East Asian Arch Psychiatry 2012;22:90-3
THEME PAPER
亚洲早期思觉失调网络发表的《亚洲早期思觉失调声明》
* Group members listed at the end of paper
Address for correspondence: Dr Gloria HY Wong, Asian Network of Early Psychosis, c/o Department of Psychiatry, The University of Hong Kong, Pokfulam, Hong Kong.
Tel: (852) 2255 3064; Fax: (852) 2255 1345; email: ghywong@hku.hk
Submitted: 5 March 2012; Accepted: 30 March 2012
Abstract
In line with the Early Psychosis Declaration issued by the World Health Organization and the International Early Psychosis Association, as well as the International Clinical Practice Guidelines for early psychosis by the latter in 2005, increasing interest in early intervention programmes is evident throughout Asia. Experience sharing and close collaboration that take into account the unique Asian context are needed to facilitate development of early psychosis services, education, and research in the region. The Asian Network of Early Psychosis has defined a set of Asian-specific principles to guide best practice in mental health care delivery for psychotic disorders in Asia. These principles are outlined in this paper.
Key words: Asia; Culture; Early intervention; Psychotic disorders
摘要
随著2005年世界卫生组织和国际早期思觉失调协会颁佈的《早期思觉失调声明》,以及後者颁 佈的《国际早期思觉失调临床方针》,思觉失调早期干预在亚洲越受关注。为了促进符合亚洲 人口的早期思觉失调服务的发展、教育和研究,各地的经验交流和紧密合作是必要的。亚洲早 期思觉失调网络(Asian Network of Early Psychosis)近期制定一套针对亚洲人口的思觉失调护 理準则,为这地区精神病人口的精神健康护理提供最佳指引。本文将概述这些準则。
关键词:亚洲、文化、早期干预、思觉失调
Introduction
Since the introduction of the concept of ‘early intervention for psychotic disorders’ in the 1990s, many early intervention programmes for psychosis have taken root in western countries. In Asia, the early intervention programmes were first introduced in Hong Kong and Singapore in 2001. Since then, several other similar programmes have been set up across Asia. Increasing interest in early intervention programmes is now evident in the region, and experience sharing and close collaboration are called for to facilitate development of early intervention for psychosis services, education, and research in Asia.
The Asian Network of Early Psychosis (ANEP) is an informal network of clinicians and researchers working in early intervention for psychosis in Asia. Addressing the specific culture and values in the Asian setting, the ANEP provides a platform to facilitate development of early intervention services in Asia through close exchanges and experience sharing across member sites. The ANEP also aims to promote research in the course, outcomes, and early intervention service delivery of first-episode psychosis in Asia, and encourage use of standardised instruments and assessment procedures for more comparable results. To date, the ANEP has contributors from cities in China, India,Indonesia, Japan, Korea, Malaysia, Singapore, and Taiwan. Through regional meetings and symposia, collaborative research, links with other regional and international networks, as well as an online discussion forum (https://sites.google.com/site/asianearlypsychosis), the ANEP encourages groups and researchers in the region to work together for the better care of psychosis in Asia.
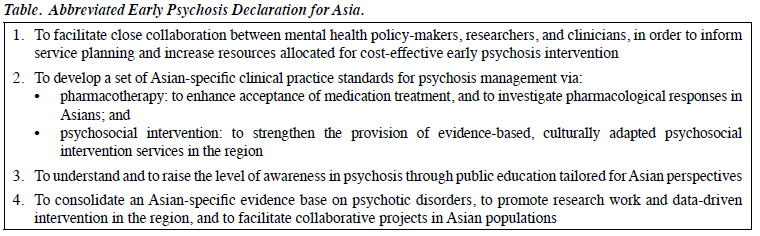
In line with the Early Psychosis Declaration issued by the World Health Organization1 and the International Early Psychosis Association, as well as the International Clinical Practice Guidelines for early psychosis by the latter institution,2 and taking into consideration the unique Asian context, we have defined a set of common principles with input from regional consultants of the ANEP to guide best practice in mental health care delivery in the field of psychotic disorders in the region. The principles outlined below were first discussed at the International Conference on Early Psychosis in Asia Pacific 2012, held in Hong Kong in January 2012. A concise summary of the statements is given in the Table.
Mental Health Policies on Psychotic Disorders
In general, Asian countries are faced with a lack of resources in early intervention for severe mental health conditions including psychotic disorders, compared with our western counterparts. Among Asian cities where early intervention programmes have commenced, high caseloads and suboptimal management remain a problem within public mental health systems. Regional and international clinical studies3-8 have provided evidence for the cost-effectiveness of comprehensive early intervention for patients with first- episode psychosis, especially during the critical period immediately following illness onset. The extra manpower and other resource input for early intervention can be offset by reduced service utilisation in terms of hospital stay and emergency services. Close collaboration between mental health policy-makers, researchers, and clinicians is needed for more informed planning in cost-effective resource allocation and achieving the best patient outcomes and mental health care at the societal level.
Clinical Care
A set of practical clinical standards for psychosis management, including pharmacotherapy and psychosocial intervention, should be developed, taking into account Asian-specific factors in terms of physiology, psychology, cultural values, and resource limitations. In particular, we sought to:
- explore and pioneer optimal interventional approaches in the context of low mental health resources and high caseload (e.g. utilisation of the primary health service in developing clinical standards, education, and training materials);
- explore and enhance Oriental cultural, societal, and famil- ial strengths for better care of early psychosis patients;
- encourage community care instead of institutional care for early psychosis;
- understand service delivery barriers to early psychosis detection and management;
- advocate adequate consultation time for early psychosis patients; and
- develop training systems for specialised professionals working in early psychosis.
Pharmacotherapy
Antipsychotics are the mainstay of treatment for psychotic disorders. In Asia, the patients and their family’s acceptance of medication treatment remains low and should be enhanced, and clinical experience should be accumulated on the use of antipsychotics in Asian populations. There are needs to: (1) reinforce correct perception of pharmacotherapy and attitudes to medication in early psychosis patients and their families; and (2) explore how treatment response and side- effects of medication are different among Asians in terms of ethnopsychopharmacogenetics.
Psychosocial Intervention
Non-medication interventions have crucial impacts on the outcomes of patients with psychotic disorders. Provision of psychosocial intervention services should be greatly strengthened in the region. We need to:
- provide evidence-based, culturally adapted psychosocial interventions to achieve the best possible clinical outcomes during the early critical period of the illness — these may include cognitive behavioural therapy (CBT), family therapy, and multidisciplinary team approaches;
- provide active and intensive psychosocial interventions by increasing consultation time, and using case management with community service programmes;
- develop and share clinical experience in modified CBT based on Oriental thinking, such as an emphasis on awareness and perception compared with a rational approach;
- develop and share experience in the implementation of community service programmes appropriate to various Asian contexts;
- capitalise on the unique Asian value of strong familial ties by promoting family support in psychosis management, including psycho-education for family members about early detection of warning signs, and psychological support for carers; and
- mobilise community leaders (e.g. religious, local, or extended families leaders), an important group with great influence that can be found in most Asian cultures, as partners in psychosocial intervention.
Education and Public Awareness
The level of awareness and understanding of psychosis remains relatively low in Asia, which contributes to long delays in help seeking, barriers to treatment compliance, and extra psychological burdens to patients and their families. Efforts are required to:
- develop and share educational materials such as brochures, posters, videos, and handouts, with a focus on psychosis rather than schizophrenia, and present them to the public in an easy and acceptable fashion for Asian or Oriental perspectives;
- promote early detection of psychosis to minimise hospitalisation and chronic disability; and
- understand and address public awareness and stigma associated with psychosis in Asian populations.
Research
An Asian-specific evidence base needs to be consolidated to better inform policy-making, clinical management, and education strategies. Concerted research efforts among Asian countries and sites are needed. We aim to: (1) promote research work and data-driven intervention as an integral component of early psychosis management; and (2) pursue collaborative projects in areas of high research priority, including:
- risk population studies in Asia;
- duration of untreated psychosis and help-seeking behaviour in Asian societies;
- early intervention during the critical period (e.g. optimal duration and outcomes of the intervention service);
- efficacy of community service programmes;
- intervention for cognitive functioning;
- biomarkers of disease vulnerability and psychosis phenotypes in Asians;
- antipsychotic treatment response in Asian populations; and
- the role of sociocultural factors in the treatment of and recovery from early psychosis in Asia.
Our Visions
With this Declaration, we aim to achieve:
- enhanced communication among mental health stakeholders and policy-makers to allocate reasonable resources for cost-effective management in the early intervention of psychosis in Asia;
- development of clinical practice standards in psychosis in Asia, with an emphasis on optimal early intervention and community care;
- promotion of pharmacological and psychosocial management of psychosis tailored to the Asian situation;
- heightened public awareness and understanding of psychosis at a regional level; and
- consolidation of high-quality and compatible scientific data on psychotic disorders specific to Asian populations.
Conclusions
As a global direction for mental health care, developing early intervention for psychosis will continue to be a primary focus of efforts in Asian countries. Work in this area must concentrate on the 3 fronts of clinical care, education, and research. With increasing recognition of the effectiveness of early psychosis management, it is anticipated that governments and relevant authorities might contribute sufficient resources to realise the directives as outlined above. Bearing in mind the heterogeneity in many aspects, including culture, ethnicity, religion, social values, and economic development among Asian countries, joint efforts focusing on the common sets of needs, challenges, and opportunities across the region will hopefully facilitate progress in early psychosis intervention in Asia. Together, the Asia region will move towards a more preventive and cost-effective model for the management of psychotic disorders, easing the burden of the illness on patients, families, and society.
The following ANEP members (in alphabetical order) contributed to the drafting and endorsement of the Declaration in March 2012:
Suk Kyoon An (Seoul, Korea)
Sherry Kit-Wah Chan (Hong Kong, China)
Wing-Chung Chang (Hong Kong, China)
Eric Yu-Hai Chen (Hong Kong, China)
Siow-Ann Chong (Singapore)
Young-Chul Chung (Jeonju, Korea)
Christy Lai-Ming Hui (Hong Kong, China)
Hai-Gwo Hwu (Taipei, Taiwan)
I Irmansyah (Jakarta, Indonesia)
Nakao Iwata (Nagoya, Japan)
Joon-Hwan Jang (Seoul, Korea)
Jun-Soo Kwon (Seoul, Korea)
Jimmy Chee-Keong Lee (Singapore)
Edwin Ho-Ming Lee (Hong Kong, China)
Helen May-Eng Lee (Singapore)
Tao Li (Chengdu, China)
Zhening Liu (Changsha, China)
Xiaohong Ma (Chengdu, China)
Ramamurti Mangala (Chennai, India)
Carla Marchira (Yogyakarta, Indonesia)
Kazunori Matsumoto (Sendai, Japan)
Masafumi Mizuno (Tokyo, Japan)
Shinji Shimodera (Kochi, Japan)
MA Subandi (Yogyakarta, Indonesia)
Michio Suzuki (Toyama, Japan)
Sarah Ann Tay (Singapore)
Rangasamy Thara (Chennai, India)
Swapna Kamal Verma (Singapore)
Gloria Hoi-Yan Wong (Hong Kong, China)
References
- Bertolote J, McGorry P. Early intervention and recovery for young people with early psychosis: Consensus statement. Br J Psychiatry 2005;187:S116-9.
- International clinical practice guidelines for early psychosis. Br J Psychiatry Suppl 2005;48:S120-4.
- McCrone P, Craig TK, Power P, Garety PA. Cost-effectiveness of an early intervention service for people with psychosis. Br J Psychiatry 2010;196:377-82.
- Wong KK, Chan SK, Lam MM, Hui CL, Hung SF, Tay M, et al. Cost- effectiveness of an early assessment service for young people with early psychosis in Hong Kong. Aust N Z J Psychiatry 2011;45:673- 80.
- Mihalopoulos C, McGorry PD, Carter RC. Is phase-specific, community-oriented treatment of early psychosis an economically viable method of improving outcome? Acta Psychiatr Scand 1999;100:47-55.
- Cullberg J, Mattsson M, Levander S, Holmqvist R, Tomsmark L, Elingfors C, et al. Treatment costs and clinical outcome for first episode schizophrenia patients: a 3-year follow-up of the Swedish “Parachute Project” and two comparison groups. Acta Psychiatr Scand 2006;114:274-81.
- Dodgson G, Crebbin K, Pickering C, Mitford E, Brabban A, Paxton R. Early intervention in psychosis service and psychiatric admissions. Psychiatr Bull 2008;32:413-6.
- Goldberg K, Norman R, Hoch JS, Schmitz N, Windell D, Brown N, et al. Impact of a specialized early intervention service for psychotic disorders on patient characteristics, service use, and hospital costs in a defined catchment area. Can J Psychiatry 2006;51:895-903.