Hong Kong J Psychiatry 2001;11(4): 17-21
ORIGINAL ARTICLE
L Li, D Young, Z Hu
Acknowledgements: This study was supported by the World Health Organization (WHO/MNH/CHN/95/01). We wish to thank Prof C David Jenkins of the Department of Psychiatry, University of North Carolina, and Dr Doris F Chang of the Department of Psychology, University of California, Los Angeles, for their helpful advice in preparing this manuscript.
Dr L Li, MD, PhD, Mental Health Institute, Hunan Medical University, Changsha, China
Dr D Young, MD, Mental Health Institute, Hunan Medical University, Changsha, China
Dr Z Hu, MD, Mental Health Institute, Hunan Medical University, Changsha, China
Address for correspondence: Dr Lingjiang Li , MD, PhD, Mental
Health Institute, Hunan Medical University, Changsha, China
Submitted: 01 December 1999; Accepted: 01 March 2001
Abstract
The purpose of this study was to conduct a longitudinal examination of various dimensions of quality of life for patients following their first stroke and to identify variables that predict subsequent quality of life. 121 patients with a first stroke and 121 matched healthy controls from the same community were assessed at baseline and 1 year after discharge from hospital using a self-administered General Quality of Life Inventory.
One year after discharge, the clinical condition of 84% of patients following a stroke had improved or they had fully recovered. However, their quality of life had not reached the level of the healthy controls. Of note was that 16% of patients whose stroke symptoms were unchanged or worse after 1 year of follow-up showed no change in quality of life scores compared with baseline. One year after discharge, family and social support had significantly decreased and self esteem and body image were impaired compared with baseline, particularly for patients experiencing deterioration of their condition.
Multiple stepwise regression analysis showed that quality of life was best predicted by the severity of the stroke, patients’ outcome expectancy, their values of need level for life, and potential for neuroticism. Stroke was found to impair most aspects of patients’ quality of life. During rehabilitation after stroke, more attention should therefore be paid to adjusting patients’ outcomes expectancy and their values of need level for life to a more realistic level and ensuring sufficient psychosocial support as well as active drug and physical therapy.
Key words: Stroke, Quality of life
Introduction
Stroke is a major chronically disabling brain trauma that often radically and permanently changes the lives of patients. Most strokes are not fatal, but the disabilities caused may be profound and lead to severe impairment of quality of life (QOL).1-4 Gage et al3 and Solomon et al4 reported that the QOL of a patient after a moderate or major stroke is perceived as worse than or equal to death by many patients. Hence, there is a growing consensus that QOL should be considered as an important index of health care outcome.
However, despite the potential for stroke to affect multiple domains of life and related outcomes, few studies have addressed QOL after stroke. Some reported studies have reached contradictory conclusions.5-7 However, nearly all research into QOL after stroke has failed to include a comparison group of healthy adults.4,5,8-12
Over the years, QOL has been def ined in many different ways. A broad consensus has emerged that at least 4 dimensions should be included in a QOL assessment: physical, psychological, social function, and patients’ symptoms.1,2,13,14 This study, therefore, was undertaken to compare the QOL of patients after stroke with healthy controls, and to prospectively examine the QOL of patients followed up during a 12-month period after discharge from hospital using a multidimensional measure that includes physical health, psychological health, social functioning, and living conditions.1,2,14,15
Methods
Patients
Patients were included in the study as long as the following criteria were met.
The patients were discharged from hospital within 1 week of improvement in their condition after a f irst stroke. There were no other neuro-musculoskeletal conditions that would interfere with normal function and the patients had no previous history of psychiatric illness. Cognitive and language functioning was adequate for participation in the study procedures. Patients could read and write Chinese and were well enough to give informed consent. The diagnosis of stroke was conf irmed clinically and by computed tomography.
The control subjects were matched in terms of the patients’ age groups (<45 years, 45 to 65 years, >65 years), gender, and occupation (manual worker, farmer, off ice worker, professional, other) by healthy individuals from the same community who had no history of seeking medical attention during the previous year.
Materials
A 64-item self-administered form of the General Quality of Life Inventory (GQOLI) was used (the validity, reliability, and sensitivity have been described in detail elsewhere16,17). The GQOLI assesses physical health, psychological health, social functioning, and living condition dimensions, which are further divided into 16 factors. Each item is rated on a 5-point scale. Higher scores denote better QOL.
The Related Factors of Quality of Life Checklist (RFQC) includes the following 4 variables: hierarchy system of perceived needs for future life, the value of needs, referential standard compared with current life, and neuroticism and extroversion personality traits.18
The Symptom Checklist for stroke patients includes 15 symptoms related to stroke and side effects of treatment.17 Each symptom is rated on a 5-point scale with a score of 5 representing a normal condition and 1 representing a severe condition.
Stroke severity was defined in terms of level of handicap assessed by the Clinical Rating Scale for Handicap in Nervous System Functioning (CRSH) (Edinburgh and Scandinavian research criteria).19 Higher scores denote greater stroke severity or poorer functioning.
Outcome variables were identified according to the sum of the changed values of scores on the CRSH and the Global Function Rating Scale (global function is rated on a 7-point scale, whereby 1 represents normal and 7 represents death) 1 year after discharge compared with baseline. Outcomes of stroke were divided into 4 grades of deterioration, no change, improvement, and recovery.19
Statistical Analysis
The investigators requested patients to complete all the instruments at 2 points in time — 1 week before dis- charge from hospital (average, 37.9 days after the stroke occurred) and 1 year after discharge. The healthy controls were assessed for baseline data with the GQOLI and RFQC.
During the 1-year period after discharge, patients received stroke rehabilitation and prophylactic therapy such as antihypertensive agents, aspirin, and physical therapy. Patients were asked not to use alcohol and cigarettes.
Results
Demographic Characteristics
128 patients and 128 matched controls were assessed for baseline data before discharge from hospital. The controls were assessed throughout the study enrolment period. At the second data collection period (1 year after discharge from hospital), 7 patients (5.5%) had withdrawn from the study. Therefore, the sample reported here represents 94.5% of the 128 patients and their matched controls who entered the study.
The mean age of the 121 patients who completed the 1- year follow-up was 60.4 ± 8.1 years (range, 35 to 85 years). The average duration of illness (from stroke to predischarge evaluation) was 79.6 ± 82.5 days (range, 20 to 167 days) and the mean duration of admission of hospital was 37.9 ± 28.2 days (range, 18 to 64 days). The mean score of the CRSH was 4.7 ± 3.9 (range, 2 to 9). Sixty three patients were male (52.1%) and 58 were female. Fifty six patients had a haemorrhage-type stroke (46.3%), and the remaining 65 had an infarction-type stroke.
Quality of Life
At baseline, the scores for the physical health dimension were significantly lower for the patients than the controls for the 4 factors (Table 1). With the exception of self esteem and body image factors, the scores for the psychological health dimension and other factors were signif icantly lower for the patients than the controls.
With regard to the social functioning dimension, the scores for the social support and communication factors were notably higher for the patients than the controls and the scores for the recreation and working factors of the social functioning dimension were lower for patients than controls. There were no significant differences in the scores for marriage and family relationship factors between the 2 groups. On the other hand, the score for income and consuming factor of living conditions dimension was signif icantly lower for the patients than the controls.
The patients were divided into 2 groups according to stroke type to compare the quality of life between these groups. At baseline, no signif icant difference was found between patients with haemorrhage- and infarction-types of stroke for almost all factors of the GQOLI, with the exception of cognitive functioning. For this factor, the score was signif icantly lower for patients with haemorrhage-type stroke (9.67 ± 2.14) than for those with infarction-type stroke (12.19 ± 2.08; t = 4.39; p < 0.01).
One year after discharge, the scores for positive and negative feelings were lower for the patients with haemorrhage-type stroke (10.12 ± 2.03) than for those with infarction-type stroke (12.78 ± 2.34; t = 2.48; p < 0.05). There was no signif icant difference between the 2 groups for the other factors.
Patients were then grouped according to the outcome assessment of stroke 1 year after discharge. For the patients whose condition deteriorated, the scores for positive and negative feelings, self esteem and body image, social support and communication, and marriage and family relationship factors were lower 1 year after discharge than they were before discharge (Table 2).
For the patients who improved or recovered, the scores for the self esteem and body image, and social support and communication factors remained significantly lower despite the improvement in physical function during the follow-up period. Furthermore, the scores for the remaining factors of the QOLI and Symptom Checklist (except for marriage and family relationships) signif icantly increased by the end of the year compared with baseline, although the scores for most of the factors of the QOLI for the patients who improved or recovered had still not reached the normal level of the matched controls.
Hierarchy System of Needs and Referential Standard of Life
Each patient was asked to choose 1 to 3 items representing their main needs or desires in life and 1 referential standard for life. At baseline, the responses indicated that the highest priority needs or desires for life among the patients were good physical health (88.8%), wealth (27.0%), and realisation of self worth (14.6%). However, among the control group, the highest priority needs or desires for life were wealth (44.4%), happy family and marriage (39.3%), and good physical health (27.1%). The means of values of need level for overall life were 2.73 ± 1.56 for the patients and 3.24 ± 2.11 in the controls (t = 3.27; p < 0.01).
Forty one percent of the patients compared their present life with an ‘ideal self standard for life’, 37.0% with ‘previous self conditions’, and 21.4% with ‘conditions of other people’, while only 14.7% of controls compared their present life with ‘ideal self standard for life’, and 36.4% with ‘previous self conditions’, although 48.9% of controls compared their life with ‘conditions of other people’. There were signif icant differences between the patients and the controls (c2 = 8.57; DF = 2; p < 0.025).
Multiple Regression Analysis of Factors Affecting Quality of Life
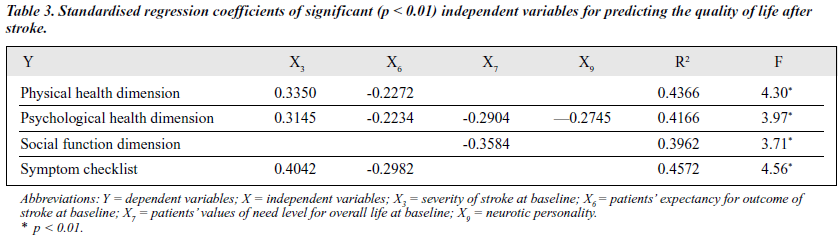
According to the theoretical possibility and the results of the univariate analyses, the change values (between 1 week before discharge and 1 year after discharge) of each dimension in GQOLI and Symptom Checklist as dependent variables (Y) were selected. The independent variables were age (X1 ), sex (X2 ), severity of stroke at baseline (X3 ), stroke type (X4 — the values of the variables were coded as 1 for haemorrhage-type stroke and 2 for infarction-type stroke), duration of illness (X5 — from stroke to predischarge evaluation), patients’ expectancy for outcome of stroke at baseline (X7), patients’ values of need level for overall life at baseline (X6 ), reference standard of life at baseline (X8 — the values of the variables were coded for ‘conditions of other people’ as 1 for no and 2 for yes), neurotic personality (X9), and extrovert personality (X10). As shown in Table 3, quality of life was best predicted by the severity of stroke, patients’ expectancy value for stroke outcome, patients’ values of need level for overall life, and Eysenck’s neuroticism personality scale.
Discussion
From this study, it can be seen that patients with stroke continue to report substantial impairment for most areas of QOL, including physical health, psychological health, social functioning, and income and consuming factors of the living conditions dimension when compared with healthy controls, despite the results of clinical examination and CRSH evaluation showing that their clinical conditions had improved at discharge. One year after discharge, the clinical conditions of most patients (84.3%) had further improved or they had fully recovered according to the evaluation of outcome criteria. However, most aspects of physical and psychological health dimensions and working conditions of the social dimension of QOL had not reached the normal level of healthy controls, although their scores on most factors of QOLI had risen signif icantly compared with baseline levels of QOL before discharge.
It was striking that, at baseline, patients did not experience more mar riage and f amily relationship impairment and they received more social support and communication than healthy controls (Table 1). However, 1 year after discharge, the scores for social support and communication, and marriage and family relationship factors for patients whose condition deteriorated were signif icantly lower than for healthy controls. For the patients whose condition improved or who recovered, these f actors decreased to normal.
One explanation considered for the decrease of social and family support over time is the long-term duration of stroke and the family burden of caring for the patients. At the time of onset of first stroke, the cohesion among family members may increase due to stress.20 During the short hospital admission period (mean, 37.63 ± 28.16 days), patients may have perceived more physical and psychosocial support.
As time passes, the long-term burden of taking care of a patient with stroke could impair family cohesion. Family caregivers have to work and pay the family expenses as well as caring for these chronically disabled patients. Meanwhile, the family carers may have less support and intimacy, including a low-quality sexual life (Tables 1 and 2), from the patient than before the onset of the stroke. This could subsequently lead to a decrease in the carers’ support for the patients. On the other hand, the long duration and chronicity of stroke results in negative feelings and low self esteem for patients,5,7,8,12,21 which may impair patients’ perceptions of the perceived social and family support.
Another important finding from this study was that the patients did not exhibit more self esteem and body image impairment compared with healthy controls at baseline. However, the score for this factor of QOL increasingly lowered over time. At 1 year after discharge, all patients had a lower self esteem and body image than healthy controls. Some researchers have reported that normal self esteem and body image in stroke patients may be related to neurological disturbances in terms of neglect of body contour, impaired awareness of the disease,7 and enjoyment of increased social support after stroke.21
In this study, we also found that the scores for social support and communication, and marriage and family relationship factors were parallel with the score for the self esteem and body image factor. Therefore, it is further identif ied that social and family support plays a critical role in promoting patients’ behavioral change and psychological adjustment for coping with stroke.7
How can QOL of patients be improved after stroke? As seen in Table 2, one year after discharge, patients whose conditions improved or who were rehabilitated reported signif icant improvements for nearly all aspects of QOL; whereas the patients whose conditions deteriorated or did not change evaluated their QOL as lower for some aspects or unchanged for others.
Most importantly, as expected, the multiple regression analysis also demonstrated that among all the indepen- dent variables, severity of the stroke was a key predictor, being positively related to the physical and psychological health dimensions of QOLI. These f indings suggest that severity of stroke — mainly the severity of neurological def icits and physical disability — is closely linked with QOL, although it is not the only factor affecting QOL. Another important factor related to QOL was level of needs for overall life.
Calman suggested that QOL was the gap or disparity between one’s needs and achievements.22 Thus, the narrower the gap, the higher the quality of life perceived. Specif ically, when disease is severely experienced by an individual, almost all aspects of life become health-related. In this study, 88.8% of patients regarded ‘good physical health’ as their main need in life compared with 27.1% of healthy controls. Obviously, on the one hand, improving the therapeutic effects can lessen the gap and therefore improve patients’ QOL, while, on the other hand, lowering the value of needs level for life may be an important way to improve QOL. From our multiple regression analysis (Table 3), we found that higher self evaluations of QOL, especially with regard to psychological health, were related to a lower expectancy for outcome of stroke or lower need level for overall life. After having a stroke, patients may consciously adjust their needs and decrease the value of need level for life in order to cope with the stress of stroke and thus keep their subjective life perception on a psychologically bearable level. Indeed, this study found that the value of need level for overall life for the patients was signif icantly lower than that for the controls.
In summary, in the process of a patient’s rehabilitation after stroke, in addition to receiving active drugs and physical treatment, more attention should be paid to adjusting a patient’s expectancy for outcome of stroke or need for overall life to a more realistic level. Suff icient psychosocial support, enabling patients to be realistic in their self evaluation of their post-stroke restrictions and increasing their chances of fulfilling their responsibilities and enjoying life to the full, is essential.
References
- Orley J, Kugken W. Quality of life assessment: international perspec- tives. Berlin: Springer Verlag; 1994.
- Spliker B. Quality of life assessments in clinical New York: Raven Press, Ltd; 1990.
- Gage BF, Cardinalli AB, Owens DK. The effect of stroke and stroke prophylaxis with aspirin or warfarin on quality of life. Arch Intern Med 1996;156:1829-1836.
- Solomon NA, Glick HA, Russo CJ, Lee J, Schulman KA. Patient pre- ferences for stroke outcones. Stroke 1994;25:1721-1725.
- Niemi ML, Laaksonen R, Kotila M, Waltimo O. Quality of life 4 years after stroke. Stroke.1988;19:1101-1107.
- Ablsio B, Britton M, Murray V, Theorell T. Disablement and quality of life after stroke. Stroke 1984;15:886-890.
- King RB. Quality of life after stroke. Stroke 1996:27:1467-1472.
- Osberg JS, Dejong G, Haley SM, Seward ML, McGinnis GE, Germaine J. Predicting long-term outcome among post-rehabilitation stroke patients. Am J Phys Med Rehabil 1988;67:94-103.
- Viitanen M, Fugl-Meyer KS, Bernspang B, Fugl-Meyer AR. Life satisfaction in long-term survivors after stroke. Scand J Rehabil Med 1988;20(1):17-24.
- Wade DT, Legh-Smith J, Hewer RA. Depressed mood after stroke. Br J Psychiatry 1987:151:200-205.
- de Haan R, Aaronson N, Limburg M, Langtom Hewer R, Van Crevel Measuring quality of life in stroke. Stroke 1993;24:320-327.
- de Haan RJ, Limburg M, Van der Meulen JH, Jacobs HM, Aaronson NK. Quality of life after stroke: impact of stroke type and lesion location. Stroke 1995;26:402-408.
- Feigenson JS. Stroke rehabilitation: effectiveness, benef its, and cost. Some practical considerations. Stroke 1979;10:1-3.
- Frisch MB, Cornell J, Villanueva M. Clinical validation of the quality of life inventory. Psychological Assessment 1992;4:92-101.
- World Health Organization. The development of the WHO quality of life assessment instrument. Geneva: World Health Organization, 1993.
- Li L, Wei H, Young D. The development of the General Quality of Life Inventory in China. Chin Ment Health J 1995;9(5):227-231.
- Li L, Young D, Hu Z. The development of quality of life inventory for cerebral apoplexy patients. Chin J Behav Med Sci 1997:6(1):4-8.
- Yaoxian G. Manual of the Eysenck Personality Questionnaire (EPQ for adults). Changsha: Hunan University Press; 1981.
- Mong J. The comment upon the clinical trails of stroke. Chin J Neurol Psychiatry 1988;21(1):57-58.
- Li L, Young D. Life event, family behavior style and marital stability. Chin Ment Health J 1990;4(6):257-261.
- Friedland J, McColl MA. Social support and psychosocial dysfunction after stroke: buffcring effects in a community sample. Arch Phys Med Rehabil 1987;68:475-480.
- Calman KC. Quality of life in cancer patients: an hypothesis. J Med Ethics 1984;10:124-127.