Hong Kong J Psychiatry 2004;14(3):26-30
ORIGINAL ARTICLE
Dr Soumya Basu, MD, DPM, Central Institute of Psychiatry, Kanke, Ranchi, Jharkhand, India-834006.
Professor Vinod K Sinha, MD, DPM, Central Institute of Psychiatry, Kanke, Ranchi, Jharkhand, India-834006.
Address for correspondence: Dr Vinod K Sinha, Central Institute of Psychiatry, Kanke, Ranchi, Jharkhand, India-834006.
Submitted: 6 November 2002; Accepted: 30 October 2003
Abstract
Objective:This study was conducted to find the average duration of prodrome in childhood and adolescent mania, to ascertain the symptoms, and to assess the difference in duration of prodromes on the basis of sex, mood, and age.
Patients and Methods:This was a prospective study of 30 consecutive patients aged 19 years or younger who had had a manic episode or bipolar affective disorder, manic type according to the International Classification of Diseases-10. A checklist was applied for symptoms of mania and other associated symptoms. The duration between the first symptom and the manic episode was taken as the prodrome.
Results:The mean duration of prodrome was 14.9 days. A significantly longer prodromal period was found for the age group 12 to 16 years than for the age group 17 to 19 years (mean, 22.9 days vs 7.9 days). Decreased sleep and increased self-esteem were among the most common prodromal symptoms.
Conclusions:Caregivers can be sensitised to early warning symptoms so that treatment can be initiated early to prevent a full-blown manic episode and/or admission to hospital, thereby influencing the course and prognosis of the manic episode.
Key words: Adolescent, Bipolar disorder, Child
Introduction
The term prodrome indicates a forerunner of an event.1 In other words, a prodrome is the period that elapses between the occurrence of the first symptoms and the fully developed illness. The appearance of prodromal symptoms has been important in clinical medicine for many progressive and treat-able diseases in which early detection and timely treatment are crucial. Except for schizophrenia, research into prodro-mal symptoms in psychiatry has been largely anecdotal.1-5
Recent studies have concentrated on identifying symp-toms of mania early in the evolution of the episode.6-8 Social workers have been encouraged to detect early relapses and refer such patients to minimise the undesirable con-sequences of career damage, financial loss, unwanted pregnancy, and impaired relationships.9
In one study, 40 adult patients with mania and de-pression were interviewed on the prodromes for mania and depression and how these prodromes were managed.10 The authors reported that, for patients with bipolar disorder, their level of functioning in the areas of work, marital relation-ships, parenting abilities, and social functioning was related to how well they managed the prodromes of mania. The recognition of prodromal symptoms is becoming more important, as highlighted by the emergence of psychoeduca-tional programmes for partners of patients with bipolar mania.11 The National Institute of Mental Health working parties highlighted the need for research and the develop-ment of methods for psychological intervention in bipolar affective disorder,12,13 an obvious candidate being early intervention during the prodrome.
Several methodological problems are involved in the exploration of prodromes in affective disorders.1,2 Studies have equated hospital latency — the time of onset of the first symptom to the point of admission to hospital — as that of evolution or prodrome.14,15 In 1988, Molnar et al defined prodrome as the period from onset of the first symptom to maximum intensity — a definition that is consistent with the concept of evolution.6 Meanwhile Keitner et al asked the pa-tients and guardians to list the symptoms before the onset of the manic episode — a concept consistent with prodrome.8
There have been many methods of eliciting symptoms during evolution. Studies have asked the patients to re-port symptoms of prior episodes6,8 or have used a symptom checklist.7 Other methods include dating the symptoms using the Present State Examination15 and longitudinal Brief Psychiatric Rating Scale administration.16 Use of a symp-tom checklist might facilitate recall by the informant but would result in missed symptoms not included in the checklist. Asking the informants to recall the symptoms would result in some symptoms being missed due to the time delay. Further, many data would be generated making it difficult to sort into categories. A better design would be to use a symptom checklist to facilitate recall along with an open column for unlisted symptoms.
Another methodological issue comprises the source of the information. Previous researchers have interviewed pa-tients and/or corroborated the information with the relatives’ help.6-8,15 Although it has been reported that patients retain insight after the onset of illness,7 other researchers have noted that insight is lost from the earliest symptoms.9 Insight, if present, is transient and patients with mania are notoriously refractory to self-examination and treatment.17 Thus, even if a patient is able to recollect episodes, it becomes incum-bent on the caregivers to identify an impending relapse and to help patients seek treatment.
The use of prophylactic drugs could affect the develop-ment of an episode of mania and this aspect is not men-tioned in most studies.6-8 While many patients are receiving drugs,15,16 it is necessary for them to be drug-free for the index episode for which they are evaluated so that the assessment of prodrome is accurate. Other methodological problems include assessment strategies (prospective or retrospective) and confounding symptoms such as premorbid traits and subclinical fluctuations of mood in chronic affec-tive conditions such as bipolar disorder.5,10
The recommendation for indefinite, life-long treatment has been successfully challenged for schizophrenia18 and questioned by some authors for bipolar illness.19 Therefore, identification of prodromal symptoms early in the course of the illness may be useful for intermittent use of lithium,9 enabling recurrences of affective disorder to be treated earlier and perhaps more effectively. 6
Previous findings have indicated that mania can begin in very early childhood. Some parents have reported that symptoms of mania had always been present, but were un-able to establish an exact age of onset.20 This finding is con-sistent with the finding of insidious onset reported in early onset bipolar disorder21 and that it is sometimes preceded by minor oscillations in mood or mild cyclothymic mood swings.21
Early psychosis has often been equated with early schizophrenia. As a consequence, first-episode (FE) affec-tive psychosis has been relatively neglected. Mania, in particular, has been understudied, and information in the literature about FE mania is sparse. For many reasons, it is important that a preventive approach should be extended to the full range of FE psychosis.22
This study was conducted to find the average duration of prodrome in childhood and adolescent mania, to ascer-tain the symptoms, and to assess the difference in duration of prodromes on the basis of sex, mood, and age, so that preventive methods may be used for future episodes.
Patients and Methods
This study was conducted at the Central Institute of Psychiatry, Ranchi, India. The Central Institute of Psychia-try is a postgraduate teaching hospital with a wide catch-ment area from eastern India and neighbouring countries such as Nepal, Bhutan, and Bangladesh, and has a 15-bed child psychiatry unit.
This prospective study enrolled 30 consecutive patients over a period of 7 months. The patients were aged 19 years or younger and fulfilled the Diagnostic Criteria for Research International Classification of Diseases-10 (DCR, ICD-10) for manic episode or bipolar affective disorder, manic type. Informed consent to participate in the study was obtained from the nearest relative.
Exclusion criteria included duration of prodrome greater than 6 months (as subjective recall is doubtful beyond that period), failure to obtain informed consent, accompanying relative not remaining with the patient for the index episode and diagnosis of organic mania or substance-induced mania. The patient was required to have been drug-free for at least 6 months before the appearance of the first symptom and there should have been no history of treatment with psy-chotropic drugs for the index episode.
All patients enrolled in the study were interviewed within 48 hours of their first contact in the Outpatients Depart-ment and the severity of the index episode was rated using Young’s Mania Rating Scale.23 Relevant information such as demographic and socioeconomic details, history and family history of mental illness, and personal history was recorded. The symptom checklist was given to the relative, who was asked to record the symptoms. Later, relatives were asked to sequence the events in order of onset and date the individual symptoms as accurately as possible in the symptom checklist. This was a self-generated checklist (available from the first author) that was prepared in con-sultation with faculty members and other senior practicing psychiatrists. The checklist incorporated the features of the symptom checklist of the Diagnostic and Statistical Manual of Mental Disorders-IIIR (DSM-IIIR), the des-cription of manic episode in the DSM-IV, and symptoms of manic episode in the DCR, ICD-10. This checklist was used by another group from the Central Institute of Psychiatry to study the pattern of evolution of symptoms during manic episodes.24 The section ‘other’ in the list was left for uncommon/unlisted symptoms, thereby making the questionnaire flexible and open.
The duration between the first symptom and the day on which criteria for manic episode (bipolar affective disorder, current episode mania) were fulfilled was taken as the prodrome, which included symptoms other than those required for diagnostic criteria (e.g., hedonic symptoms such as increased or decreased appetite, increased energy, and depressive symptoms such as fatiguability, suicidal ideas, and low mood). It was hypothesised that a significant prodro-malperiod would emerge from this study in adolescent mania with some symptoms common to prodrome in all patients.
Results
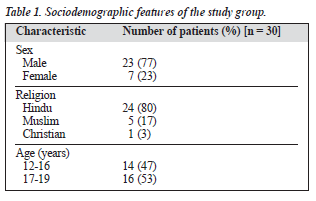
The details of the sociodemographic characteristics are shown in Table 1. The relative was the father for 22 patients, brother for 4, and mother for 4. The mean duration of pro-drome was 14.9 ± 18.3 days (range, 3.0 - 65.0 days). Twenty two patients (73.3%) had a prodrome with a mean of 20.3 ± 18.6 days. Twenty one patients did not have any history of psychiatric illness, while 9 patients had previous affective episodes (mean, 1.7 episodes; range, 1 - 5 episodes; median, 1 episode). Eighteen of the 21 FE patients (85.7%) had a prodrome with a mean of 22.80 days and 4 of the 9 patients with a previous history of affective episode (49.4%) had a prodrome with a mean of 29.75 days. The mean and standard deviations of the prodrome for the vari-ous subcategories are shown in Table 2. A significantly longer prodromal period was found for the age group 12 to 16 years than for the age group 17 to 19 years (mean, 22.9 days vs 7.9 days).
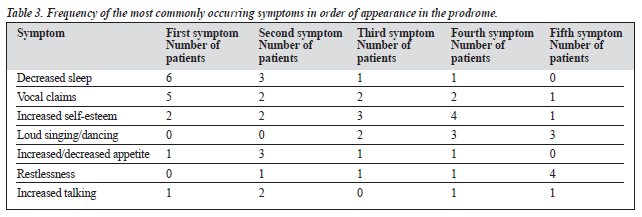
A significant difference by sex was found in Chi-squared analyses (likelihood ratio = 0.02). All 7 females (100%) had predominantly irritable mood, whereas 15 of 23 males (65%) had irritable mood. Table 3 shows the most commonly occurring symptoms in order of appearance in the prodrome (according to the symptom check list).
The most frequent first symptom occurring in prodrome was decreased sleep (27%), followed by vocal claims (23%). Of the first 3 frequent symptoms, decreased sleep was the most frequent (45%), followed by vocal claims (41%) and increased self-esteem (32%). Of the first 5 symptoms, vocal claims and increased self-esteem were equally frequent (54%), followed by decreased sleep (50%) and loud singing/ dancing (36%).
Discussion
The target of this study was the duration and pattern of pro-dromal symptoms in childhood and adolescent mania. Acute or abrupt onset have been described but the exact duration has remained elusive until, in 1 study, a time frame of 1 to 10 days was noted.25 A more precise duration of 21.14 ± 22.24 days was given in another study.6 However, in other studies, it was concluded that prodromal symptoms might precede the full syndrome by weeks or months (median, 22.00 days).7,15
This study showed that 73% of the population reported prodromal symptoms, which is similar to 75% reported by Smith and Tarrier,7 but less than 93% reported by Keitner et al.8 The findings of this study are in contrast to the findings of previous studies,20-21 which inferred that the onset of ju-venile mania might be insidious, manifesting itself in some children at the beginning of life. One of the major differ-ences could be that in the group described here, all patients were aged between 12 and 19 years, whereas earlier studies enrolled younger patients. In this study, prodrome was sig-nificantly longer (mean, 22.9 days) in the younger age group than in the older age group (mean, 7.9 days). As 12 of the 14 children in the younger age group had FE mania, the prodromal period in 85.7% of this group gave the clinicians an opportunity to educate the relatives about common pro-dromal symptoms so that early intervention for future manic prodrome could be instigated.
Another reason for the shorter duration of prodrome in this study may be the use of the stringent DCR, ICD-10 criteria to demarcate prodrome from onset of the manic episode, which were not used in any of the previous studies, whereby the demarcating feature was either admission to hospital or left to the patient’s or relative’s discretion). As shown in earlier studies,26 a significant proportion of pa-tients (73%) had predominantly irritable mood and only 8 of 30 patients (27%) had elevated mood. A significantly high prevalence of irritable mania in females (7 of 7) compared with males (15 of 23) was also noted.
Jacobson, while describing the signs, stressed the fact that each individual may have different symptoms thus emphasising the heterogeneity of symptoms in a prodromal phase.9 However, other studies found certain symptoms that were consistent in all patients.6,7,9,27,28 These symptoms in-cluded decreased sleep, increased activity, increased socialisation, and elevated mood. In 1987, Wehr et al hypothesised that sleep disturbance was the final common pathway leading to a manic episode.29
In this study, decreased sleep, vocal claims, and increased self-esteem were frequently found among the first 5 symptoms. An interesting clinical feature of many patients with mania in this study was the ease with which they com-plied with the request to sing a song. Singing was thus as-sessed as a prodromal symptom and was found in 36% of the population when the most common first 5 symptoms were considered together. Interestingly, elevated/irritable mood never predominated the prodrome, although the acu-men needed by the relatives to detect this might be ques-tionable in this sociocultural group.
This clinical study of prodromal symptoms in childhood and adolescent mania was exploratory in nature and was thought necessary owing to the absence of any comprehen-sive published work from India and limited international research. Seventy three percent of the study population (22 of 30 patients) were found to have a mean prodromal phase of 20.3 days. Decreased sleep, vocal claims, increased self-esteem, and loudly singing songs/dancing were the most common initial prodromal symptoms, which contrasts with the elated mood and increased activity reported in previous studies of adult populations. The difference could be either due to the difference in age of the patients or to cultural differences. This study had the advantage of assessing the prodromal phase in detail via a symptom checklist with specific relevance to an Indian setting.
Some limitations of this study include the small sample size, the non-standardised symptom checklist, which was more closed than open, the lack of a control group for drug treatment or any other form of treatment, and the lack of patients younger than 12 years. Again, unless prodromes are similar in duration and pattern across episodes, it would be difficult for the family or treating personnel to draw conclusions, hence the need to compare the initial date with that of follow-up and readmissions, thus requiring a prospective detection of manic prodromes rather than the approach used in this study.
The strength and uniqueness of this study lies in the fact that prodrome was demarcated when DCR, ICD-10 criteria for manic episode were fulfilled, thus making it more objective and definitive rather than arbitrary and subject to patients’ or relatives’ discretion. With these findings, pa-tients and their relatives can be sensitised to the early warning symptoms so that treatment can be initiated early to prevent a full-blown manic episode and/or admission to hospital, thereby influencing the course and prognosis of the manic episode.
References
- Chapman J. The early symptoms of schizophrenia. Br J Psychiatry 1966; 112:225-251.
- Docherty JP, Van-Kamnen DP, Siris SG. Stages of onset of schizo-phrenic psychosis. Am J Psychiatry 1978;135:420-426.
- Herz MI, Melville C. Relapse in schizophrenia. Am J Psychiatry 1980; 137:801-805.
- Birchwood M, Smith J, Macmillan F. Predicting relapse in schizophrenia. Psychol Med 1989;19:649-656.
- Subotnik KL, Nuechterlein KH. Prodromal signs and symptoms of schizophrenic relapse. J Abnorm Psychol 1988;97:405-412.
- Molnar G, Feeny MG, Fava GA. Duration and symptoms of bipolar prodromes. Am J Psychiatry 1988;145:1576-1578.
- Smith JA, Tarrier N. Prodromal symptoms in manic-depressive psychosis. Soc Psychiatry Psychiatr Epidemiol 1992;27:245-248.
- Keitner GI, Solomon DA, Ryan CE, et al. Prodromal and residual symp-toms in bipolar I disorder. Compr Psychiatry 1996;37:362-367.
- Jacobson JE. The hypomanic alert: a program designed for greater thera-peutic control. Am J Psychiatry 1965;122:295-299.
- Lam D, Wong G. Prodrome, coping strategies, insight and social functioning in bipolar affective disorders. Psychol Med 1997;27: 1091-1100.
- Van-Gent EM, Zwart FM. Psychoeducation of partners of bipolar manic patients. J Affect Disord 1991;21:15-18.
- Prien RF, Potter WZ. NIMH Workshop report on treatment of bipolar disorders. Psychopharmacol Bull 1990;28:409-427.
- Scott, J. Psychotherapy for bipolar disorders. Br J Psychiatry 1995; 167:581-588.
- Francis A, Gasparo P. Interval between symptom onset and hospital-ization in mania. J Affect Disord 1994;31:179-185.
- Sclare P, Creed F. Life events and the onset of mania. Br J Psychiatry 1990;156:508-514.
- Altman ES, Margaret MR, Mintz J, Miklowitz DJ, Goldstein MJ, Hwang S. Prodromal symptoms and signs of bipolar relapse; a report based on prospectively collected data. Psychiatr Res 1992:41;1-8.
- Akiskal HA. Mood disorders: clinical feature In: Sadock BJ, Sadock, VA, editors. Comprehensive text book of psychiatry. 7th ed. Baltimore: Williams and Wilkins; 2000:1338-1376.
- Herz MI. Toward an integrated approach to the treatment of schizophrenia. Psychother Psychosom 1986;46:45-57.
- Molnar G, Fava GA. Long term follow up of patients on managed lithium discontinuation. Psychopharmacol Bull 1989;25:250-252.
- Wozniak J, Biederman J, Keily K. Mania like symptoms suggestive of childhood onset bipolar disorder in clinically referred children. J Am Acad Child Adolesc Psychiatry 1995;34:867-876.
- Akiskal HS, Downs J, Jordan P.Affective disorder in referred children and younger siblings of manic-depressives. Arch Gen Psychiatry 1985; 42:996-1004.
- Conus P, Mc Gorry PD. First episode mania: a neglected priority for early intervention. Aust NZ J Psychiatry 2002;36:158-172.
- Young RC, Biggsn JT, Ziegler VE, Meyer DA. A rating scale for mania: reliability, validity and sensitivity. Br J Psychiary 1978;133:429-435.
- Kumar R, Ram D. Evolution of symptoms of mania. Indian J Psychiatry 2001;43:235-241.
- Bunney WE, Murphy DL, Goodwin FK. The switch process in manic depressive illness. Arch Gen Psychiatry 1972;27:295-317.
- Hsu LK, Starzynski JM. Mania in adolescence. J Clin Psychiatry 1986; 47:596-599.
- Carlson GA, Goodwin FK. The stages of mania. Arch Gen Psychiatry 1973;28:221-228.
- Wong G, Lam D. The development and validation of the coping inven-tory for prodromes of mania. J Affect Disord 1999;53:57-65.
- Wehr TA, Sack DA, Rosenthal NE. Sleep reduction as a final common pathway in the genesis of mania. Am J Psychiatry 1987:144;201-204.