J.H.K.C. Psych. (1991) 1, 47-49
Summary
The characteristics of 69 children attending a Child Mental Health Clinic in St. James Settlement were described. The majority of them were found to be suffering from a definable psychiatric disease which required psychiatric intervention. The importance of this model of service was discussed.
INTRODUCTION
A child mental health clinic was set up in St. James' Settlement in March 1987. It was established by a joint effort of Family and Child Services Division of St. James' Settlement and Department of Psychiatry, University of Hong Kong. The major characteristic of this service was that it provided child psychiatric services for children below 12 years of age on a self-referral basis. It was felt that there was a need of such a service because:
(1) Parents wanted a more direct and easy approachable child psychiatric service by-passing the usual referral by doctors.
(2) Some parents were reluctant to bring their children to attend Psychiatric Clinics because of They were more at ease seeking help from social welfare agencies.
The clinic was the first of its kind in Hong Kong. All the cases were seen by either one of the first 2 authors. There was one half-day session per week and 2 new cases were seen per session. The clinic was well received and many parents phoned and enquired about the service. When they requested an appointment, they were put on the waiting list. No referral was necessary and no screening was done except that they were not receiving psychiatric intervention then. The waiting period was about 3-4 months. Treatment was done in the clinic. If intensive treatment was required, they would be referred to the University Psychiatric Unit.
The characteristics of children attending psychiatric clinic in Hong Kong have been studied by Luk & Lieh-Mak (1985) and Wong (1988). Both studies were done in psychiatric units attached to general hospitals with the majority of cases referred by medical practitioners. It had been found that only a small minority of the psychiatrically ill were treated by the specialist services (Rutter 1970). Thus these findings may not represent the general picture of childhood psychiatric problems in Hong Kong. In order to get a more complete picture of the childhood psychiatric problems in the community, studies involving different settings with different referral agencies are required. The Child Mental Health Clinic provided a good opportunity for such study.
The aims of the present study are:
(1) To study the characteristics of children attending the Child Mental Health Clinic
(2) To compare the fingings with other studies in Hong Kong
METHOD
All the children seen in the clinic from March 1, 1987 to December 31, 1987 were included as subjects.
In addition to the provision of clinical care, three questionnaires were used to study the characteristics of the sample:
(1) A pre-set demographic questionnaire to be completed by social workers of St. James' Settlement
(2)A symptom-check-list to be completed by the attending The symptom-check-list is a modified version of the "Item" sheet used in the Children Department of Maudsley Hospital in England, for clinical data register for children and adolescents (Thorley, 1982). The check list records clinical symptoms or signs which have occurred during the previous twelve months. The judgements are global ones, based of information from all available sources, and expressed on a three-point scale: absent, O; dubious or minimal; 1; and definitely present, 2. There are 50 items grouped into 8 categories: emotions, somatic, social relationships, speech and language, motor, habitual manipulations, conduct and miscellaneous.
(3)A child-behabviour questionnaire (Rutter Scale A) to be completed by parents if the child is 6 years old or above (Rutter, 1970). There are 31 items, symptoms are scored on a 3-point scale and children scoring 13 or more are regarded as problem cases. This scale has been used in clinic studies and its reliability and validity has been well documented. A Chinese version was used. Several forward and backward translations were carried out in order to achieve accurate translation.
RESULTS
69 children were seem during the above mentioned period. The mean age was 8 years 2 months (S.D.: 29 months). There were 46 boys and 23 girls.
SOURCE OF REFERRAL
The majority (N = 56, 81.2%) was self-referred. 12 (17.4%) were referred by social worker of St. James' Settlement and one by teacher.
REASON OF REFERRAL
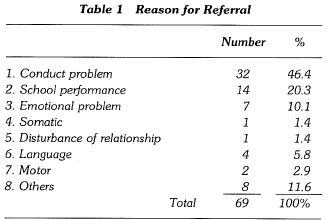
It was shown in Table 1. Conduct problem and school performance problem formed the majority.
DURATION OF PROBLEM
In 46 (66.6%) of them, the duration of child's psychiatric disorder was 2 years or more.
DEMOGRAPHIC DATA
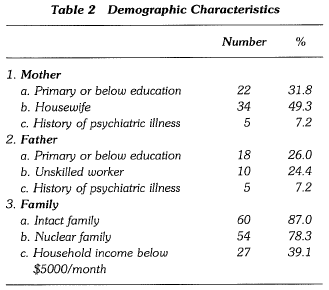
Mean age of mother was 35 years (S.D. 4 years 6 months). The mean number of siblings was 2.07. The other family characteristic was shown in Table 2.
DIAGNOSIS
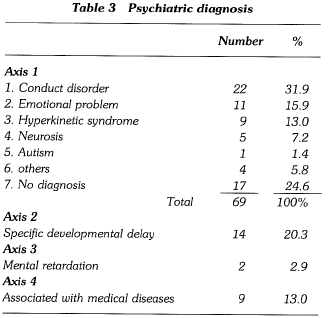
Psychiatric diagnosis was made according to a multi-axial classification scheme developed within the W.H.O. programme on the standardization of diagnosis, classification and statistics (Rutter, 1975). See Table 3. The three main diagnosis were conduct disorder, emotional disorder and hyperkinetic syndrome. Out of the 17 children with no Axis one diagnosis, 5 suffered from specific developmental delay and one mental retardation.
SYMPTOM PATTERN
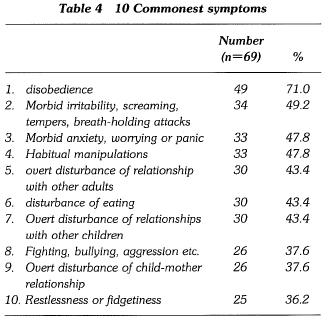
The mean number of symptoms recorded in the symptom-check-list was 5.35 (S.D. 2.69). The 10 commonest symptoms were shown in Table 4. Disobedience was the commonest symptom.
RUITER A QUESTIONNAIRE
There were 56 children above 6 years old. The mean score was 20.32 (S.D. 6.81)
DISCUSSION
In the beginning, we were unsure about the nature of the problem that would tum up in the clinic. Because it was not screened, the cases might turn out to be mild cases or transient problem. In effect, we found that the majority of cases seen in the Child Mental Health Clinic was suffering from a definable psychiatric disease which required psychiatric intervention. They should not be regarded as mild cases. On the contrary, these cases should be considered seriously because: (1) The duration of child's psychiatric disorder was over 2 years in 66.6% of the sample; (2) the mean Rutter A Questionnaire was 20.32. Although there was no local norms, the mean score was very much higher than the usual cut off point ( > 13) to define abnormality (Rutter 1970); (3) the mean number of symptoms in the _symptom check list was 5.35, showing the usual picture of multiple symptoms in a patient.
The comparison between the characteristics of children in our sample with the other two similar studies in Hong Kong is important (Luk & Lieh-Mak 1985; Wong 1988). The Child Mental Health Clinic can be considered as a primary care clinic because self-referral was accepted, it was different from the other 2 clinics which accepted mainly referrals from doctors. Comparison between these 2 settings will give idea on the reason why cases are referred to specialist services.
It was difficult to compare the characteristics of our sample with the other two similar studies in Hong Kong because (1) our children sample was younger; (2) detail demographic data was not mentioned in the other 2 studies. Anyway, 2 interesting features were noted:
(1) The 2 most common reasons for referral in our sample were conduct problem and unsatisfactory school performance. In the 2 previous studies conduct problem was also common but not unsatisfactory school performance. On the other hand, somatic complaints were more common in their samThis finding suggested referral bias.
(2) The frequency of the common childhood problems of conduct disorder, emotional problem and hyperkinetic syndrome were similar in all 3 There was only one case of childhood autism and no psychophysiological disorder in our sample. Childhood autism was over-represented in Luk & Lieh-Mak's sample and also not uncommon in Wong's sample probably because cases of autism were usually referred to Special Centre for management (Kaeser, 1971).
CONCLUSION
Our study supported the finding ·that a lot of child psychiatric cases were not referred to specialist services (Rutter, 1970). As the duration of the children's psychiatric problems was over 2 years in the majority of our sample, it meant that some of them might never reach specialist service if not for the presence of the self-referred child mental health clinic. Williams and Clare (1981) have identified 3 models in which psychiatrists and general practitioners can collaborate in the provision of care for this pool of psychiatric patients. They are: (1) "replacement model", the psychiatrists replace the general practitioner as the doctor of first contact. (2) "increased throughput" model is based on the view that more patients should be referred to psychiatists. (3) "liaison-attachment" model whereby psychiatrists move out of hospital into the general practice setting itself. Our self-referred child mental health clinic probably belong to their "replacement model,". In Hong Kong, this model of service may be of importance because:
(1) the primary care structure is not well established in Hong Referral to specialists depend very much on whether patient can find a doctor who shows interest in child psychiatric problem;
(2) parents may be reluctant to attend psychiatric clinic because of stigma. The Child Mental Health Clinic provides a useful
ACKNOWLEDGEMENT
The authors wish to thank all the staffs of St. James' Settlement who co-operated in this study.
REFERENCES
Kaeser, A.C. & Cooper, B. (1971) The psychiatric out-patient, the general practitioner and the outpatient clinic; an operational study: a review. Psychological Medicine, I, 312-325.
Luk, S.L. & Lieh-Mak, F. (1985) Journal of Paediatrics, Obstetrics and Gynaecology, Sept/Oct, 15-18.
Rutter, M., Tizared, J. & Whitmore, K. (1970) Education Health & Behaviour, London: Longman.
Rutter, M., Shaffer, D., Sturge, C. (1975) A guide to a multi-axial classification scheme for psychiatric disorders in childhood and adolescence. Institute of Psychiatry, London.
Thorley (1982) The Bethlem, Royal and Maudsley Hospital's clinical data register for children and adolescents. Journal of Adolescence, 5, 179-189.
William, P, Clare, A.W. (1981) Changing patterns of psychiatric care. British Medical Journal, 282, 375-377.
Wong, C.K. (1988) Journal of the Hong Kong Medical Associa tion, 40, 1, 40-49.
World Health Organization (1973) Psychiatry and Primary Medical Care. Copenhagen: WHO.
Y. Chung, MB, BS; MRCPsych Senior Lecturer, Department of Psychiatry, University of Hong Kong.
S.L. Luk, MB, BS, MRCPsych Senior Lecturer, Department of Psychological Medicine, University of Otago, New Zealand.
Soo BA, BSW Division Supervisor, St. James' Settlement.
Correspondence: Department of Psychiatry, University of Hong Kong, Queen Mary Hospital, Hong