizi, MD, PhD, Department of Basic Medical Sciences, Faculty of Pharmacy, International Islamic University Malaysia, Malaysia.
Prof. Abdul Razak Tariq, MBBS, FRCP, MD, Faculty of Pharmacy, International Islamic University Malaysia, Malaysia.
Address for correspondence: Dr A. Talib Norlelawati, Department of Basic Medical Sciences, Faculty of Medicine, International Islamic University Malaysia, 25200 Kuantan, Malaysia.
Tel: (60-9) 5716400; Fax: (60-9) 5716784; email: noleata@yahoo.com
Submitted: 26 January 2012; Accepted: 6 March 2012
Abstract
Objectives: Obesity is an issue of concern among patients with schizophrenia as it is a co-morbid condition that is closely related to metabolic syndrome. The present study assessed the correlation of body mass index with antipsychotic use among multiracial schizophrenia outpatients. The study also compared the patients’ body mass index with Malaysian Adult Nutrition Survey (MANS) data.
Methods: A total of 216 participants were recruited into a cross-sectional study conducted over 5 months, from December 2010 to April 2011. Body weight and height were measured using the standard methods. Demographic data and treatment variables were gathered through interview or review of the medical records.
Results: There were differences in mean body mass index between men and women (p = 0.02) and between Malay, Chinese and Indian races (p = 0.04). Stratified by sex, age, and race, the body mass index distributions of the patients were significantly different to those of the reference MANS population. The prevalence of obesity among patients was more than 2-fold greater than among the reference population in all variables. Although body mass index distribution was related to antipsychotic drugs (χ2 = 33.42; p = 0.04), obesity could not be attributed to any specific drug.
Conclusion: The prevalence of obesity among patients with schizophrenia was significantly greater than that in the healthy Malaysian population, and affects the 3 main races in Malaysia.
Key words: Antipsychotic agents; Body mass index; Obesity; Schizophrenia
摘要
目的:肥胖症是精神分裂症患者须关注的问题,因前者往往与代谢综合症密切相关。本研究评估不同种族的精神分裂症门诊病人其抗精神病药物使用与身体质量指数的相关性。研究也将上述患者的数据跟马来西亚成人营养调查(MANS)数据作比较。
方法:本横断面研究於2010年12月至2011年4月进行,共纳入216名参与者,并运用标準方法测量他们的体重和高度,以及透过会谈或病历回顾收集人口统计学数据和各种治疗变数。
结果:身体质量指数於性别上(p = 0.02)和种族上(马来人、华人和印度人)〔p = 0.04〕有显著分别。按性别、年龄和种族分析,这些参与者的身体质量指数跟MANS数据也显著不同。在所有变数上,这些患者的肥胖症现患率为MANS参与人口的2倍以上。虽然身体质量指数的分佈与抗精神病药物相关(χ2 = 33.42;p = 0.04),但後者并不会导致肥胖症。
结论:精神分裂症患者的肥胖症现患率较马来西亚健康人口为高,且影响当中3个主要种族。
关键词:抗精神病药物、身体质量指数、肥胖症、精神分裂症
Introduction
Obesity is a prevalent metabolic disorder affecting not only people in developed countries, but also those in developing countries including Malaysia. Obesity is often associated with high fat and calorie intake, and lack of physical activity. Among individuals with schizophrenia, there is considerable evidence to suggest a strong relationship between obesity and schizophrenia.1,2 The link between schizophrenia and obesity is not new. PubMed literature searches for all its available archives, using the terms ‘obesity’ and ‘schizophrenia’, found more than 700 articles, of which the earliest article was dated 1953. Interestingly, when the search terms were changed to ‘antipsychotic’ and ‘obesity’, more than 930 articles were retrieved, of which the first published article was dated 1956. The antipsychotics of concern before 1960 were mainly chlorpromazine and reserpine.
As was reported 10 years ago, obesity was almost 3 times more prevalent among schizophrenia patients than among healthy individuals in a western population.3 Even though the mean body mass index (BMI) was significantly higher among schizophrenia patients than among non- schizophrenia participants in the US during 1987 to 1996, the incremental trend was not specific to the introduction of atypical antipsychotic drugs at that time.4 Some of the factors that contribute to obesity in schizophrenia could be disease-related, the effect of antipsychotic medications, or a combination of both factors.5-7 Managing schizophrenia with second-generation antipsychotic drugs has been linked to a likelihood of gaining weight.8,9 One of the earliest studies on clozapine found that the body weight increased even in the early months of treatment.10
Obesity is a considerable clinical concern as it is one of the components of metabolic syndrome and an important risk factor for cardiovascular disease,11,12 which is among the main contributors to morbidity and mortality. In the presence of concomitant obesity, as well as an increase in the overall cost of treatment for schizophrenia patients, life expectancy is reduced.13 A previous study has also found that health-related quality of life was significantly reduced in schizophrenia patients.14 Fear of weight gain has also been blamed for non-compliance with schizophrenia medication,15 a repetitive cycle that generally worsens the prognosis for schizophrenia.
To the best of the authors’ knowledge, there is no previous study from Malaysia that compares the distribution of BMI between schizophrenia patients and the healthy population. This study was therefore done to assess the BMI status, antipsychotic use, and severity of obesity among schizophrenia patients receiving outpatient treatment at a regional hospital on the East coast of Malaysia, and to compare the data with the BMI status of the healthy adult Malaysian population.
The study hypothesised that the BMI distribution between schizophrenia patients and the healthy population stratified by race, sex, and age is significantly different. The study also hypothesised that there is a significant association between BMI distribution and antipsychotics used.
Methods
A cross-sectional study was started in December 2010 at the Psychiatry Clinic of Tengku Ampuan Afzan Hospital, Kuantan, Malaysia. Patients who attended for follow-up at the clinic were either from Kuantan (the state capital of Pahang) or referred from other districts in Pahang or from Kemaman (in Terengganu) for specialised psychiatric management. As far as possible, all schizophrenia patients attending the clinic were informed about the study, and were recruited if they agreed to participate and fulfilled the study inclusion criteria. All participants fulfilled the DSM-IV criteria for a diagnosis of schizophrenia, were older than 18 years, and were able to be interviewed and to sign written informed consent for study participation. In order to accumulate data from all schizophrenia patients attending the Psychiatry Clinic, the recruitment process only stopped when all potential participants had been notified in April 2011. Of 240 participants, 24 were excluded from further analyses due to incomplete information. In all, 216 schizophrenia patients were recruited.
Patients’ social and family histories were taken during the interview. Information about previous and current antipsychotic medications was gathered from the medical records. Body weight and height of each participant were measured using the standard methods. Height was measured to the nearest millimetre, with the participants standing upright and without shoes. Body weight was measured by using the standard clinic-calibrated weighing scale. The BMI was calculated based on the formulae of weight in kilograms per height in square metres (kg/m2). The World Health Organization (WHO) criteria16 were used to classify BMI and obesity into 3 classes of severity. Using similar criteria, obesity was defined as a BMI of > 30 kg/m2.
The data were then compared with the BMI distribution of more than 6000 participants in the latest Malaysian Adult Nutrition Survey (MANS) completed in 2003.17
Statistical Analyses
Data were analysed by the Statistical Package for the Social Sciences Windows version 17.0 (SPSS Inc., Chicago [IL], US). The prevalences of obesity and normal distribution of BMI were calculated using descriptive statistics. The BMI values were compared with the MANS data and the type of antipsychotic therapy currently received. Categorical variables were calculated using Chi-square test, while parametric variables were compared using Student’s t test or one-way analysis of variance (ANCOVA). The ANCOVA was conducted to assess the effect of sex, race, and type of antipsychotics on mean BMI, with age as the covariance. To compare the distribution of BMI between participants in the current study and the MANS data, Chi-square goodness-of-fit analysis was performed using an online interactive software.18 A p value of < 0.05 was taken to be statistically significant.
Results
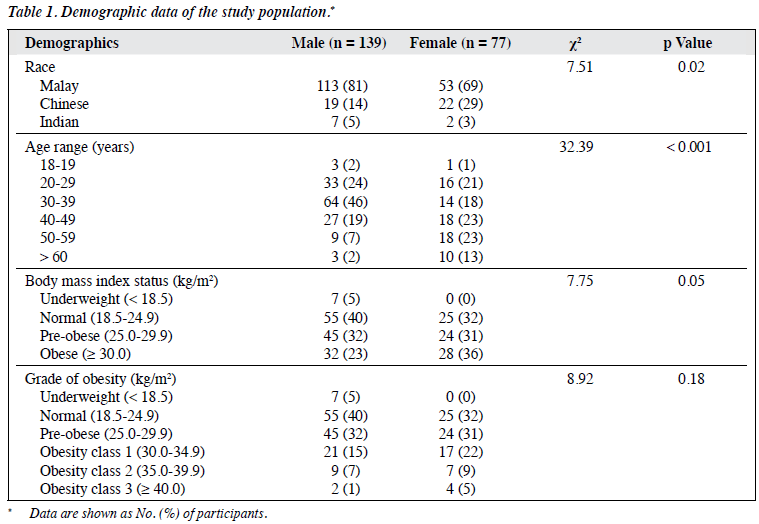
Of the 216 participants, 139 were male and 77 were female, with respective mean (± standard deviation [SD]) age of 36 ± 10 years and 43 ± 14 years. There were significant differences in racial representation; most were Malays (n = 166) followed by Chinese (n = 41) and Indians (n = 9) [Table 1]. The mean (± SD) BMI was 27.1 ± 6.4 kg/m2. A significant difference in mean BMI was noted between male (26.2 ± 5.7 kg/m2) and female (28.9 ± 7.1 kg/m2) participants (p = 0.02), as well as between the Malay (27.4 ± 6.6 kg/m2), Chinese (25.5 ± 4.2 kg/m2), and Indian races (30.0 ± 8.7 kg/m2) [p = 0.04]. The preliminary ANCOVA analysis evaluating the homogeneity of regression assumption indicated that there were no significant interactions between age (as the covariance) and the independent variables of sex, race, and type of antipsychotics (typical / atypical). The ANCOVA was significant for race (F = 6,262, p = 0.02), sex (F = 7.664, p = 0.01), and age (F = 9.444, p = 0.002), but not significant for the type of antipsychotics used (F = 0.322, p = 0.57). Pairwise comparison showed that the mean BMI of Chinese participants was significantly different to Malay (p = 0.03) and Indian (p = 0.05) participants, while no significant difference was found between Malay and Indian participants (p = 0.14).
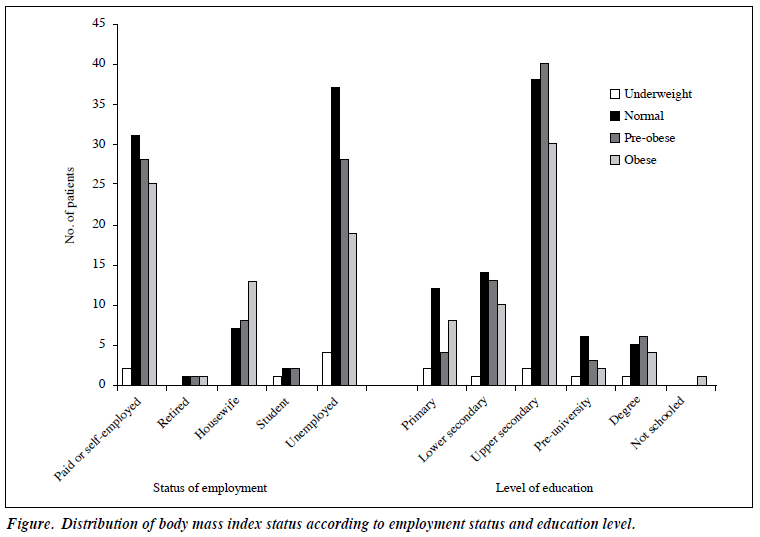
There were 60 (28%) obese participants (BMI ≥ 30.0 kg/m2) and 69 (32%) overweight or pre-obese participants (BMI, 25.0-29.9 kg/m2), or 59 (27%) and 93 (43%) participants, respectively, if the Malaysian Clinical Practice Guidelines on Management of Obesity19,20 definition was used for both conditions. The prevalence of obesity was significantly higher among women with schizophrenia (n = 28; 36%) than among men with schizophrenia (n = 32; 23%) [χ2 = 61.6, p < 0.001, degrees of freedom (df) = 1]. There were no significant differences between distribution of BMI and education status (χ2 = 12.2, p = 0.84; n = 204) and employment status (χ2 = 23.9, p = 0.93; n = 210) [Figure].
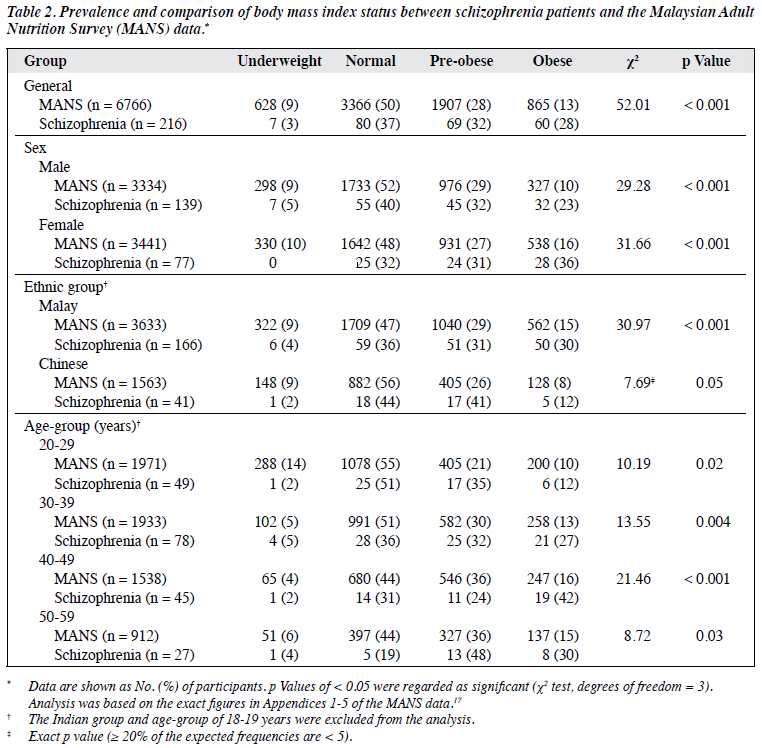
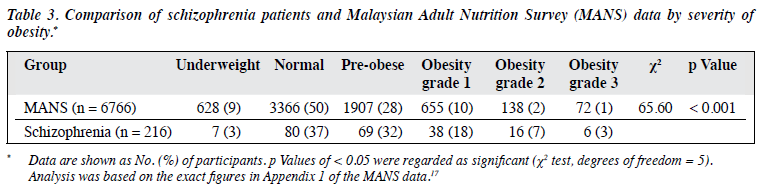
For comparison of BMI distribution among the different races, the Indian group (n = 9) was excluded as the number of participants was too small for significant statistical analyses. The age range of 18 to 19 years was also excluded from the analyses as the MANS data were not available for this group. Analysis of BMI distribution stratified by race, sex and age showed significant differences in BMI between the participants and the reference MANS population in all parameters. The prevalence of obesity among the study participants was more than 2-fold greater than the reference population in all variables (Table 2). There were highly significant differences in BMI distribution between the MANS population and schizophrenia patients if the data were further stratified based on obesity severity — grades 2 and 3 obesity were 3.5- and 3-fold greater than the reference population, respectively (Table 3).
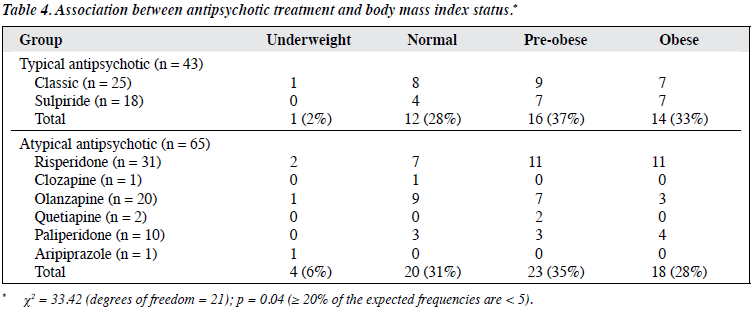
Of the 216 patients, data from 108 were selected for further analyses to look for an association between BMI status and antipsychotic treatment. The remaining patients (n = 108) were excluded from the analyses either because there was incomplete clinical information or because patients were taking more than 1 antipsychotic therapy (polypharmacy) or had been taking antipsychotic treatment for less than 6 months. Of the 108 patients, 31 (29%) received risperidone, followed by classic typical antipsychotics (n = 25, 23%), olanzapine (n = 20, 19%) or sulpiride (n = 18, 17%). A few patients received other atypical antipsychotics such as paliperidone (n = 10), quetiapine (n = 2), clozapine (n = 1) or aripiprazole (n = 1). Distribution of BMI status by type of antipsychotic therapy is shown in Table 4. There was a significant association between antipsychotic use and BMI status (χ2 = 33.42, p = 0.04, df = 21). There was no significant difference in the prevalence of obesity between patients treated with typical antipsychotics (n = 14 [33%]) and those treated with atypical antipsychotics (n = 18 [28%]; p = 0.59). There were also no significant differences in the prevalence of overweight and obesity between: (1) patients taking sulpiride (n = 14) and those taking other classic antipsychotics (n = 16) [p = 0.50]; (2) risperidone (n = 22) and other atypical antipsychotic drugs (n = 19) [p = 0.30]; and (3) olanzapine (n = 10) and other atypical antipsychotics (n = 31) [p = 0.17]. Even though the rates of overweight and obesity in patients treated with sulpiride (78%) and risperidone (71%) were higher than that in other antipsychotic drugs, these were not statistically significant (Table 4).
Discussion
The present study was done to compare the distribution of BMI between individuals with and without schizophrenia in the Malaysian population. The significant difference between the racial groups reflects the typical racial distribution on the East coast of Malaysia. Even though there were significant differences in mean BMI among the 3 racial groups, the cause of the differences could not be determined in this study. However, it is possible that certain genetic polymorphisms and cultural lifestyle play important roles in these differences. There is evidence that differences in susceptibility to obesity could be attributed to certain candidate genes21 that could be prevalent in some ethnic groups. Furthermore, obesity is considered a complex problem where environment / lifestyle typically plays a major role in its development.22 This study found that the mean BMI was highest among Indians, followed by Malays and Chinese. This finding contradicts the report of BMI measurement in the reference population, where Malays were found to have a higher BMI than Indians and Chinese.17 However, as the number of Indian participants was small (n = 9) in this study, their higher mean BMI could be misleading.
The demographic data also showed that the mean BMI of female schizophrenia patients was higher than that of the male counterparts, which is similar to the recent findings by Lee et al23 in an investigation into the gender differences among patients with schizophrenia in Singapore, a southern neighbour of Malaysia. There was a significant difference in the prevalence of obesity between men and women with schizophrenia, which is contradictory to the previous findings observed by Hsiao et al.24 Once diabetes occurs, women with schizophrenia and obesity are at a disadvantage with respect to cardiovascular risk.25 A study has shown that women with higher baseline BMI are predicted to be more prone to hypertension, as the BMI increase in obese women leads to a greater rise in systolic blood pressure than for men.26
As many as 13 studies have used different BMI criteria for predicting metabolic health risks,27 especially with regard to western and Asian populations due to their physical differences. There have been suggestions that the BMI range associated with metabolic diseases should be lower in Asian population than that in the European population.28,29 The current study used the cut-off criteria proposed by the WHO,16 as these criteria have been widely used among the Malaysian health community. Nevertheless, by using the BMI cut-off values proposed by the Malaysian Clinical Practice Guidelines on Management of Obesity,19,20 the cumulative prevalence of obesity and overweight among the schizophrenia population in the current study of 70% is comparable to the prevalence obtained by Ainsah et al30 in urban Kuala Lumpur of 74%. This indicates that socio- economic and lifestyle differences in urban and suburban areas are probably not important determinants of obesity in schizophrenia patients. By using the Malaysian cut-off values and population-specific BMI criteria, the prevalence of obesity in this study is higher than that in 3 other populations including Canada,3 Taiwan,24 and Japan.31 The prevalence of obesity among the Japanese patients was the lowest at 31%, even though the study used stringent BMI cut-off criteria of ≥ 25 kg/m2 for a definition of obesity31; the prevalence in Canada was 42% (BMI ≥ 30 kg/m2),3
Malaysia was 43%17 (BMI > 27.5 kg/m2), and Taiwan was 39% (BMI > 26.4 kg/m2).24 It is assumed that the higher prevalence of obesity among the schizophrenia patients in Malaysia compared with other races follows the trend of obesity among the healthy Malaysian population. A study of 16,127 healthy Malaysian participants found that the prevalence of obesity is very high, i.e. about 13% for those aged ≥ 20 years. This figure for obesity is 280% higher than the last Malaysian National Health and Morbidity Survey in 1996.32 In contrast, the prevalence of obesity in the Japanese population is remarkably low at 3.5%.33
In addition, comparisons of sex, race, and age showed that the BMI distribution between schizophrenia patients and the reference population was highly significantly different for all factors, except among Chinese participants (Table 2). This study is in agreement with previous studies in which significant differences in BMI distribution between healthy populations and schizophrenia patients were found.3,24,31 The prevalence of obesity in schizophrenia patients was more than 2-fold higher than that in the reference population. The current study reaffirmed the results of previous studies in other populations,3,24,31 showing that obesity was very prevalent among schizophrenia patients, and was significantly higher than that in the healthy reference populations.
There are several possibilities for the increased likelihood of obesity among schizophrenia patients. It has been mentioned that poor dietary habits, sedentary lifestyles, and antipsychotic medication may be responsible for weight gain among schizophrenia patients, resulting in obesity-related morbidity and mortality.34 There have also been suggestions that symptoms such as paranoia and some negative symptoms like apathy and social withdrawal may independently contribute to obesity in schizophrenia patients.35 This study found no suggestive link between type of schizophrenia and BMI status. In the general population, obesity has also been typically related to higher carbohydrate intake, and thus could be inferred to occur in people with good financial status. This study found no significant relationship between BMI and employment status. Nevertheless, it was noted that there was a higher proportion of obesity among housewives (13 / 28, 46%) than among participants with other employment status (Fig). In the general population, obesity has been associated with level of educational attainment, as shown in a UK study that the prevalence of obesity was higher among individuals who achieved fewer qualifications.36 A study in 972 Malaysian women also found a significant relationship between obesity and level of education.37 However, no significant relationship between education level and obesity was found in the current study. This non-significant finding could be attributed to the cognitive impairment that normally accompanies schizophrenia.38
The importance of antipsychotic medication as therapy for schizophrenia is undeniable. Nevertheless, there is legitimate acceptance that antipsychotic treatment is the root of obesity among patients with chronic schizophrenia, which is an issue of concern as obesity is a co-morbid condition that is closely related to cardiovascular disease and type 2 diabetes mellitus.39,40 There is consensus that both typical and atypical antipsychotic drugs induce obesity,41,42 although clozapine and olanzapine (both atypical antipsychotics) have the highest potential.8
Although the current study found a higher prevalence of obesity among the schizophrenia patients than among the reference population, no differences were noted on the prevalence of obesity between those who received typical or atypical antipsychotic drugs. The atypical antipsychotic drugs of choice for monotherapy in this study were risperidone, followed by olanzapine. The prevalence of obesity with both drugs was no different than with the other antipsychotics, although this could be misleading as the representation from other groups of atypical antipsychotics, including clozapine, was marginal. It is believed that the likelihood of weight gain in patients receiving antipsychotic treatment was due to interactions of the drugs with H1- histamine receptor affinity.43 It was suggested that the newer atypical antipsychotic drugs such as ziprasidone and aripiprazole, which have low H1-histamine receptor affinity, are less likely to cause weight gain.43 Neither of these drugs were used by the obese participants in this study, while only 1 patient of normal weight used clozapine, a potent antipsychotic for treatment-resistant schizophrenia that is highly correlated with weight gain.
There were various limitations to the present study. The use of a cross-sectional method of investigation was not sufficient to conclude any causal relationship between antipsychotic use and obesity. In addition, some important data such as antipsychotic dose and duration of use were not accounted for in the statistical analysis due to the difficulties in obtaining consistent data. Furthermore, confounding factors for obesity such as diet and lifestyle are difficult to assess and were not investigated in this study.
In conclusion, although the current study was limited by its small sample size and simple cross-sectional method of data collection, it has objectively shown that the prevalence of obesity among schizophrenia patients was greater than that in the general population, and affected the 3 main races in Malaysia, thus supporting the findings of iatrogenic pharmacotherapy as a common cause of obesity.
Acknowledgement
With grateful thanks to Dr Norazlina Abd Rahman and Dr Jamaludin Abdul Rahman for statistical advice, and to Dr Ahmad Zafri Abu Bakar and the staff of the Psychiatry Clinic, Tengku Ampuan Afzan Hospital, Kuantan for their help with this study. This study was supported by IIUM Endowment Grant: EDW B1002-365.
References
- Thakore JH, Mann JN, Vlahos I, Martin A, Reznek R. Increased visceral fat distribution in drug-naïve and drug-free patients with schizophrenia. Int J Obes Relat Metab Disord 2002;26:137-41.
- Aronne LJ. Epidemiology, morbidity, and treatment of overweight and obesity. J Clin Psychiatry 2001;62 Suppl 23:13-22.
- Coodin S. Body mass index in persons with schizophrenia. Can J Psychiatry 2001;46:549-55.
- Homel P, Casey D, Allison DB. Changes in body mass index for individuals with and without schizophrenia, 1987-1996. Schizophr Res 2002;55:277-84.
- Brown S, Birtwistle J, Roe L, Thompson C. The unhealthy lifestyle of people with schizophrenia. Psychol Med 1999;29:697-701.
- Theisen FM, Linden A, Geller F, Schäfer H, Martin M, Remschmidt H, et al. Prevalence of obesity in adolescent and young adult patients with and without schizophrenia and in relationship to antipsychotic medication. J Psychiatr Res 2001;35:339-45.
- Henderson DC, Borba CP, Daley TB, Boxill R, Nguyen DD, Culhane MA, et al. Dietary intake profile of patients with schizophrenia. Ann Clin Psychiatry 2006;18:99-105.
- Allison DB, Mentore JL, Heo M, Chandler LP, Cappelleri JC, Infante MC, et al. Antipsychotic-induced weight gain: a comprehensive research synthesis. Am J Psychiatry 1999;156:1686-96.
- Goudie AJ, Cooper GD, Halford JC. Antipsychotic-induced weight gain. Diabetes Obes Metab 2005;7:478-87.
- Leadbetter R, Shutty M, Pavalonis D, Vieweg V, Higgins P, Downs M. Clozapine-induced weight gain: prevalence and clinical relevance. Am J Psychiatry 1992;149:68-72.
- Isomaa B, Almgren P, Tuomi T, Forsén B, Lahti K, Nissén M, et al. Cardiovascular morbidity and mortality associated with the metabolic syndrome. Diabetes Care 2001;24:683-9.
- Galassi A, Reynolds K, He J. Metabolic syndrome and risk of cardiovascular disease: a meta-analysis. Am J Med 2006;119:812-9.
- Chwastiak LA, Rosenheck RA, McEvoy JP, Stroup TS, Swartz MS, Davis SM, et al. The impact of obesity on health care costs among persons with schizophrenia. Gen Hosp Psychiatry 2009;31:1-7.
- Kolotkin RL, Corey-Lisle PK, Crosby RD, Swanson JM, Tuomari AV, L’italien GJ, et al. Impact of obesity on health-related quality of life in schizophrenia and bipolar disorder. Obesity (Silver Spring) 2008;16:749-54.
- Weiden PJ, Mackell JA, McDonnell DD. Obesity as a risk factor for antipsychotic noncompliance. Schizophr Res 2004;66:51-7.
- World Health Organization. Global database on body mass index: BMI classification. World Health Organization website: http://apps.who.int/ bmi/. Accessed 15 August 2011.
- Azmi MY, Junidah R, Siti Mariam A, Safiah MY, Fatimah S, Norimah AK, et al. Body mass index (BMI) of adults: findings of the Malaysian Adult Nutrition Survey (MANS). Malays J Nutr 2009;15:97-119.
- Preacher KJ. Calculation for the chi-square test: an interactive calculation tool for chi-square tests of goodness of fit and independence (computer software). Website: http://quantpsy.org. Accessed 18 April 2012.
- Ismail MN, Chee SS, Nawawi H, Yusoff K, Lim TO, James WP. Obesity in Malaysia. Obes Rev 2002;3:203-8.
- Clinical Practice Guidelines on Management of Obesity, 2004. Ministry of Health Malaysia and Academy of Medicine of Malaysia website: www.moh.gov.my/attachments/3932. Accessed 18 April 2012.
- Rankinen T, Zuberi A, Chagnon YC, Weisnagel SJ, Argyropoulos G, Walts B, et al. The human obesity gene map: the 2005 update. Obesity (Silver Spring) 2006;14:529-644.
- Brantley PJ, Myers VH, Roy HJ. Environmental and lifestyle influences on obesity. J La State Med Soc 2005:157 Spec No 1:S19-27.
- Lee J, Jiang J, Sim K, Tay J, Subramaniam M, Chong SA. Gender differences in Singaporean Chinese patients with schizophrenia. Asian Journal of Psychiatry 2011;4:60-4.
- Hsiao CC, Ree SC, Chiang YL, Yeh SS, Chen CK. Obesity in schizophrenic outpatients receiving antipsychotics in Taiwan. Psychiatry Clin Neurosci 2004;58:403-9.
- Seeman MV. Secondary effects of antipsychotics: women are at greater risk than men. Schizophr Bull 2009;35:937-48.
- Wilsgaard T, Schirmer H, Arnesen E. Impact of body weight on blood pressure with a focus on sex differences: the Tromso Study, 1986-1995. Arch Intern Med 2000;160:2847-53.
- Low S, Chin MC, Ma S, Heng D, Deurenberg-Yap M. Rationale for redefining obesity in Asians. Ann Acad Med Singapore 2009;38:66-9.
- Jafar TH, Chaturvedi N, Pappas G. Prevalence of overweight and obesity and their association with hypertension and diabetes mellitus in an Indo-Asian population. CMAJ 2006;175:1071-7.
- Deurenberg-Yap M, Chew SK, Deurenberg P. Elevated body fat percentage and cardiovascular risks at low body mass index levels among Singaporean Chinese, Malays and Indians. Obes Rev 2002;3:209-15.
- Ainsah O, Salmi R, Osman CB. Binge eating, coping styles and obesity among patients with schizophrenia. Malaysian eJournal of Psychiatry 2007;17:14-9.
- Kitabayashi Y, Narumoto J, Kitabayashi M, Fukui K. Body mass index among Japanese inpatients with schizophrenia. Int J Psychiatry Med 2006;36:93-102.
- Rampal L, Rampal S, Khor GL, Zain AM, Ooyub SB, Rahmat RB, et al. A national study on the prevalence of obesity among 16,127 Malaysians. Asia Pac J Clin Nutr 2007;16:561-6.
- International comparison of obesity prevalence 2009. UK National Obesity Observatory website: http://www.noo.org.uk/publications. php5?rid=718. Accessed 18 April 2012.
- Wirshing DA. Schizophrenia and obesity: impact of antipsychotic medications. J Clin Psychiatry 2004;65 Suppl 18:13-26.
- Davidson S, Judd F, Jolley D, Hocking B, Thompson S, Hayland B. Cardiovascular risk factors for people with mental illness. Aust N Z J Psychiatry 2001;35:196-202.
- Adult obesity and socio economic status. UK National Obesity Observatory website: http://www.noo.org.uk. Accessed 18 April 2012.
- Sidik SM, Rampal L. The prevalence and factors associated with obesity among adult women in Selangor, Malaysia. Asia Pac Fam Med 2009;8:2.
- O’Carroll R. Cognitive impairment in schizophrenia. Advances in Psychiatric Treatment 2000;6:161-8.
- Bosello O, Zamboni M. Visceral obesity and metabolic syndrome. Obes Rev 2000;1:47-56.
- Grundy SM. Obesity, metabolic syndrome, and cardiovascular disease. J Clin Endocrinol Metab 2004;89:2596-600.
- Taylor DM, McAskill R. Atypical antipsychotics and weight gain — a systematic review. Acta Psychiatr Scand 2000;101:416-32.
- McIntyre RS, McCann SM, Kennedy SH. Antipsychotic metabolic effects: weight gain, diabetes mellitus, and lipid abnormalities. Can J Psychiatry 2001;46:273-81.
- Kroeze WK, Hufeisen SJ, Popadak BA, Renock SM, Steinberg S, Ernsberger P, et al. H1-histamine receptor affinity predicts short- term weight gain for typical and atypical antipsychotic drugs. Neuropsychopharmacology 2003;28:519-26.