Hong Kong J Psychiatry 2006;16:128-31
Original Article
Cross-cultural Validity of the Eating Disorder Examination: a Study of Chinese Outpatients with Eating Disorders in Hong Kong
進食失調症會談問卷的跨文化有效度 : 一項在中國香港進食失調症門診進行的調查
LLS Lau, S Lee, W Wong
劉麗珊、李誠、李浩銘、黃宗顯
Dr Lisa LS Lau, MBChB, DipMed, FHKCPsych, FHKAM (Psychiatry), Medical and Health Officer, Department of Psychiatry, The Chinese University of Hong Kong, Hong Kong, China.
Prof S Lee, MBBS, MD, MRCPsych, FHKCPsych, FHKAM (Psychiatry), Department of Psychiatry, The Chinese University of Hong Kong, Hong Kong, China.
Dr Edwin Lee, MBChB, MRCPsych, Resident, Department of Psychiatry, Tai Po Hospital, Hong Kong, China.
Dr Willy Wong, MBChB, Resident, Department of Psychiatry, Tai Po Hospital, Hong Kong, China.
Address for correspondence: Dr Lisa LS Lau, Department of Psychiatry, The
Chinese University of Hong Kong, Hong Kong, China. Tel: (852) 2607 6111; Fax (852) 2662 3568;
E-mail: lisalaishan@hotmail.com
Submitted: 18 December 2006; Accepted: 29 January 2007
Abstract
Objective: To assess the cross-cultural validity of the Cantonese-Chinese version of the Eating Disorder Examination among Chinese outpatients.
Patients and Methods:The Cantonese-Chinese version of the Eating Disorder Examination was administered to 42 patients with anorexia nervosa, anorexia nervosa without fat phobia, bulimia nervosa or binge eating disorders and to 12 controls. An eating disorders specialist made the clinical diagnoses. The eating disorder psychopathologies of cases were compared with controls.
Results: The Cantonese-Chinese version of the Eating Disorder Examination exhibited satisfactory internal consistency, sensitivity, specificity, positive and negative predictive value for diagnosing subjects with anorexia nervosa, bulimia nervosa and binge eating disorders. All subscales discriminated between patients with anorexia nervosa or bulimia nervosa and controls. Apart from the restraint subscale, the other three subscales discriminated between those with binge eating disorders and controls. Those with anorexia nervosa and anorexia nervosa without fat phobia had similar results except for those of the weight concern subscale. No subjects with eating disorders met the definition for excessive exercise.
Conclusion:The Cantonese-Chinese version of the Eating Disorder Examination has good reliability, discrimination and criterion validity. The similarities between responses from those with anorexia nervosa and those with anorexia nervosa without fat phobia made the inclusion of fat phobia as a diagnostic criterion for anorexia nervosa in the 4th Edition of the Diagnostic and Statistical Manual of Mental Disorders questionable. The discrepancy between hinge eating disorders and control regarding weight and shape concern suggests cognitive features should be considered as diagnostic criteria for binge eating disorders. The definition of excessive exercise may not be appropriate for Hong Kong Chinese population.
Key words: Anorexia nervosa; Eating disorder; Psychometrics
摘要
目的:評估進食失調症會談問卷(CC-EDEI)粵語版的跨文化有效度。
患者與方法:以粵語版CC-EDEI比較42位進食失調(厭食症、非恐胖厭食症、暴食症或過胖暴食症)病人及12位對照者。病症由有關專家診斷,並以進食失調精神病理學比較兩組結果。
結果:粵語版CC-EDEI顯示厭食症、暴食症和過胖暴食症患者的內部統一性、敏感度、特異性和正負預測值均令人滿意。所有分量得分都可明顯區分對照組與厭食症組,以及對照組和暴食症組。除克制分量得分,其他三種分量得分都可明顯區分過胖暴食症患者和對照者。除了重量關心分量得分,厭食症患者和非恐胖厭食症患者在其他分量得分皆相若。沒有病者因過量運動被診斷為患有進食失調症。
結論:粵語版CC-EDEI具良好的可靠性、區別性和標準有效性。厭食症組和非恐胖厭食症組的數據相似,令人懷疑應否將「恐胖」列入《精神疾病診斷和統計手冊》第四版內的厭食症診斷標準;而過胖暴食症患者和對照患者在關心身形及體重分數的差別,也說明了認知態度應考慮被列入過胖暴食症的診斷標準。以過量運動界定進食失調症則不適用於華籍人口。
關鍵詞:厭食症、暴食症、進食失調、心理測量學
Introduction
Several community studies in Hong Kong have indicated that between 3 and 10% of young females suffer from eating disorders. At a university-affiliated psychiatric clinic in Hong Kong, the number of referrals of patients with eating disorders (primarily anorexia nervosa [AN]) has increased from 2 per year in the early 1990s to at least 1 per week by mid-2000.1 Lee and Katzman1 noted improvements in the quality of eating disorder research, including greater reporting of reliability and validity information over the past 2 decades. Nonetheless, compared with anxiety disorders, eating disorder studies are less likely to use structured diagnostic assessments (10% vs 21%).2 Therefore, one of the most important challenges in the study of eating disorders is ensuring the use of high-quality assessment tools. Within Chinese societies in particular, the lack of a valid and culturally sensitive diagnostic instrument to address the complex psychopathology of eating disorders, is a significant obstacle to research.3
Eating disorder instruments, such as the Eating Attitude Test-26 (EAT-26; Chinese version) and Eating Disorder Inventory (EDI) have received more attention in Chinese communities. Both EAT-26 and EDI are self- reporting questionnaires and they may not provide reliable data for constructs that are more abstract and difficult to define.4 Binge eating is one such challenging construct as opinions of what constitutes a large amount of food often vary from individual to individual and may differ markedly from that of the clinical interviewer.5 The extent to which self-evaluation is unduly influenced by shape and weight, included in the Diagnostic and Statistical Manual of Mental Disorders–4th Edition (DSM-IV6) criteria for both AN and bulimia nervosa (BN), is also difficult to measure because it is an abstract concept that requires an awareness of self- definition.2 Dietary restraint is considered an important concept in eating disorders but has also been difficult to assess.7 In addition, Franko et al8 and Striegel-Moore et al9 have suggested that the EDI may not generalise as well to older binge eating disorder (BED) or ethnically diverse samples.2 In contrast, the Eating Disorder Examination (EDE) permits the investigator to clarify the underlying meaning of the abstract constructs with subjects.10,11 This is particularly so for understanding the definition of binge eating, the importance of shape or weight and dietary rules.
The EDE is a semi-structured investigator-based interview used for assessing eating disorder psychopathology as reflected by 4 subscales: restraint, eating concern, shape concern, and weight concern. Most items are rated on a 7- point scale ranging from 0 to 6 used to rate either frequency or severity. In most instances, 0 represents the absence of the feature in question and 6 represents its presence to an extreme degree. Frequency ratings are based on a 28- day month.10 It can be used to arrive at a diagnosis of AN, BN or a BED.10,11 The EDE has shown good psychometric properties in both community and clinical studies in western populations, but studies of its cross-cultural validity are scanty.12-14 Our study set out to assess the cross-cultural validity of the Cantonese-Chinese interview version of the EDE (CC-EDEI) among Chinese outpatients.
Methods
This study received the Clinical Research Ethical Approval of the Chinese University of Hong Kong. The interview version of the EDE, the 12th Edition was translated to the Cantonese-Chinese version with careful consideration of cultural and linguistic equivalents by a panel of experts including an eating disorder specialist, an experienced psychiatrist, and a clinical psychologist. The Cantonese version was then translated back to English by an individual with a Bachelor’s degree in English and compared with the original EDE. The above process was repeated until a satisfactory Cantonese-Chinese version (CC-EDEI) was created.
The study sample was made up of 101 subjects who represented a consecutive series of referrals to a university-affiliated psychiatric clinic and the Hong Kong Eating Disorder Association (HEDA) from January 2005 to September 2005. The latter is a charitable organisation, running monthly parents’ support group meetings and providing outpatient counselling to people with eating disorders.
Forty two subjects fulfilled the criteria for AN (n = 9), BN (n = 17), BED (n = 7) and anorexia nervosa without fat phobia (NFAN) [n = 9] respectively. Commonly seen in Hong Kong and less-industrialised societies, these non- fat phobic patients attribute their emaciation to somatic complaints such as gastric bloating or loss of appetite,15 and fulfil culture-flexible diagnostic criteria for AN.16 The remaining 59 patients had ‘eating disorder not otherwise specified (EDNOS)’.17
Cantonese-speaking Chinese patients aged from 18 to 65 years with a diagnosis of either AN, NFAN, BN or BED were included. Those who were pregnant or had significant physical illnesses were excluded. The clinical DSM-IV diagnosis was made by either an eating disorder specialist (n = 17) or an experienced psychiatrist (n = 25). Twelve fourth-year medical students were invited to participate as controls and were assessed by the psychiatrist to make sure they did not fulfil DSM-IV eating disorder diagnoses. Two other investigators administered the CC-EDEI to patients and controls and were blinded to the status of the subjects. Before the study began, both investigators received interview training of the EDE and weekly supervision from the eating disorder specialist during the study. They regularly discussed and reviewed any ambiguous cases during supervision.
Data Analysis
Data were entered into and analysed using the Statistical Package for Social Science (SPSS) Windows version 11.0. A p value of less than 0.05 was considered statistically significant. The one-way analysis of variance (ANOVA) was used for continuous data with the Bonferroni test for post hoc comparison. The Cronbach alpha coefficients for each subscale were calculated to test internal consistency. For discriminative validity, a 2-tailed independent sample t test was used to compare continuous variables between patients with AN, NFAN, BN or BED and controls. The sensitivity, specificity, positive and negative predictive values for establishing the diagnoses of AN, BN, and BED were calculated against the clinical DSM-IV diagnosis made by the eating disorder specialist and experienced psychiatrist without reference to the EDE ratings.
Results
Demographic Data
The controls (mean age ± SD, 23.95 ± 4.66 years) and the subjects with either AN (24.00 ± 8.11 years), NFAN (24.01 ± 7.35 years), BN (23.47 ± 3.78 years), or BED (24.50 ± 8.56 years) were similar in age (p > 0.05).
Subjects with AN (16.45 ± 1.58 kg/m2) and those with NFAN (16.90 ± 2.58 kg/m2) had a similar body mass index (BMI). Those with AN showed significantly lower BMIs than those within the BN (22.14 ± 4.13 kg/m2), BED (29.39 ± 5.37 kg/m2) and control (20.19 ± 3.28 kg/m2) groups (p < 0.05). Subjects with BED had significantly higher BMIs than those within the other 4 groups (p < 0.05).
Reliability
The Cronbach alpha coefficients for each subscale were 0.81 (restraint), 0.89 (eating concern), 0.95 (shape concern), and 0.81 (weight concern). The data were compared with equivalent findings from the Oxford study (restraint: 0.75; eating concern: 0.90; shape concern: 0.79; weight concern: 0.67)12 and the Sydney study (restraint: 0.78; eating concern: 0.68; shape concern: 0.70; weight concern: 0.70).18 This study obtained better internal consistency in all 4 subscales than the other 2 studies.
Discriminative Validity
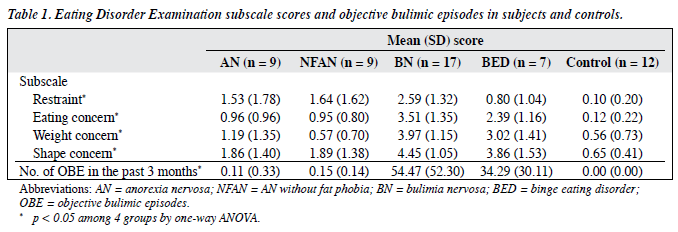
Each subscale of the CC-EDEI was found to discriminate well between those with BN and those who were controls (p < 0.05), as well as between those with AN and those who were controls (p < 0.05) [Table 1]. Apart from the weight concern subscale, the global scale and the remaining 3 subscales discriminated effectively between patients with NFAN and those who were controls (p < 0.05). In addition, with the exception of the restraint subscale, those with BED showed a significant difference from controls on the global scale and the remaining 3 subscales (p < 0.05). Both BN and BED subjects showed significantly more objective bulimic episodes (OBE) than controls (p < 0.05), but there were no significant differences in OBE between those with BN and BED (p > 0.05). There were no significant differences in OBE between those with AN and those who were controls (p > 0.05), as well as between those with NFAN and those who were controls (p > 0.05).
Criterion Validity
The CC-EDEI showed good sensitivity, specificity, positive predictive value and negative predictive value for diagnosing patients with AN, BN, and BED (Table 2).
Comparison between Anorexia Nervosa and Anorexia Nervosa without Fat Phobia
The patients with either AN or NFAN were similar in age, BMI, and OBE (p > 0.05). Apart from the weight concern subscale, there was no significant difference between patients with AN and those with NFAN on the restraint, eating and shape concern subscales (p > 0.05).
Excessive Exercise
When interpreting EDE results, the Oxford definition of excessive exercise was used. Similarly, when interpreting the results from the CC-EDEI, the Oxford definition of excessive exercise (intense exercising to control shape or weight occurring on average at least 5 days per week over the past 3 months) was adhered to.10 None of the patients with AN, NFAN, BN, BED, nor the controls met this definition.
Discussion
This study found that the CC-EDEI has satisfactory internal consistency on both the global scale and the 4 subscales. Moreover, for each eating disorder diagnosis, the global scale as well as 3 out of the 4 subscales discriminated well between subjects with eating disorders and those who were controls. The CC-EDEI also demonstrated satisfactory criterion validity in arriving at diagnoses of AN, BN, and BED. The satisfactory internal consistency and discriminative validity found in this study are compatible with those in the Sydney and Oxford studies. They support the contention that the CC-EDEI is a cross-culturally reliable and valid instrument for measuring eating psychopathology in a multidimensional manner. Nonetheless, our findings raise several problems of cross-cultural interest.
Many leading researchers have questioned the mandatory inclusion of fat phobia as a diagnostic criteria for AN.1 Researchers have suggested that not all Asian anorexic patients exhibit fat concern1 and atypical AN (NFAN) occurs in Hong Kong.19 A previous study found that 41 (59%) of 70 Chinese anorexic patients, despite a resemblance to their western counterparts, attributed food refusal to stomach bloating, loss of appetite, no hunger, and other non-fat phobic rationale.19 It has also been shown, using the EDI, that fat-phobic and non-fat phobic anorectic patients are similar except on the drive for thinness subscale.15 Our study also found that typical and atypical AN subjects are similar in every way except the weight concern subscale. Thus, from a cross-cultural perspective, it is imperative that the diagnostic criteria for AN be re-examined. According to Hsu and Sobkiewicz,20 the general assumption that perceptual body weight distortion is pathognomic for eating disorders deserves re-examination and clarification.
Eldredge and Agras21 showed that individuals with BED expressed greater concerns about weight and shape than non–eating disordered controls. Likewise, this study found that subjects with BED scored significantly higher than controls on items dealing with weight concern and shape concern. This finding suggests that the absence of any cognitive criteria in the DSM-IV Research Criteria for BED is an issue of concern. Some other researchers have highlighted the importance of and the need to consider cognitive diagnostic criteria for BED as well.22 Our results provide cross-cultural evidence that cognitive features of weight and shape concern should be considered diagnostic criteria for BED as in the DSM-IV diagnostic criteria for AN and BN.
In the DSM-IV,6 excessive exercise is listed as one of the symptoms of BN. It is very interesting that in our study, none of the subjects and controls fulfilled the Oxford definition of excessive exercise. These findings are not compatible with previous findings of a positive association between exercise quantity and eating disorder symptoms.23,24
A possible explanation for this incompatibility may be that the Oxford definition is not appropriate for our population and that the level of exercise defined as excessive may be too high for our population. A cross-cultural comparison study found that Chinese subjects in Hong Kong report doing significantly less exercise than Chinese Americans in the United States.25 Moreover, a 5-year local study involving 13,025 people aged between 18 and 70 years showed that 80.5% were physically inactive and that 54% walked for less than an hour a day.26
Additionally, in the CC-EDEI, the quantity of physical activity is considered rather than the quality. Exercise becomes compulsive when it is characterised by a sense of obligation to exercise. In a multivariate analysis, compulsion to exercise was a positive predictor of disordered eating symptoms.27 An alteration in the means of assessing unhealthy exercise as a symptom of eating disorders could be achieved by using ‘compulsive’ as a more clinically useful characterisation than ‘excessive’. Future study should focus on compulsive elements of exercise like a rigid exercise schedule, detailed record keeping, and feelings of guilt and anxiety over missed exercise sessions.28 This is analogous to the assessment of ‘dietary rules’ with the compulsive dimension being asked in EDE (‘How have you felt about breaking them? How would you have felt if you had broken one of your dietary rules?’).10
In 2003, according to the HEDA, 369 clients phoned in to seek help for eating problems. Of these, 62 patients were identified as having AN and another 117 patients classified as having BN. The remaining 190 clients had an eating disorder with impairment of physical health or
psychosocial functioning but not the full criteria for AN or BN (personal communication, Director of HEDA). A similar pattern was seen during recruitment for this study. Clients presenting consecutively to HEDA and a university-affiliated clinic were recruited from January to September 2005. During this period a total of 101 people attended the 2 sites but only 42 patients fulfilled the DSM- IV criteria for AN, BN, BED, or NFAN. The remaining 59 attendees (58.4% of clients seeking treatment for eating problems) suffered from EDNOS: conditions that meet the definition of an eating disorder but not the criteria for AN or BN.17 The clinical features of these 59 attendees closely resembled those of AN or BN but they did not meet the full diagnostic criteria for AN or BN, either because one necessary diagnostic criterion was missing or, because one or more of the criteria were not severe enough to reach the specified threshold.
Although EDNOS is the most common category of eating disorder encountered in routine clinical practice, it has rarely been studied.29 Thus, the needs of a large proportion of people seeking treatment for eating disorders have received less empirical attention. Moreover, by focusing on AN, BN, and BED only, researchers and clinicians have failed to view eating disorders in their entirety.17 In the future more attention should be paid to the development of a measurement tool for EDNOS.
Acknowledgements
The authors would like to thank Prof CG Fairburn, Prof Kelly Lai, Ms Philipa Yu, Mr Adley Tsang, and medical students for supporting this study. Material support from the Hong Kong Eating Disorders Centre, the Hong Kong Eating Disorder Association, the Prince of Wales Hospital is gratefully acknowledged.
References
- Lee S, Katzman MA. Cross-cultural perspectives on eating disorder. In: Fairburn CG, Brownell KD. Eating disorders and obesity. New York: Guildford; 2002:260-4.
- Peterson CB, Miller KB. Assessment of eating disorders. In: Wonderlich S, Mitchell J, De Zwann M, Steige H, editors. Eating disorders review Part 1. Abingdon (UK): Radcliffe Publishing; 2005:105-26.
- Lee S, Ho TP, Hsu LK. Fat phobic and non-fat phobic anorexia nervosa: a comparative study of 70 Chinese patients in Hong Kong. Psychol Med 1993;23:999-1017.
- Wilson GT. Assessment of binge eating. In: Fairburn CG, Wilson GT, editors. Binge eating: nature, assessment and treatment. New York: Guildford; 1993:227-49.
- Fairburn CG, Beglin SJ. Assessment of eating disorders: interview or self-report questionnaire? Int J Eat Disord 1994;16:363-70.
- Diagnostic and statistical manual of mental disorders. 4th ed. Washington, DC: American Psychiatric Association; 1994.
- Anderson DA, Paulosky C. Psychological assessment of eating disorders and related features. In: Thompson JK, editor. Handbook of eating disorders and obesity. New York: John Wiley & Sons; 2004:112- 29.
- Franko DL, Schumann BC, Barton B. Stability of the factor structure of the Eating Disorder Inventory in black and white adolescents girls. Poster presented at the Eating Disorder Research Annual Meeting, Charleston SC; 2003 Nov 20-23.
- Striegel-Moore RH, Franko DL, Barton BA. Factor structure of the Eating Disorders Inventory. Poster presented at the International Conference on Eating Disorders; 2002 Apr 25-28; Boston MA.
- Fairburn CG, Cooper Z. The Eating Disorder Examination (12th ed.). In: Fairburn CG, Wilson GT, editors. Binge eating: nature, assessment and treatment. New York: Guildford; 1993:317-32.
- Garner DM. Measurement of eating disorder psychopathology. In: Fairburn CG, Brownell KD, editors. Eating disorders and obesity. New York: Guildford; 2002:141-6.
- Cooper Z, Cooper PJ, Fairburn CG. The validity of the eating disorder examination and its subscales. Br J Psychiatry 1989;154:807-12.
- Rizvi SL, Peterson CB, Crow SJ, Agras WS. Test-retest reliability of the eating disorder examination. Int J Eat Disord 2000;28:311-6.
- Grilo CM, Masheb RM, Lozano-Blanco C, Barry DT. Reliability of the Eating Disorder Examination with binge eating disorder. Int J Eat Disord 2004;35:80-5.
- Lee S, Lee AM, Leung T. Cross-cultural validity of the Eating Disorder Inventory: a study of Chinese patients with eating disorders in Hong Kong. Int J Eat Disord 1998;23:177-88.
- Weiss MG. Eating disorders and disordered eating in different cultures. Psychiatr Clin North Am 1995;18:537-53.
- Fairburn CG, Walsh BT. Atypical eating disorders (eating disorders not otherwise specified). In: Fairburn CG, Brownell KD, editors. Eating disorders and obesity. New York: Guildford; 2002:171-7.
- Beumont PJ, Kopec-Schrader EM, Talbot P, Touyz SW. Measuring the specific psychopathology of eating disorder patients. Aust N Z J Psychiatry 1993;27:506-11.
- Lee S, Chan YY, Hsu LK. The intermediate-term outcome of Chinese patients with anorexia nervosa in Hong Kong. Am J Psychiatry 2003;160:967-72.
- Hsu LK, Sobkiewicz TA. Body image disturbance: time to abandon the concept for eating disorder? Int J Eat Disord 1991;10:15-30.
- Eldredge KL, Agras WS. Weight and shape overconcern and emotional eating in binge eating disorder. Int J Eat Disord 1996;19:73-82.
- Masheb RM, Grilo CM. Binge eating disorder: a need for additional diagnostic criteria. Compr Psychiatry 2000;41:159-62.
- Davis C, Fox J, Cowles M, Hastings P, Schwass K. The functional role of exercise in the development of weight and diet concerns in women. J Psychosom Res 1990;34:563-74.
- Richert A, Hummers J. Patterns of physical activity in college students at possible risk for eating disorders. Int J Eat Disord 1986;5:757-63.
- Davis C, Katzman MA. Chinese men and women in the United States and Hong Kong: body and self-esteem ratings as a prelude to dieting and exercise. Int J Eat Disord 1998;23:99-102.
- Ko TC. HK eating and lazing its way to early grave. South China Morning Post. 2005 Oct 21.
- Adkins EC, Keel PK. Does “excessive” or “compulsive” best describe exercise as a symptom of bulimia nervosa? Int J Eat Disord 2005;38:24- 9.
- Wyatt LM. Obsession-compulsiveness and disordered eating in obligatory and non-obligatory exercisers [dissertation]. Los Angeles: California School of Professional Psychology; 1997.
- Fairburn CG, Bohn K. Eating disorder NOS (EDNOS): an example of the troublesome “not otherwise specified” (NOS) category in DSM-IV. Behav Res Ther 2005;43:691-701.