Hong Kong Journal of Psychiatry (1998) 8 (1) 33-37
Mental Health and Services
Summary
A prospective three-year control study was canned out in Nanshi district of Shanghai, People’s Republic of China. It aimed to assess the long-term effectiveness of group psychosocial education program for relatives of schizophrenic patients in the community. The experimental group consisted of relatives of 251 patients. They were given a psycho-social education program which included 16 lectures on mental illness and 7 group discussions. The control group consisted of relative of 158 patients. At the end of the third year, patients in the experimental group had lower relapse rate, higher rates of regular work and better social functioning than those in control group. While the relatives in the experimental group had less care burden; had more knowledge about schizophrenia and its treatment; and had relatively better mental and physical status. The education approach were well accepted by both relatives and mental health workers. It is concluded that more attention should be paid on psychosocial intervention in community – based psychiatric rehabilitation.
Key words: schizophrenia, community service, family intervention, psychosocial education, group therapy, Chinese
INTRODUCTION
Schizophrenia is a chronic psychiatric disorder with long illness duration and high relapse rate. It often resulted in impairment on psychosocial functioning. The development of modem psycho-pharmacology has significantly improved the patients' prognosis; has shortened the duration of hospital stay; and has made more discharges of patients hack to the community. Many of these schizophrenic patients were therefore be taken care of by their relatives in the community. However, this has created new challenges to these relatives. Questions on methods of rehabilitating patients in the community, reducing their relapse rate and methods to reduce the care burden and to avoid psychosomatic impairment on family members were often raised.
In the last ten years, many researches have focused on interventions with families of schizophrenic patients. Particularly, the researches on expressed emotion (Brown, 1997; Leff, 1982; Vaughn7 1976) have revealed that high levels of expressed emotion can often precipitate relapses. Family intervention measures have therefore been developed with the hope to reduce the levels of expressed emotion in the families of these patients. Such individual family treatment and intervention required the skills of specially trained therapists. But in the developing country like the People's Republic of China, they obviously have difficult to be applied them widely because of the shortage of specialists as comparing to the huge patient volume.
We have developed a 3-years group psychosocial education program for the relatives of schizophrenics in Nanshi district of Shanghai. The results of first-year and second-year were positive in improving effectiveness of both schizophrenic patients and their family members (Zhang, 1993). The present paper described the results of the three-year follow up of these patients and their relatives after completing the education program.
METHODOLOGY
SAMPLE
By random cluster sampling method, a probability sample of patients was drawn from the community patient registration centers. The criteria for enroll-ment into the study were: (1) diagnosed as suffering from schizophrenia basing upon the Chinese Classif-ication and Diagnostic Criteria of Mental Disorders (CCMD-2), which is similar to lCD-10 and DSM-IV; (2) aged between 16 to 59; and (3) living with at least one relative who could participate in the
group education program. All patients in the probability sample who met enrollment criteria were randomly divided into two groups: experimental group and control group according to the ratio 2:1. Families in experimental group were given the psychosocial education program in addition to the routine community mental health services while the control group received routine services only.
EDUCATIONAL PROGRAM
There were sixteen lectures plus group discuss-ions for family members during the three years' period, eight in the first year four in the second years and four in the third year. The lectures were tilled: (1) psychosis and schizophrenia; (2) strategies for coping with patients' psychotic symptoms and behavior; (3) psychotropic drugs: their dosage & side effects; (4) early symptoms of relapse and its prevention; (5) reduction of stress at home, at work, and in the community; (6) marriage and family planning for psychotic patients; (7) supervision and care of psychotic patients; (8) methods of social and vocational rehabilitation; (9) long-term antipsychotic medication and its maintenance; (10) principles of family self-help organization; (11) promotion of mental health of caregivers; (12) promotion of psychosocial rehabilitation; (13) antipsychotics and compliance; (14) reduction of psychiatric disability on patients' social functioning; (15) knowledge of patients' quality of life; and (16) reviews and principles of adapting with environment and social integration. Where were also seven sessions of group discussion arranged separately during the three years. The lectures were of 60 minutes duration each and there were unlimited time for questions and free discussion. They were delivered by trained psychiatrists or nurses in groups of 20 to 40 relatives.
ASSESSMENT INSTRUMENTS
The major assessment instruments applied in this research were: (1) a questionnaire (designed by the researchers) - to evaluate the severity of the illness and symptoms; (2) the Psychiatric Disability Assessment Schedule (WHO/DAS) (WHO, 1988) - to evaluate the social role function of patients; (3) the Family Burden Interview Schedule (PS) (Pai et. al. , 1981) - to assess the difficulties of the families resulted from caring for the patients; (4) a quiz on knowledge about mental illness (designed by the researchers) - to test relatives' extent of knowledge about mental disorder; and (5) the General Health Questionnaire (GHQ-28, Goldberg) - to assess the level of psychosomatic health status of the relatives. Time for assessment were at enrollment, and at 1, 2 and 3 year.
RESULTS
COMPARISON OF COMPLETED SAMPLE
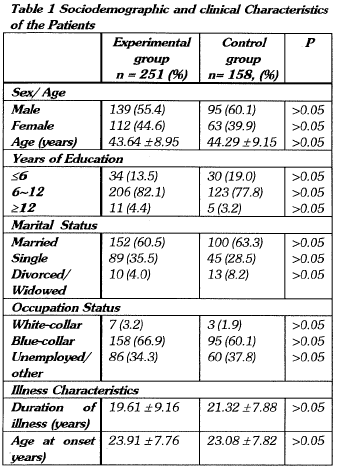
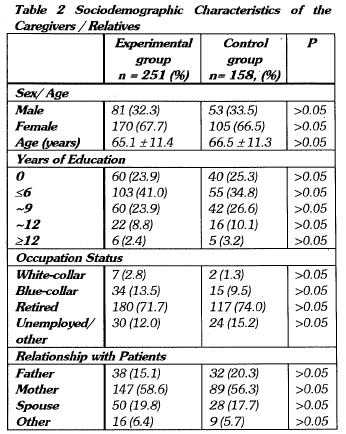
At total of 409 subjects completed the program, of which 251 were in the experimental group and 158 were in the control group. Table 1 & 2 shows the characteristics of the patients and their relatives. There were no significant differences between the experimental and control groups of patients and relatives in terms of sex, age, educational level, occupation and other sociodemographic characteristic.
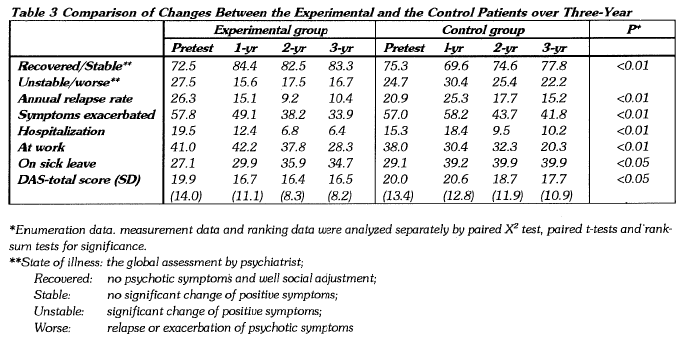
EFFECTS ON PATIENTS
At the end of third year, the experimental group showed a higher rate of recovery and stabilizaltion of condition, a lower rate of exacerbation of symptoms and a reduction in annual relapse rate and hospitalization rate (p<0.01) when compared with the control.
Improvement were also made in some degree in the total score on DAS and sick-leave days (p<0.05). The above results suggested that group psychosocial education program could enhance the rehabilitation of the mentally ill patients doubtlessly (see table 3).
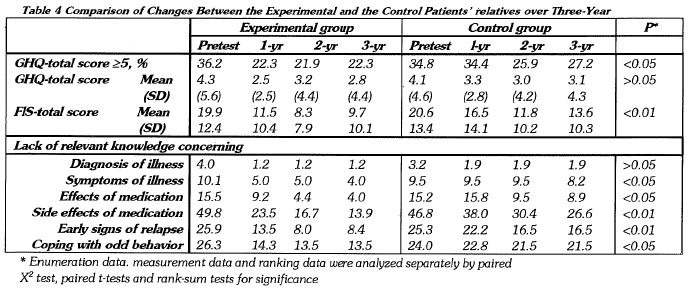
EFFECTS ON RELATIVES
The group psychosocial education program showed its effects on the relatives mainly in two areas. One was a reduction of care burden and the other was a great increase in knowledge of mental illness (see table 4).
Comparing the changes over the three years, the relatives in the experimental group had less care burden
(p<0.01) than those of the control. Their PS-total score decrease by 10.2% in the three years' period. They got more knowledge in the understanding and caring of patients with schizophrenia. The quiz on knowledge about mental illness showed that about 86.1% to 98.80/6 of relatives had knowledge and skill of coping with schizophrenia (p<0.05 to p<0.01) GHQ was used to assess the psychosomatic health status for relatives. Although there was no significant difference between two groups on the average total score, the number of subjects scored greater than 5 on GHQ decreased more significantly in experimental group.
DISCUSSION
Most of the previous researches related to schizophrenic family education have neither been carried out on large sample size nor have been followed up for long duration. Therefore, data on long term systematic follow-up were lacking (Tarrier, 1988; Gittelman, 1990; McGill et al, 1989). We and many researchers have pointed out that effectiveness of short term intervention was obviously not enough for a chronic disease such as schizophrenia. Therefore, we designed this three-year systematic intervention on schizophrenic family.
To answer the question on whether a longer family education program were more beneficial to the patients. The answer was positive. A "relapse" was defined as the recurrences of symptoms or the exacerbation of residual symptoms that required a modification of the medication. The annual rate in experimental group has been declined from 26.3% to 10.4% in the three years' period (p <0.01); while the rate in control group who received only routine community service showed no significant change (from 20.9%: to 15.2%, p>0.05).
Similar changes were found in other indexes of illness such as the rate of relief and the number of hospitalizations, etc. The social functioning of the experimental patients also improved significantly as indicated by the DAS total score and number of sick-leave days.
Another purpose of family education program was to help the relatives of patients. The majority of the educational program contents were about the knowledge of mental disorder, for example, the concepts and manifestations of the illness, the effects and side effects of the treatment especially the medication, the recognition and coping with the abnormal behavior etc. So we would expect the relatives' psychological and psychosomatic distress be relieved by enhancing their knowledge about the disorder. It could be said that the target above was reached in certain degree in term of the changing of the total score of F'S and the proportion of high score in GHQ.
One of the main contents of family education was to explain the importance of taking antipsychotic drugs regularly under the supervision of doctors and thus to increase the treatment compliance of the patients. The rate of regular medication maintenance in patients of the experimental group was 81.3% which was statistically higher (p<0.05) than that of the control group of 72.7% at the end of the third year. We considered that the rehabilitation plan for schizophrenia should include both drug therapy and family education as well as other psychosocial intervention.
There were some limitations in the present project. Group psychoeducation could only deal with the common questions from relatives, but do little for special problems of individual family. Tine areas on changing illness behavior and training in social communication skill were less discussed in our program and therefore the rehabilitation of social functioning of patients was not as satisfactory as we have hoped. The total scores on DAS were still rather high at the end of the third year in patients of the experimental group. Furthermore, we also found that the improvement in the third year was not as great as in the first year in general.
Certainly, it was not fair for family educational program to resolve all the rehabilitation problems of schizophrenia. Our experiences indicated that group family psychoeducation was effective and easy to carry out in practice. It should be a good approach of mental health service to include group support, more intensive intervention and loner-term follow-up.
CONCLUSION
The Group Psychosocial Education program (GPE) as a kind of community mental health service was feasible. The approach of GPE were also well accepted by mental health workers in community.
The long term (over three-year) effectiveness of GPE was obvious and had played a definite role in the treatment of patients with schizophrenia.
This program also helped the relatives or caregivers in reducing their psychological burden and psychosomatic distress. This was achieved by learning more about mental disorder.
There are some limitations in our project. It only dealt with the common questions but was unable to help individual families with special problems in general. The improvement in the third year was not as great as in the first year.
Although drug therapy is the major treatment method for schizophrenia at present, much attention should also be paid to psychosocial intervention in community-based psychiatric rehabilitation.
ACKNOWLEDGEMENT
This research was partially supported by World Health Organization and World Association of Psychosocial Rehabilitation.
REFERENCES
Brown GW, Birley JLT, Wing JK. (1997) Influence of family life on the course of schizophrenic disorders: A replication. British journal of Psychiatry 121: 241.
Gittelman M, Dubuis J, Nagaswami V, et al. (1990) Mental health promotion through psychosocial rehabilitation. International Journal of Mental Health 18: 99.
Leff JP, Berkowitz R, Eberlein-Vries, Sturgeon D. (1982) A controlled trial of social intervention in schizophrenic families. British journal of Psychiatry 141:121.
Leff JP, Berkowitz R, Shachan A, et al. (1989) A trial of family therapy via a relatives' group for schizophrenia. British Journal of Psychiatry; 154: 58.
McGill CW, Falloon IRH. Boyd JL, et al (1983) Family educational intervention in the treatment of schizophrenia. Hospital & Community Psychiatry 34: 934.
Pai S, Kapur Rl (1981) The burden on the family of a psychiatric patient. Development of an interview schedule. British Journal of Psychiatry 138: 332.
Tarrier N, Barrowclough C, Vaughn C, et al (1988) The community management of schizophrenia: A controlled trial of a behavioural intervention with families to reduce relpase. British Journal of Psychiatry 153: 532.
Vaughn CE, Leff JP. (1976) The influence of family and social factors on the course of psychiatric illness: A comparison of schizophrenia and depressed neurotic patients. British Journal of psychiatry 129:125.
World Health Organization (1988) Psychiatric Disability Assessment Schedule (WHO/DAS). Geneva: WHO.
Zhang M, Yan H.(1993) Effectiveness of psychoeducation of relatives of schizophrenic patients: A prospective cohort study in five cities of China. International Journal of Mental Health 22: 47-59.
*Zhang, Ming-yuan MD Chairman, Chinese Society of Psychiatry; Psychiatrist-in-chief, Shanghai Mental Health Centre
Zhu, Ziqing PhD Director, Department of Community Psychiatry, Shanghai Mental Health Centre
Yan, He-quin MD Psychiatrist, Shanghai Mental Health Centre
Song, Changchun MD Psychiatrist, Shanghai Health Centre
Lu, Fengzhen, MD Psychiatrist, Shanghai Mental Health Centre
*Correspondence: Professor Zhang Ming-Yuan, Shanghai Mental Halth Centre, 600 Wan Pin Nan Lu, Shanghai, China 200030, People's Republic of Chin