East Asian Arch Psychiatry 2015;25:128-136
ORIGINAL ARTICLE
Dr Ka-Yee Tung, MBBS, FHKCPsych, FHKAM (Psychiatry), Kwai Chung Hospital, Hong Kong SAR, China.
Dr Kin-Shing Cheng, MBChB, MRCPsych, FHKCPsych, FHKAM (Psychiatry), Kwai Chung Hospital, Hong Kong SAR, China.
Dr Wing-King Lee, MBChB, FRCPsych, FHKCPsych, FHKAM (Psychiatry), Kwai Chung Hospital, Hong Kong SAR, China.
Dr Po-Keung Kwong, MBBS, FRCPsych, FHKCPsych, FHKAM (Psychiatry), Kwai Chung Hospital, Hong Kong SAR, China.
Dr Kin-Wah Chan, MBBS, MRCP, FRCP (Edin), FHKCP, FHKAM (Medicine), Medical and Geriatrics Department, Princess Margaret Hospital, Hong Kong SAR, China.
Dr Alexander Chun-Bon Law, MBBS, FRCP (Lond, Glasg, Edin); FHKAM (Medicine), Medical and Geriatrics Department, Princess Margaret Hospital, Hong Kong SAR, China.
Dr William Tak-Lam Lo, MBBS, FRCPsych, FHKCPsych, FHKAM (Psychiatry), Kwai Chung Hospital, Hong Kong, SAR, China.
Address for correspondence: Dr Ka-Yee Tung, Kwai Chung Hospital, 3-15 Kwai Chung Hospital Road, Kwai Chung, New Territories, Hong Kong SAR, China.
Tel: (852) 2990 3000; Fax: (852) 2959 8702; Email: tky028a@ha.org.hk
Submitted: 11 February 2015; Accepted: 29 April 2015
Abstract
Objectives: To determine the prevalence of psychiatric morbidity and identify the correlates, as well as to evaluate the effectiveness of the Hospital Anxiety and Depression Scale and the 12-item General Health Questionnaire to screen for psychiatric morbidity in Chinese adults with type 1 diabetes.
Methods: Subjects were recruited from a local public diabetes specialist outpatient clinic from August 2013 to January 2014. Demographic and clinical factors were recorded. Psychiatric diagnosis was established using the Chinese-bilingual version of the Structured Clinical Interview for the DSM-IV Axis I disorders. Scores for the Hospital Anxiety and Depression Scale and the 12-item General Health Questionnaire were compared with the psychiatric diagnosis.
Results: Of the 136 patients, the point prevalence of overall psychiatric, depressive, and anxiety disorders was 39.7%, 23.5%, and 25.7%, respectively. Family history of mental illness, smoking status, history of mental illness, presence of social problems, perceived absence of confidant, presence of neuropathy and hyperlipidaemia, as well as higher level of glycosylated haemoglobin were found to be the associated factors.
Conclusion: Psychiatric disorders were common in Chinese adults with type 1 diabetes. Finding out associated factors and using the Hospital Anxiety and Depression Scale and the 12-item General Health Questionnaire as a screening tool helped to identify patients in a diabetes clinic with psychiatric disorders.
Key words: Diabetes mellitus, type 1; Mental disorders; Prevalence
Introduction
Type 1 diabetes (T1DM) is caused by beta-cell destruction in the pancreas, leading to absolute insulin deficiency. Unlike patients who suffer from type 2 diabetes (T2DM), individuals with T1DM present at a much younger age and depend on regular insulin injections for survival thereafter.1
They face a lifetime of inconvenience and restraints in order to achieve optimal glycaemic control. They need to juggle insulin dose, diet, and exercise to maintain a near-normal blood sugar concentration to reduce the threat of long- term complications while avoiding the short-term disaster of disabling hypoglycaemia. Previous studies have shown that patients with T1DM experience greater levels of threat than those with T2DM2: it is difficult for an individual with T1DM to live a normal life, and therefore not surprising to find that the rates of depression and anxiety are higher in those with T1DM than in healthy individuals.3-5
Psychiatric morbidities have long been proven to worsen glycaemic control,6-8 resulting in higher complication rates,9 decreased adherence to treatment regimen, and poorer quality of life.10,11 The early identification of treatable psychiatric morbidity is therefore of paramount importance and can greatly improve clinical outcomes.12,13
Psychiatric morbidity is common in T1DM patients, and it is being intensively investigated in many countries, but few data are available from Asia and Hong Kong. The current study aimed to assess the prevalence of psychiatric morbidity in T1DM patients in Hong Kong, to identify associated factors, and to assess the usefulness of convenient self-rating screening tools in assisting physicians to identify patients who are in need of referral to psychiatric services.
Methods
Study Design
This was a cross-sectional study conducted in a diabetes specialist outpatient clinic at the Princess Margaret Hospital of the Hospital Authority in Hong Kong from August 2013 to January 2014. The clinic acts as a major local centre for the management of all T1DM patients and those with T2DM who require intensive care because their diabetes is not under control despite treatment supervised by general medical clinics. Approval for the present study was obtained from the hospital’s Clinical Research Ethics Committee.
Patients
All patients who attended the diabetes clinic from August 2013 to January 2014 with a confirmed diagnosis of T1DM made by an endocrinologist were recruited to the study. According to the prevalence rate of depression found in a previous study,3 125 patients were needed for the current study. Patients were excluded if they were non- Chinese, unable to comprehend the Chinese language, or had significant cognitive impairment or communication difficulties.
Procedure
All eligible patients were approached by the first author in person on the day of their follow-up, and written informed consent was obtained from those who agreed to participate. They were given the Chinese version of the Hospital Anxiety and Depression Scale (HADS) and the Chinese version of the 12-item General Health Questionnaire (GHQ- 12) to complete before the interview. Characteristics of patients such as socio-demographic and clinical data were collected by the first author. The Chinese-bilingual version of the Structured Clinical Interview for the DSM-IV Axis I disorder (SCID) was administered by the first author who completed the required training in its use.
Data Analyses
The data from the present study were analysed using the Statistical Package for the Social Sciences Windows version 20.0 (SPSS Inc., Chicago [IL], US). Statistical analyses were performed in 2 stages. In the first stage, the variables were compared between: (1) T1DM patients with and without current psychiatric morbidity, (2) T1DM patients with and without current depressive disorders, and (3) T1DM patients with and without current anxiety disorders.
Two independent samples were compared using the Student’s t test for continuous variables that were normally distributed, and the Mann-Whitney U test was used for ordinal or non-normally distributed continuous data. The Chi-square test was used for categorical data comparison. When any of the cells for comparison had a value of < 5, the Fisher’s exact test was used. In the second stage, those variables with significant association (p < 0.1) from the bivariate analysis were entered into logistic regression to determine significant associations with psychiatric morbidity, depressive disorders, and anxiety disorders. The adjusted odds ratio (OR) and 95% confidence interval were calculated. All tests for statistical significance were set at p = 0.05. The receiver operating characteristic curve was used to evaluate the performance of HADS and GHQ-12 against the gold standard for diagnoses using SCID.
Results
Recruitment of Patients
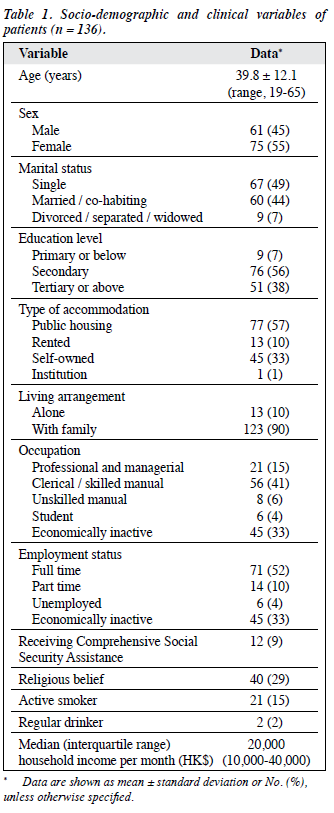
Among the 144 T1DM patients scheduled for follow-up at the diabetes clinic, 3 were excluded because they were unable to comprehend Chinese, and a further 3 were excluded because they had communication difficulties. Among the remaining 138 patients, 2 refused to participate. Thus a total of 136 subjects were recruited, yielding a response rate of 98.6%. No statistically significant difference was found between the participating and non-participating patients in this study with regard to gender (p = 1.00) or age (p = 0.76). The socio-demographic variables of the patients are shown in Table 1.
Clinical Characteristics, Medical Co-morbidities, Social and Psychiatric Background of Patients
Among the 136 patients, the mean (± standard deviation) age of onset of T1DM was 24.1 ± 11.7 years (range, 2-55 years), the mean duration of illness was 15.6 ± 10.4 years (range, 1-52 years), and the mean dose of insulin was 0.85 ± 0.34 units/kg (range, 0.15-2.4 units/kg). The prevalence of diabetes complications was 24.3%: among those with complications, 36.4% had nephropathy, 21.2% had neuropathy, 84.8% had retinopathy, and 6.1% had macrovascular disease. In addition, 72 (52.9%) patients had a haemoglobin A1c (HbA1c) level of ≤ 8 mmol/L; most (86.0%) were prescribed intensive insulin treatment and 59.6% monitored their blood glucose according to standards set by physicians (at least 3 times/day for 3 times/ week). Also, 77.2% had hypoglycaemic attacks < 5 times per month, 95.6% adhered to their insulin regimen, and 73.5% complied with dietary advice. The body mass index was < 23 kg/m2 in 49.3%, 23 to 25.9 kg/m2 in 25%, and ≥ 26 kg/m2 in 25.7% of the patients.
A total of 68 (50%) patients had chronic medical illnesses other than T1DM, and the most common co- morbidities were hyperlipidaemia (20.6%) and hypertension (17.6%). Among the recruited patients, 18 (13.2%) reported a history of psychiatric illness: 14 (10.3%) with depressive disorders, 2 (1.5%) with psychotic disorders, 1 (1%) with obsessive-compulsive disorder, and 1 (1%) with adjustment disorders. Current treatment for mental illness was prescribed to 16 (11.8%) patients. A reported family history of mental illness was present in 10 (7.4%) patients, and 60% of whom had a maternal history of depressive disorders. Also, 43 (31.6%) patients reported having problems in at least 1 social aspect, namely financial (15.4%), occupational (14.7%), family relationship (10.3%), and housing (8.1%) problems. Most (78.7%) patients had confidants with whom they could share their distress.
Prevalence of Psychiatric Morbidity
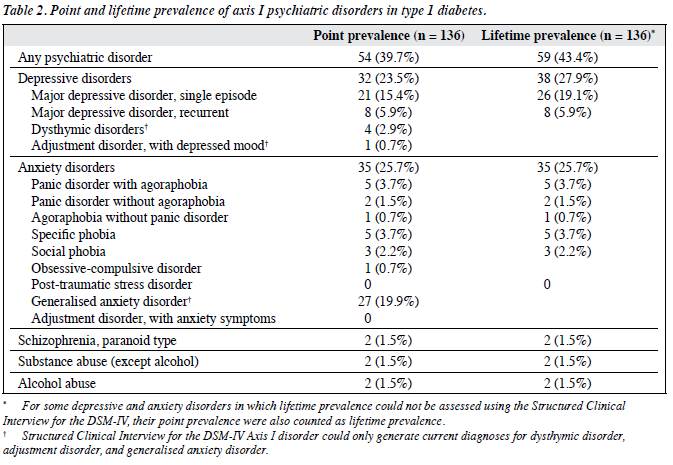
The point and lifetime prevalence of psychiatric morbidity are summarised in Table 2. The point prevalence of psychiatric disorders was 39.7%: that of depressive disorders was 23.5% and that of anxiety disorders was 25.7%. Major depressive disorder (MDD) was the most common depressive disorder and generalised anxiety disorder (GAD) was the most common anxiety disorder. Schizophrenia, substance abuse, and alcohol abuse were found in 2 (1.5%) patients each.
The lifetime prevalence of psychiatric disorder was 43.4%: that of depressive disorders was 27.9%, with MDD being the main contributor, and that of anxiety disorders was 25.7%. Generalised anxiety disorder had a point prevalence of 19.9%, which was greater than the lifetime prevalence of all of the other individual anxiety disorders; thus it was regarded as the most common lifetime anxiety disorder.
Correlates of Psychiatric Morbidities
Bivariate Analysis
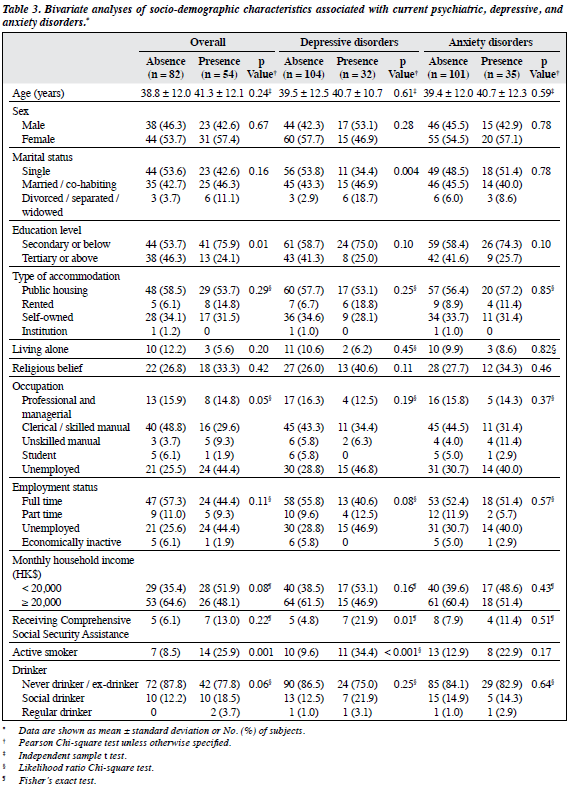
Socio-demographic comparison between the patients with current psychiatric, depressive and anxiety disorders and those without as diagnosed by SCID are summarised in Table 3. Patients with current psychiatric disorders were significantly more likely to have a lower level of education, be unemployed, and a smoker. The presence of other chronic medical illnesses in the genitourinary and orthopaedic systems, hyperlipidaemia and neuropathy, as well as the frequency of self-monitoring of blood glucose were significantly associated with psychiatric disorder. A psychiatric history and family history of mental illness were more common in patients with psychiatric disorders, who were also more likely to have social problems and perceived absence of confidant.
Patients with current depressive disorders were more commonly divorced, separated or widowed, in receipt of Comprehensive Social Security Assistance, and be a current active smoker. The level of HbA1c also differed significantly in depressed subjects. They were more likely to have a history of psychiatric illness and family history of mental illness, to have more social problems, and perceived absence of confidant.
Family history of mental illness, family and housing problems, and a perceived absence of confidant were significantly associated with current anxiety disorders. Most other socio-demographic characteristics, medical background, and characteristics of diabetes were not associated with anxiety disorder.
Multivariate Analysis
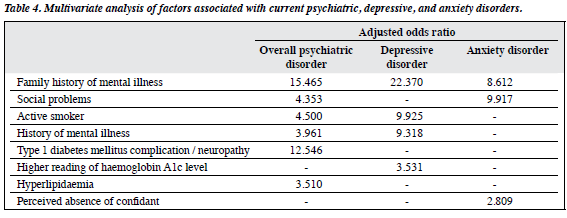
In the second stage of the statistical analysis, all potential predictors associated with a p < 0.1 on bivariate analysis were entered into the logistic regression. The results are summarised in Table 4.
Family history of mental illness and history of mental illness, the presence of neuropathy and hyperlipidaemia, being a smoker, and having social problems were shown to be independently associated with current overall psychiatric disorders. Family history of mental illness, history of mental illness, being an active smoker, and having a higher level of HbA1c were all independent factors associated with current depressive disorder. Family history of mental illness, perceived absence of confidant, and presence of family problems (a subtype of social problems) were independently associated with current anxiety disorders.
Performance of Hospital Anxiety and Depression Scale and 12-Item General Health Questionnaire
Comparison of sensitivity and specificity revealed that the GHQ-12 performed better than HADS in screening for current psychiatric, depressive, and anxiety disorders. For screening of current psychiatric disorders, the optimal cutoff point for GHQ-12 was 11/12 with a sensitivity of 81.5% and specificity of 65.9% (vs. 75.9% and 67.1% for HADS total score [i.e. combination of anxiety and depression subscale scores (HADS-T)] at an optimal cutoff point of 9/10). For current depressive disorders, the optimal cutoff point for GHQ-12 was 12/13 with a sensitivity of 71.9% and specificity of 70.2% (vs. 75.0% and 68.3% for HADS-T at an optimal cutoff point of 11/12). For current anxiety disorders, the optimal cutoff point for GHQ-12 was 12/13 with a sensitivity of 82.9% and specificity of 75.2% (vs. 74.3% and 65.3% for HADS-T at an optimal cutoff point of 10/11).
Discussion
Prevalence of Psychiatric Morbidity
Overall Psychiatric Disorders
The respective lifetime prevalence and point prevalence of psychiatric disorders was 43.4% and 39.7%, which is within the range reported by previous studies that used structured diagnostic interviews.8,10 The majority of patients (69.5%) in the study who had psychiatric disorders remained untreated — this is not an uncommon phenomenon as stated in the literature.14 Many factors contribute to this problem, including the common assumption that depression is merely secondary to the medical illness and not of independent importance, and it is therefore not the main focus of physicians.15
Prevalence of Depressive Disorders
The point prevalence of depression was 23.5%, with MDD (21.3%) being the most common diagnosis. These findings were comparable to those of a systematic review, with a range from 13.4% to 32% for uncontrolled studies.3 It also falls within the range of 8% to 36.6% for those studies that used structured interviews.15,16 In the present study, 21.3% of subjects suffered from MDD, which is higher than the 8.4% reported in a local study of the community population.17 This increase in the rate of depression may be due to the psychosocial demands and constraints imposed by diabetes,4 and the feeling of loss of control because of required lifestyle modifications.18 There is also evidence of a biological link between depression and diabetes19 that is bidirectional due to their many shared similarities.
Prevalence of Anxiety Disorders
The point prevalence of anxiety disorders was 25.7%, with GAD being the most prevalent at a rate of 19.9% and within the range of prevalence of anxiety disorders reported in the literature. The prevalence of GAD in our study was higher than that reported in a systematic review (14%),5 and may be explained by the large differences in methodology and diagnostic tools used in the 18 studies of the systematic review.
In the existing literature, much more focus has been placed on depressive disorders, but the present study showed a higher rate of anxiety disorder (25.7%) than that of depressive disorder (23.5%). The current study indicated that anxiety disorders are also common among T1DM patients and should receive more attention.
The prevalence of GAD (19.9%) in the present study was much higher than that reported in the local population (4.1%),20 and may be explained by the preoccupation of diabetic patients with self-monitoring, glycaemic control, and a fear of somatic complications, and hypoglycaemia,21,22 or occur secondary to hyperglycaemia.23
Factors Associated with Psychiatric Morbidity
Family History of Mental Illness
Family history of mental illness was a risk factor for current overall psychiatric, depressive and anxiety disorders, and the adjusted OR was particularly high for depressive disorders. A positive family history of depression was found to be more common in individuals with diabetics suffering from depression than in non- depressed subjects.24 Particular interest was given to the relationship between maternal mental illness and the development of depression in youths with T1DM. The present study also showed that the majority of subjects with a family history of mental illness had a maternal history of depression (60%). A 10-year longitudinal study showed that general maternal psychopathology was a risk factor for psychiatric disorders in youths, and that maternal depression specifically increased the risk of depression in offspring.25
Presence of Social Problems
The presence of social problems was an independent factor associated with current overall psychiatric and anxiety disorders. The presence of social stressors has long been known to be associated with psychiatric disorders, and their relationship is bidirectional. Psychiatric disorders can lead to lowering of work productivity, relationship difficulties, poor stress, and reduced ability to cope. These can lead to emergence of social stressors. Social stressors can also precipitate psychiatric disorders. Two studies reported that life events were strongly associated with common mental disorders, especially in mid-adult life.26,27 This corresponds with the mean age (39.8 ± 12.1 years) of our study subjects. This is further supported by a study conducted during the time of the breakup of Yugoslavia when economic and political deterioration increased, a much higher rate of psychiatric disorders in diabetic individuals was reported than in other studies.28
Smoker
Smoking status was an independent factor associated with current overall psychiatric and depressive disorders. One study indicated that smokers had significantly higher levels of perceived stress, negative affect, and had more depressive and general clinical symptoms than non-smokers.29 Smoking cessation was reported to be particularly difficult in this group of patients, because they may experience more severe depression and worse nicotine withdrawal symptoms.30 Smoking cessation can be helped with the use of antidepressants such as bupropion, together with close surveillance of the patient’s mental state by health care professionals.30
History of Mental Illness
History of mental illness was an independent factor associated with current overall psychiatric and depressive disorders. A history of mental illness is known to increase the risk of future psychiatric morbidities, such as MDD for which relapses and recurrence are well known to occur.31One study also showed that an earlier psychiatric disorder increased the risk of later disorder in subjects with T1DM.25
Neuropathy
The occurrence of neuropathy was a risk factor for current overall psychiatric disorders. Several studies have shown that diabetes complications are associated with an increased risk of psychiatric morbidities.16,32 Neuropathy can be episodic or chronic, intermittently or persistently painful, and quite frequently produces disability. It may also act as a stressor that is sufficient to provoke depression.33 Peripheral neuropathy is estimated to affect about 30% of patients with diabetes, and often coexists with depression with which it shares many common pathways34: the monoaminergic pathways, including the serotonergic and noradrenergic systems, and disturbances in the hypothalamic-pituitary- adrenal (HPA) axis occur, together with an increase in cytokines and down-regulation of negative feedback at glucocorticoid receptors in both chronic pain and depression.35 Patients with neuropathy also present with a more severe course of depression.33 Thus, it is important to target the treatment of both neuropathy and depression through their common pathways, such as the use of selective serotonin and noradrenaline reuptake inhibitors or tricyclic antidepressants that block both the reuptake of 5-hydroxytryptamine and noradrenaline.34
Haemoglobin A1c Level
The level of HbA1c was an independent factor associated with current depressive disorder. A meta- analysis confirmed the association of depression with hyperglycaemia, but revealed neither the mechanism nor the direction of the association.7 Both physiological and behavioural mechanisms have been hypothesised.6
Hormonal changes such as changes in the pituitary-adrenal cortical system through the effect of cortisol, the effects of epinephrine and norepinephrine on the sympathetic- adrenal medullary system, and increased glucagon and growth hormone secretion as a result of depression may all cause hyperglycaemia. Behavioural mechanisms also play an important role, because depressed individuals are less likely to adhere to strict diabetes self-care behaviour, resulting in poor glycaemic control.6 Hyperglycaemia is also shown to produce dysphoric symptoms and altered mood state.23 Another complex component is the effect of the pharmacological treatment of depression on glycaemic control. Serotonin reuptake inhibitors have been shown to decrease blood glucose levels,12 whereas tricyclic antidepressants have been reported to increase serum blood glucose level.13 The direction of the relationship between depression and glycaemic control thus remains unclear.
Hyperlipidaemia
Hyperlipidaemia was an independent factor associated with current overall psychiatric disorders. Previous studies found that physiological mechanisms link depression and metabolic syndrome, including the dysregulation of the HPA axis and the autonomic nervous system.36 Therefore, hyperlipidaemia, diabetes, and depression are frequently found to coexist. In another study, hyperlipidaemia was also shown to increase the risk of depression and anxiety and to exhibit a synergistic effect on the risk of depression in the presence of diabetes.37 It also reported that the use of statin was associated with a reduced risk of depression in hyperlipidaemic patients.37 Antidepressants or antipsychotics should also be used more cautiously to treat psychiatric morbidities, because they have been shown to increase the risk of hyperlipidaemia.36
Perceived Absence of Confidant
Perceived absence of confidant was an independent predictor of anxiety disorders. The presence of confidant was evaluated as a factor to reflect the level of perceived social support. As shown in other studies, poor social support is associated with an increased risk of psychiatric morbidities.38 Support may predispose individuals to perceive stressful situations and the adaptation to chronic illness as less threatening.2 The lifestyle changes that T1DM patients need to make may sometimes be difficult to implement and maintain, and social support thus plays an important role. A low level of social support was associated with high diabetes distress, low diabetes empowerment and poor quality of life, and less frequent healthy eating, exercise, and even adherence to medication.39
Clinical Implications
This study showed that psychiatric morbidities were high in the local T1DM population. The majority of those with psychiatric morbidity had been left untreated although treatment has been shown to have beneficial outcomes.40 Staff in diabetes clinics should therefore be more alert to the presence of psychiatric disorders, especially depression and anxiety disorders.
Some factors were identified as being associated with psychiatric morbidity and could help physicians to recognise those who are at risk and make referrals when necessary. Patients who are more vulnerable to psychiatric morbidity include smokers, those with a family history of mental illness, social problems, a history of mental illness, and perceived absence of confidant. Those with diabetic neuropathy, a high HbA1c level, and hyperlipidaemia should also receive more attention. Input from a medical social worker may be helpful for socially deprived patients. Health care professionals should promote the active involvement of family members in empowering patients to manage their diabetes. Education about mental health should also be provided to patients and families. Due to the bidirectional effect of psychiatric morbidities and glycaemic control, physicians should be more stringent in keeping HbA1c at an optimal level and pay special attention to the effect on glycaemic control when antidepressants are prescribed. Promoting smoking cessation and assisting the patient to quit smoking by the use of antidepressants such as bupropion may help. The occurrence of diabetic neuropathy should also receive prompt attention and the symptoms can be minimised by the use of duloxetine, with both serotonin and norepinephrine reuptake inhibitor properties.41 Statin should also be used to treat hyperlipidaemia, because it has been shown to lower the risk of depression.37
Given the detrimental effects of psychiatric disorders on outcomes, prompt identification is necessary. The 2 screening tools used in this study showed acceptable sensitivity and specificity. The HADS with a total score cutoff threshold of 9/10 and the “0123” scoring method of GHQ-12 with a cutoff threshold of 11/12 offer a practical means by which a physician can screen for psychiatric morbidity. The GHQ-12 showed better discriminatory power and should therefore be preferred to HADS. Patients who screen positive can be referred to the mental health professionals for further evaluation so that appropriate treatment can be offered.
Limitations and Directions for Future Research
Several limitations in the present study should be noted so that possible improvements can be made for future studies, if time and resources are adequate and logistic difficulties can be overcome.
This was a cross-sectional study and could not delineate the temporal relationship between independent factors and psychiatric disorders. A control group was not included for comparison of the prevalence of psychiatric disorders and their associated factors, and the results could only be compared with those of other studies.
The study relied heavily on the subjects’ self- reporting of current and past symptoms. Those who were afraid of being stigmatised or had poor insight might have withheld their symptoms, resulting in the under-reporting of psychiatric symptoms. Collateral information collected from significant others may help to correct this. The contribution of personality factors, help-seeking behaviour, and coping strategy were not assessed. Furthermore, only the self-perceived presence of social problems was used, not a subjective assessment by standard instruments. Nonetheless a lengthy assessment might reduce the willingness of patients to participate in the study. Future studies can focus more on those factors that were not assessed in this study and significantly associated ones can be examined in more detail.
Conclusion
The current study is the first to estimate the prevalence of psychiatric disorders among local Chinese adults with T1DM using a structured clinical interview. It suggested that current psychiatric morbidities are prevalent, with depressive and anxiety disorders being the most common.
This phenomenon is under-recognised, and many of these patients were not receiving proper mental health care. To facilitate early identification and referral for patients in need of psychiatric services, the use of GHQ, together with the other identified associated factors, can aid early detection of psychiatric morbidity and improve patient outcome.
Declaration
The authors declare that they have no source of financial support for the study.
References
- American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care 2014;37 Suppl 1:S81-90.
- Connell CM, Davis WK, Gallant MP, Sharpe PA. Impact of social support, social cognitive variables, and perceived threat on depression among adults with diabetes. Health Psychol 1994;13:263-73.
- Anderson RJ, Freedland KE, Clouse RE, Lustman PJ. The prevalence of comorbid depression in adults with diabetes: a meta-analysis. Diabetes Care 2001;24:1069-78.
- Gendelman N, Snell-Bergeon JK, McFann K, Kinney G, Paul Wadwa R, Bishop F, et al. Prevalence and correlates of depression in individuals with and without type 1 diabetes. Diabetes Care 2009;32:575-9.
- Grigsby AB, Anderson RJ, Freedland KE, Clouse RE, Lustman PJ. Prevalence of anxiety in adults with diabetes: a systematic review. J Psychosom Res 2002;53:1053-60.
- de Groot M, Jacobson AM, Samson JA, Welch G. Glycemic control and major depression in patients with type 1 and type 2 diabetes mellitus. J Psychosom Res 1999;46:425-35.
- Lustman PJ, Anderson RJ, Freedland KE, de Groot M, Carney RM, Clouse RE. Depression and poor glycemic control: a meta-analytic review of the literature. Diabetes Care 2000;23:934-42.
- Lustman PJ, Griffith LS, Clouse RE, Cryer PE. Psychiatric illness in diabetes mellitus. Relationship to symptoms and glucose control. J Nerv Ment Dis 1986;174:736-42.
- de Groot M, Anderson R, Freedland KE, Clouse RE, Lustman PJ. Association of depression and diabetes complications: a meta-analysis. Psychosom Med 2001;63:619-30.
- Das-Munshi J, Stewart R, Ismail K, Bebbington PE, Jenkins R, Prince MJ. Diabetes, common mental disorders, and disability: findings from the UK National Psychiatric Morbidity Survey. Psychosom Med 2007;69:543-50.
- Kohen D, Burgess AP, Catalán J, Lant A. The role of anxiety and depression in quality of life and symptom reporting in people with diabetes mellitus. Qual Life Res 1998;7:197-204.
- Lustman PJ, Freedland KE, Griffith LS, Clouse RE. Fluoxetine for depression in diabetes: a randomized double-blind placebo-controlled trial. Diabetes Care 2000;23:618-23.
- Lustman PJ, Griffith LS, Clouse RE, Freedland KE, Eisen SA, Rubin EH, et al. Effects of nortriptyline on depression and glycemic control in diabetes: results of a double-blind, placebo-controlled trial. Psychosom Med 1997;59:241-50.
- Rubin RR, Ciechanowski P, Egede LE, Lin EH, Lustman PJ. Recognizing and treating depression in patients with diabetes. Curr Diab Rep 2004;4:119-25.
- Lustman PJ, Clouse RE, Griffith LS, Carney RM, Freedland KE. Screening for depression in diabetes using the Beck Depression Inventory. Psychosom Med 1997;59:24-31.
- Pouwer F, Geelhoed-Duijvestijn PH, Tack CJ, Bazelmans E, Beekman AJ, Heine RJ, et al. Prevalence of comorbid depression is high in out- patients with type 1 or type 2 diabetes mellitus. Results from three out-patient clinics in the Netherlands. Diabet Med 2010;27:217-24.
- Lee S, Tsang A, Kwok K. Twelve-month prevalence, correlates, and treatment preference of adults with DSM-IV major depressive episode in Hong Kong. J Affect Disord 2007;98:129-36.
- Trigwell P, Peveler R. Psychiatric aspects of diabetes mellitus. Adv Psychiatric Treatment 1998;4:159-66.
- Heeramun-Aubeeluck A, Lu Z, Luo Y. Comorbidity of depression and diabetes: in a nutshell. Psychology 2012;3(Spec Issue):787-94.
- Lee S, Tsang A, Chui H, Kwok K, Cheung E. A community epidemiological survey of generalized anxiety disorder in Hong Kong. Community Ment Health J 2007;43:305-19.
- Friedman S, Vila G, Timsit J, Boitard C, Mouren-Simeoni MC. Anxiety and depressive disorders in an adult insulin-dependent diabetic mellitus (IDDM) population: relationships with glycaemic control and somatic complications. Eur Psychiatry 1998;13:295-302.
- Wild D, von Maltzahn R, Brohan E, Christensen T, Clauson P, Gonder- Frederick L. A critical review of the literature on fear of hypoglycemia in diabetes: Implications for diabetes management and patient education. Patient Educ Couns 2007;68:10-5.
- Sommerfield AJ, Deary IJ, Frier BM. Acute hyperglycemia alters mood state and impairs cognitive performance in people with type 2 diabetes. Diabetes Care 2004;27:2335-40.
- Talbot F, Nouwen A. A review of the relationship between depression and diabetes in adults: is there a link? Diabetes Care 2000;23:1556-62.
- Kovacs M, Goldston D, Obrosky DS, Bonar LK. Psychiatric disorders in youths with IDDM: rates and risk factors. Diabetes Care 1997;20:36- 44.
- Jordanova V, Stewart R, Goldberg D, Bebbington PE, Brugha T, Singleton N, et al. Age variation in life events and their relationship with common mental disorders in a national survey population. Soc Psychiatry Psychiatr Epidemiol 2007;42:611-6.
- Stegenga BT, Nazareth I, Grobbee DE, Torres-González F, Švab I, Maaroos H, et al. Recent life events pose greatest risk for onset of major depressive disorder during mid-life. J Affect Disord 2012;136:505-13.
- Padgett DK. Sociodemographic and disease-related correlates of depressive morbidity among diabetic patients in Zagreb, Croatia. J Nerv Ment Dis 1993;181:123-9.
- Spangler JG, Summerso JH, Bell RA, Konen JC. Smoking status and psychosocial variables in type 1 diabetes mellitus. Addict Behav 2001;26:21-9.
- Covey LS. Tobacco cessation among patients with depression. Prim Care 1999;26:691-706.
- Nierenberg AA, Petersen TJ, Alpert JE. Prevention of relapse and recurrence in depression: the role of long-term pharmacotherapy and psychotherapy. J Clin Psychiatry 2003;64 Suppl 15:13-7.
- Katon W, von Korff M, Ciechanowski P, Russo J, Lin E, Simon G, et al. Behavioral and clinical factors associated with depression among individuals with diabetes. Diabetes Care 2004;27:914-20.
- Lustman PJ, Griffith LS, Freedland KE, Clouse RE. The course of major depression in diabetes. Gen Hosp Psychiatry 1997;19:138-43.
- Jensen TS, Backonja MM, Hernández Jiménez S, Tesfaye S, Valensi P, Ziegler D. New perspectives on the management of diabetic peripheral neuropathic pain. Diab Vasc Dis Res 2006;3:108-19.
- Blackburn-Munro G, Blackburn-Munro RE. Chronic pain, chronic stress and depression: coincidence or consequence? J Neuroendocrinol 2001;13:1009-23.
- Chien IC, Lin CH, Chou YJ, Chou P. Increased risk of hyperlipidemia in patients with major depressive disorder: a population-based study. J Psychosom Res 2013;75:270-4.
- Chuang CS, Yang TY, Muo CH, Su HL, Sung FC, Kao CH. Hyperlipidemia, statin use and the risk of developing depression: a nationwide retrospective cohort study. Gen Hosp Psychiatry 2014;36:497-501.
- Roy T, Lloyd CE. Epidemiology of depression and diabetes: a systematic review. J Affect Disord 2012;142 Suppl:S8-21.
- Joensen LE, Almdal TP, Willaing I. Type 1 diabetes and living without a partner: psychological and social aspects, self-management behaviour, and glycaemic control. Diabetes Res Clin Pract 2013;101:278-85.
- Lustman PJ, Clouse RE. Treatment of depression in diabetes: impact on mood and medical outcome. J Psychosom Res 2002;53:917-24.
- Goldstein DJ, Lu Y, Detke MJ, Lee TC, Iyengar S. Duloxetine vs. placebo in patients with painful diabetic neuropathy. Pain 2005;116:109-18.