Hong Kong J Psychiatry 2005;15(1):9-13
ORIGINAL ARTICLE
TSF Chan, LCW Lam, HFK Chiu
Dr Teresa Sau-Fan Chan, FHKCPsych, FHKAM (Psychiatry),
Department of Psychiatry, Tai Po Hospital, Tai Po, Hong Kong, China.
Dr Linda Chiu-Wa Lam, FHKCPsych, FHKAM (Psychiatry), Department of Psychiatry, The Chinese University of Hong Kong, Shatin, Hong Kong, China.
Dr Helen Fung-Kum Chiu, FRCPsych, FHKCPsych, FHKAM
(Psychiatry), Department of Psychiatry, The Chinese University of Hong Kong, Shatin, Hong Kong, China.
Address for correspondence: Dr Teresa Sau-Fan Chan, Department of Psychiatry, Tai Po Hospital, Tai Po, Hong Kong, China.
Tel: (852) 2607 6111; Fax: (852) 2662 3568;
E-mail: chansft@ha.org.hk
Submitted: 7 April 2004; Accepted: 6 May 2005
Abstract
Objective: To validate the Chinese version of the Zarit Burden Interview as an instrument for assessing the stress experienced by carers of elderly patients with dementia.
Patients and Methods: The Zarit Burden Interview was first translated into Chinese and then back-translated into English for comparison. Forty Chinese patients with mild to moderate de- mentia were recruited from 2 psychiatric clinics in Hong Kong. The Zarit Burden Interview, General Health Questionnaire, and Caregiver Activity Survey were completed by the patients' carers. Two raters rated another 16 carers separately for assessment of inter-rater reliability.
Results: The intraclass correlation coefficient was 0.99 and the split half correlation coefficient was 0.81, suggesting a high inter-rater reliability and internal consistency. The correlation be- tween the Zarit Burden Interview and the General Health Questionnaire was 0.59 (p < 0.001), and the correlation between the Zarit Burden Interview and the Caregiver Activity Survey was 0.57 (p < 0.001), suggesting high conceptual validity.
Conclusion: The Chinese version of the Zarit Burden Interview is a valid and reliable tool to evaluate the stress experienced by carers of elderly people with dementia in Hong Kong.
Key words: Dementia, Dependency, Stress, psychological
Introduction
Identification of carer stress is as an important issue in car- ing for patients with dementia. It is becoming increasingly evident that carers have a role in the overall treatment outcome. Most elderly people with dementia live in the community and rely heavily on their relatives for support. Early institutionalisation is undesirable, as this generally imposes a negative effect on disease progression. Patients with dementia show greater impairment in unfamiliar settings, while familiar cues at home can often trigger well- established habits. However, the burden of taking care of an elderly relative with dementia at home can be great. Apart from the demands of physical care, patients with dementia often have psychiatric and behavioural problems that are difficult to deal with in the absence of adequate support.
Having limited knowledge and skills, carers often experi- ence stress when caring for relatives with dementia.
The burden of care is affected by different factors. The illness severity and level of disability could affect the bur- den for patients and their carers.1-3 Behavioural problems and dependency of patients contribute to, and may be a major cause of, stress.4-9 However, the strengths and coping mecha- nisms of carers, as well as social support and community resources, could affect the perceived burden.3,10-12 The amount of time carers spend with their relative each day also affects the perceived burden.9,13 Poor physical and psychiatric health of carers can also affect the perceived level of stress.3,8,14,15
Excessive stress could lead to increased psychiatric morbidity for carers.16,17 Gilleard et al found that the preva- lence of psychological disturbance was high among carers, as shown by an increased score for the General Health Ques- tionnaire (GHQ).18 Excessive stress for the carer could also lead to an increased chance of institutionalisation for the patient.19,20 There is also evidence to show that carers' stress and maladaptive coping strategies may result in increased behavioural problems of patients with dementia.21 These factors would lead to an increase in economic burden.22,23
To better address the stress of carers of patients with dementia, it is desirable to have an instrument to measure their burden in direct relationship to the demand for care. This approach will help clinicians to investigate the factors affecting the level of stress and design appropriate intervention strategies. The Zarit Burden Interview (ZBI) has been specifically designed for the assessment of subjective burden of carers, defined as the extent to which carers perceived their emotional or physical health, social life, and financial status to have changed as a result of caring for their relative with dementia.24 The selection of items in this interview was based on clinical experience with carers and prior studies. The ZBI has been used by carers of patients with dementia in different countries with satis- factory reliability and validity.25 The aim of this study was to evaluate the psychometric properties of the Chinese version of the ZBI for measuring the perceived burden of stress in Chinese carers of elderly people with dementia in Hong Kong.
Patients and Methods
Patients with dementia were recruited from 2 psychiatric clinics in Shatin and Tai Po in Hong Kong from December 1999 to August 2000. All patients fulfilled the Diagnostic and Statistical Manual of Mental Disorders-IV diagnostic criteria of dementia; severity was mild to moderate ac- cording to the Clinical Dementia Rating (CDR) of 1 or 2. Patients were required to have at least 1 primary carer for inclusion into the study. Most of the participants were living with their carers in the community. Informed consent was obtained from the patients with dementia and their carers, and the study was approved by the Clinical Research Ethics Committee of The Chinese University of Hong Kong.
Assessment Tools
The ZBI comprises 22 items. Carers were requested to indi- cate the level of distress caused by each item, ranging from 'not at all' to 'extremely' distressing, on a scale of 0 to 4. A total burden score was obtained by adding the responses to the individual items. The possible score ranged from 0 to 88; a higher score indicated greater carer distress. The ZBI includes factors most frequently mentioned by carers as problem areas such as carer's health, psychological well being, finances, social life, and the relationships between the carer and the patient with dementia.
The GHQ has been well validated as a screening instru- ment for psychiatric morbidity in the community, and is used in different languages and cultures. There are 4 different versions available containing 60, 30, 28, or 12 items. Studies have shown that the shorter versions are as good as the longer versions for case detection.26 The 12-item version was used in this study because it is short and easy to administer.
The Caregiver Activity Survey (CAS) is an instrument to measure the amount of time a carer spends looking after a dependent patient in the 24 hours prior to the assessment. The CAS consists of 6 areas of daily living: communicating with the patient, using transportation, eating, dressing, look- ing after the patient's appearance, and supervising the patient. The total time could be more than 24 hours because of overlap of time used for the different areas.27
The Community Screening Instrument for Dementia (CSI-D) is a well-validated education and culture-screening instrument for dementia.28 The CSI-D consists of 2 parts: cognitive assessment of patients with dementia in 6 domains and a carer's report of the patient's daily functioning and general health. The cognitive function score (CFS) is an item-weighted total score of the cognitive test, with higher scores meaning better cognitive function. The discriminant function score (DFS) is a weighted score combining the cognitive and informant score according to an algorithm that discriminates between patients with and without dementia. A higher score indicates greater cognitive decline.
The CDR is a widely used instrument for staging the severity of dementia. The CDR is obtained via clinical interview with patients and a reliable carer. Impairment in each of 6 cognitive functions (memory, orientation, judgement and problem solving, community affairs, home and hobbies, and personal care) is rated by a trained pro- fessional interviewer on a 5-point scale.29 CDR 0 indicates no dementia and CDR 0.5, 1, 2, and 3 indicate questionable, mild, moderate, and severe dementia, respectively.30 The global CDR was derived from an algorithm based on the information obtained in the clinical interview and its reliability for measuring and staging dementia has been demonstrated.31
Methods
The ZBI was first translated into Chinese by a bilingual psychiatrist, and then back-translated to English by an independent bilingual university graduate. The Chinese version was modified until the back-translated version was comparable to the original English version. The translated instrument was then assessed for acceptability and concep- tual validity. Focus group discussions were held with health care professionals, community leaders, and carers of patients with dementia. The content and wording were considered clear, with no major modifications required. After obtain- ing consent, the carers completed the ZBI, GHQ, CAS, and the informant part of CSI-D, while the patients received the CSI-D cognitive test. All of the scales were interviewer- applied instruments and were rated by trained research assistants. Other demographic data were obtained from the carers. Two raters rated a further 16 carers separately for assessment of inter-rater reliability of the ZBI.
Statistical Analysis
The Statistical Package for the Social Sciences version 9.0 and non-parametric methods were used for data analysis. Multi-group comparisons for mean ZBI scores were done using the Kruskal-Wallis H test. Inter-rater reliability was measured by intraclass correlation coefficient, while inter- nal consistency was measured by split half correlation coefficient. Correlations between the ZBI and GHQ, and ZBI and CAS were assessed for conceptual validity. Corre- lations of ZBI with CFS and DFS were also calculated to evaluate the possible correlation of carer burden with the severity of cognitive impairment.
Results
Forty patients with dementia and their carers were recruited for the study. Twenty one carers (52.5%) were women and 19 (47.5%) were men; the mean age was 51 years. Thirty patients with dementia (75%) were women and 10 (25%) were men; the mean age was 74.9 years. The total mean ZBI score was 24.6. The mean ZBI scores in the carer sub- groups are shown in Table 1. The inter-group differences were not significant.
The intraclass correlation coefficient was 0.99. The split half correlation coefficient was 0.81. There was a significant correlation between the ZBI and GHQ (0.59; p < 0.001) and between the ZBI and CAS (0.57; p < 0.001). Furthermore, there was a significant negative correlation between ZBI, DFS, and CFS, suggesting that a lower level of cognitive ability was associated with greater carer burden (Table 2).
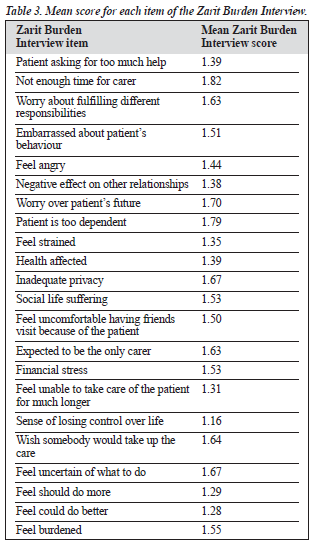
The mean scores for the individual items in the ZBI ranged from 1.16 to 1.82 (Table 3). The highest score was for not enough time for the carer, followed by feeling that the patient was too dependent on the carer. Worry over the patient's future, inadequate privacy, feeling uncertain about what to do, wishing someone else would care for the patient, and finding it difficult to fulfil different responsibilities were also highly scored items.
Discussion
The intraclass correlation coefficient was 0.99 and the split half correlation coefficient was 0.81, suggesting that the Chinese version of the ZBI has a satisfactory inter-rater re- liability and internal consistency. Assuming that increased subjective burden would lead to increased psychiatric and psychological disturbance, which has been shown in previous studies,16,17 the highly significant correlation between ZBI and GHQ supported the conceptual validity of the ZBI. A greater carer burden was expected with increas- ing time spent on the care of patients with dementia.6,13,32 Therefore, the high correlation between the CAS and ZBI also suggested that the ZBI was conceptually valid.
The total mean score of the ZBI in this group of carers was 24.6, which was lower than the mean score of 31.0 in the study by Zarit et al.24 This could reflect a general lower level of perceived stress due to caring for patients with dementia among this group. In the Chinese population, as- suming responsibility for the care of elderly relatives is usual — children are expected to care for their parents, and wives are expected to care for their husbands. This concept may reduce the stress experienced by a carer because this role is accepted.33,34 However, there is a possibility of under- reporting of stress by the carers. In a culture with a strong emphasis on filial obligation, carers may be reluctant to admit to stressful feelings and discussion of such problems outside the family might be regarded as inappropriate. A study performed in Malaysia showed that Chinese people have a greater carer burden than Malays and Indians.13 The authors suggested that, while filial obligation coupled with the societal norm of caring for elderly family members was still intact across all cultures in the Malaysian population, cultural differences might influence how filial obligation and burden were related in the care-giving process. The authors further suggested that filial obligation might be the primary motive for care-giving, explaining the greater burden experienced.
The comparison of level of carer burden in different populations cannot be made simply by looking at the ZBI scores without considering the characteristics of the carers such as age, sex, educational level, ethnicity, and cultural values, which could significantly affect carer burden. Therefore, the calculation of a cut-off score for the ZBI to identify carers at high risk for stress may not be useful because different populations with different characteristics may need different cut-off scores.
Studies have shown differences in carer burden among different age groups and sexes, and according to the relation- ship with the patient.10,14,35 This study failed to show such dif- ferences. However, this could be due to the small sample size.
The extent of cognitive decline of patients with demen- tia reflected the severity of the illness, and this aspect af- fected the subjective burden of the carer.1,2 The patients in this study had mild to moderate dementia, and the results suggested that the severity of cognitive impairment may be associated with increased stress experienced by the carers. However, as the severity of the dementia progressed and be- havioural problems attenuated, some carers found the patients with severe dementia easier to care for; while the physical demands increased, the psychological demands decreased. Physical demands caused a different type of stress from that caused by the psychological demands. Mobile and active pa- tients with dementia are more able to act out their thoughts and feelings, making them more difficult to manage.36
The carers in this study had high scores for areas such as fear of what the future held for the patient, which is com- patible with other studies.15,24 In this study, the patients with dementia were at a relatively early stage in the course of their illness. Therefore, uncertainty about the progression of the disease was understandable. Other high scores were noted for areas such as feeling that the patient was too dependent on the carers and not having enough time for themselves. Lack of time for oneself leaves little time for rejuvenation and increases stress.6,9,15 Life balance is important in western cultures and may also be important in a Chinese population.
Stress caused by caring for patients and meeting other responsibilities is common. Approximately one-third of the carers in this study were in full-time employment, and many of them also had different family roles. Therefore, they fre- quently felt guilty about not fulfilling a role and felt trapped. The desire to leave the care of the patients to another person had a high score. The score suggests that carers were not ready for the role, but felt obliged to take the responsibility. Alternatively, this score may reflect the psychological state of 'burn out' among carers. Generally, the highly scored items in the ZBI were similar those in the study by Zarit et al.24 This finding suggests that the difficulties experienced by carers may be similar in different cultures.
The number of carers enrolled in this study was relatively small, which limited its ability to study factors associated with greater carer burden in addition to the main focus of validation of the Chinese version of ZBI. This may be why age, sex, educational level, and kinship of the carers with the patients were not found to significantly affect the carer burden. Other important factors such as personal coping, physical and psychological well-being, available social support, and prior quality of the relationship of the carers with the patients37,38 were also not addressed in this study.
This study investigated the association of cognitive func- tion and the level of carer burden. However, self-care impairment, behavioural and psychotic symptoms, and level of dependency and functional deterioration may be equally, if not more, important for modulating the carer burden. These issues were not explored in this study. Patients with mild to moderate dementia were selected for this study because more severely affected patients often live in institutions and it is more difficult to identify the primary carers. The extent and sources of stress for carers of patients with severe dementia may be different from those of carers of patients with mild or moderate dementia. Therefore, larger studies involving more carers and patients with a wide range of disease sever- ity that address different carer and patient factors may help to provide a more complete picture of the burden of carers of patients with dementia in a Chinese population. Future studies could also focus on the effect of stress on some specific areas of outcome of the patients such as the develop- ment and progression of behavioural and mood symptoms.
Carers with high scores in the GHQ and ZBI could be fol- lowed up for development of psychiatric illness or change of subjective burden over time as their relative's illness progresses.
This study served the purpose of testing the reliability and validity of the Chinese version of the ZBI for use in future studies, which could lead to a better understanding of carer burden of dementia in Hong Kong. The ZBI is a reliable and valid instrument to assess the subjective bur- den of carers of patients with dementia in the Chinese population. The subjective burden of carers is high and greater efforts to address this burden will enhance the treat- ment of patients with dementia. Memory and behavioural impairment are not easily ameliorated, and interventions that focus principally on the control of specific memory or behavioural deficits have a low probability of success. Instead, an approach that includes support for carers to im- prove their coping mechanisms and provide respite, as well as modifying aspects of the behaviour of patients with dementia will bring better outcomes.
References
- Almberg B, Grafstrom M, Winblad B. Caring for a demented elderly person—burden and burnout among caregiving relatives. J Adv Nurs 1997;25:109-116.
- Haley WE, Levine EG, Brown SL, Berry JW, Hughes GH. Psychological, social, and health consequences of caring for a relative with senile dementia. J Am Geriatr Soc 1987;35:405-411.
- Baumgarten M, Battista RN, Infante-Rivard C, Hanley JA, Becker R, Gauthier S. The psychological and physical health of family members car- ing for an elderly person with dementia. J Clin Epidemiol 1992;45:61-70.
- Gilleard CJ, Belford H, Gileard E, Whittick JE, Gledhill K. Emotional distress amongst the supporters of the elderly mentally infirm. Br J Psychiatry 1984;145:172-177.
- Winslow BW, Carter P. Patterns of burden in wives who care for hus- bands with dementia. Nurs Clin North Am 1999;34:275-287.
- Kim JM, Shin IS, Jeong SJ, Gormley N, Yoon JS. Predictors of institutionalization in patients with dementia in Korea. Int J Geriatr Psychiatry 2002;17:101-106.
- De Vugt ME, Stevens F, Aalten P, et al. Do caregiver management strategies influence patient behaviour in dementia? Int J Geriatr Psychiatry 2004;19:85-92.
- Moore MJ, Zhu CW, Clipp EC. Informal costs of dementia care: esti- mates from the National Longitudinal Caregiver Study. J Gerontol B Psychol Sci Soc Sci 2001;56:S219-228.
- Langa KM, Chernew ME, Kabeto MU, et al. National estimates of the quantity and cost of informal caregiving for the elderly with dementia. J Gen Intern Med 2001;16:770-778.
- Meiland FJ, Danse JA, Wendte JF, Klazinga NS, Gunning-Schepers LJ.
- Caring for relatives with dementia — caregiver experiences of relatives of patients on the waiting list for admission to a psychogeriatric nursing home in the Netherlands. Scand J Public Health 2001;29:113-121.
- Matsuda O. The effect of coping on the caregiver of elderly patients with dementia. Psychiatry Clin Neurosci 1995;49:209-211.
- Leinonen E, Korpisammal L, Pulkkinen LM, Pukuri T. The compari- son of burden between caregiving spouses of depressive and demented patients. Int J Geriatr Psychiatry 2001;16:387-393.
- Nagatomo I, Akasaki Y, Uchida M, Tominaga M, Hashiguchi W, Takigawa M. Gender of demented patients and specific family rela- tionship of caregiver to patients influence mental fatigue and burdens on relatives as caregivers. Int J Geriatr Psychiatry 1999;14:618-625.
- Clyburn LD, Stones MJ, Hadjistavropoulos T, Tuokko H. Predicting caregiver burden and depression in Alzheimer's disease. J Gerontol B Psychol Sci Soc Sci 2000;55:S2-13.
- Chappell NL, Reid RC. Burden and well-being among caregivers: ex- amining the distinction. Gerontologist 2002;42:772-780.
- Coen RF, Swanwick GR, O'Boyle CA, Coakley D. Behaviour distur- bance and other predictors of carer burden in Alzheimer's disease. Int J Geriatr Psychiatry 1997;12:331-336.
- Hebert R, Dubois MF, Wolfson C, Chambers L, Cohen C. Factors as- sociated with long-term institutionalization of older people with dementia: data from the Canadian Study of Health and Aging. J Gerontol A Biol Sci Med Sci 2001;56:M693-699.
- Cox C, Monk A. Hispanic culture and family care of Alzheimer's patients. Health Soc Work 1993;18:92-100.
- Reis MF, Gold DP, Andres D, Markiewicz D, Gauthier S. Personality traits as determinants of burden and health complaints in caregiving. Int J Aging Hum Dev 1994;39:257-271.
- Wijeratne C. Review: pathways to morbidity in carers of dementia sufferers. Int Psychogeriatr 1997;9:69-79.
- Choo WY, Low WY, Karina R, Poip PJ, Ebenezer E, Prince MJ. So- cial support and burden among caregivers of patients with dementia in Malaysia. Asia Pac J Public Health 2003;15:23-29.
- Annerstedt L, Elmstahl S, Ingvad B, Samuelsson SM. Family caregiving in dementia — an analysis of the caregiver's burden and the "breaking- point" when home care becomes inadequate. Scand J Public Health 2000;28:23-31.
- Gallicchio L, Siddiqi N, Langenberg P, Baumgarten M. Gender differ- ences in burden and depression among informal caregivers of demented elders in the community. Int J Geriatr Psychiatry 2002;17:154-163.
- Zarit SH, Reever KE, Bach-Peterson J. Relatives of the impaired elderly: correlates of feelings of burden. Gerontologist 1980;20:649-655.
- Arai Y, Kudo K, Hosokawat, Washio M, Miura H, Hisamichi S. Reli- ability and validity of the Japanese version of the Zarit Caregiver Bur- den Interview. Psychiatry Clin Neurosci 1997;51:281-287.
- Goldberg DP, Gater R, Sartorius N, et al. The validity of two versions of the GHQ in the WHO study of mental illness in general health care. Psychol Med 1997;27:191-197.
- Davis KL, Marin DB, Kane R, et al. The Caregiver Activity Survey (CAS): development and validation of a new measure for caregivers of persons with Alzheimer's disease. Int J Geriatr Psychiatry 1997;12: 978-988.
- Chan TSF, Lam LCM, Chiu HFK, Prince M. Validity and applicability of the Chinese version of Community Screening Instrument for Dementia. Dement Geriatr Cogn Disord 2003;15:10-18.
- Hughes PH, Berg L, Danzuger WL, Coben LA, Martin RC. A new clini- cal scale for the staging of dementia. Br J Psychiatry 1982;140:566-572. 30. Morris JC. The Clinical Dementia Rating (CDR): current version and scoring rules. Neurology 1993;41:2412-2414.
- Burke WJ, Miller JP, Rubin EH, Morris JC, Coben LA, Duchek J. Reliablility of the Washington University Clinical Dementia Rating. Arch Neurol 1988;45:31-32.
- Tornatore JB, Grant LA. Burden among family caregivers of persons with Alzheimer's disease in nursing homes. Gerontologist 2002;42: 497-506.
- Youn G, Knight BG, Jeong HS, Benton D. Differences in familism values and caregiving outcomes among Korean, Korean American, and White American dementia caregivers. Psychol Aging 1999;14:355-364.
- Pang FC, Chow TW, Cummings JL, et al. Effect of neuropsychiatric symptoms of Alzheimer's disease on Chinese and American caregivers. Int J Geriatr Psychiatry 2002;17:29-34.
- Chumbler NR, Grimm JW, Cody M, Beck C. Gender, kinship and caregiver burden: the case of community-dwelling memory impaired seniors. Int J Geriatr Psychiatry 2003;18:722-732.
- Miyamoto Y, Ito H, Otsuka T, Kurita H. Caregiver burden in mobile and non-mobile demented patients: a comparative study. Int J Geriatr Psychiatry 2002;17:765-773.
- Gold DP, Cohen C, Shulman K, Zucchero C, Andres D, Etezadi J. Caregiving and dementia: predicting negative and positive outcomes for caregivers. Int J Aging Hum Dev 1995;41:183-201.
- Zarit SH, Todd PA, Zarit JM. Subjective burden of husbands and wives as caregivers: a longitudinal study. Gerontologist 1986;26:260-266.



_Table2.PNG)
