East Asian Arch Psychiatry 2010;20:101-8
ORIGINAL ARTICLE
A/Prof CB Osman, MD, MMedPsych, Faculty of Medicine, Universiti Teknologi Mara, Malaysia.
Dr Baharom Alipah, MD, MMedPsych, Department of Psychiatry, Pandan Hospital, Johor Bahru, Malaysia.
Dr M. Daud Tutiiryani, MBBS, MMedPsych, Department of Psychiatry, Universiti Kebangsaan Malaysia Medical Centre, Malaysia.
Prof Omar Ainsah, MD, MMedPsych, FCINP, PhD, Faculty of Medicine, Universiti Teknologi Mara, Malaysia.
Address for correspondence: A/Prof Che Bakar Osman, Faculty of Medicine, Universiti Teknologi Mara, Malaysia.
Tel: (60-3) 7726 5446; Fax: (60-3) 5544 2831; Email: Ocbaaaah@yahoo.com.my
Submitted: 11 January 2010; Accepted: 11 May 2010
Abstract
Objective: To determine the prevalence of depressive disorders among caregivers of patients with schizophrenia, its association with patient’s and caregiver’s socio-demographic characteristics and family functioning.
Methods: This was a cross-sectional study of caregivers of patients with schizophrenia at the outpatient clinic, Hospital Permai Johor Bahru, Malaysia. The study was conducted between August and October 2008. A total of 243 caregivers who fulfilled the inclusion criteria were enrolled, of whom 232 completed the self-administered socio-demographic questionnaire, the General Health Questionnaire (GHQ-30) and the McMaster Family Assessment Device. A total of 33 caregivers with the GHQ-30 cut-off point of 7/8 were assessed further by the Mini International Neuropsychiatric Interview to diagnose depressive disorder.
Results: The prevalence of psychological distress in our study sample was 14% (n = 33) and that of depressive disorders was 6% (n = 14). There was no association between patients’ and caregivers’ socio- demographic characteristics with depressive disorders, but there were significant associations between depressive disorders and family functioning dimensions in terms of Communication and Roles.
Conclusion: Although the causal link was not established, the results suggested that depression had a significant association with family functioning among caregivers of patients with schizophrenia.
Key words: Caregivers; Depressive disorder; Schizophrenia
摘要
目的:检视精神分裂症患者照顾者其抑鬱障碍的现患率、与患者和照顾者社会人口统计学特徵和家庭功能的关係。
方法:这项横断面研究於2008年8月至10月期间在马来西亚新山的门诊诊所进行,选出243名符合研究标準的参与者;当中232名照顾者完成有关社会人口统计的问卷调查、一般健康查询表(GHQ-30)和McMaster家庭评估。其後,33名GHQ-30达分界点7/8的照顾者透过微型国际神经精神评估确诊抑鬱障碍。
结果:照顾者的心理困扰现患率为14%(n = 33),而患抑鬱障碍的则占6%(n = 14)。患者和照顾者在社会人口统计学特徵和抑鬱障碍并无相关,但在家庭功能的沟通和角色功能上却与抑鬱障碍呈相关。
结论:虽然仍未能确立因果关係,但研究结果显示,精神分裂症患者照顾者的抑鬱症与家庭功能有一定相关性。
关键词:照顾者、抑鬱障碍、精神分裂症
Introduction
Schizophrenia is a severe mental disorder which has a considerable impact on families1 but many studies on the disorder have mainly focused on patients, with relatively less emphasis on the family.2
Patients with schizophrenia often remain physically and emotionally dependent on their relatives.1,3,4 The effect of mental illness on a family can be characterised by objective and subjective burden.2 Objective burden is the multiple tasks of taking care of patients. There are disruptions of household routines leading to social isolation of the affected family and impaired social functioning. Subjective burdens include the emotional distress characterised by feelings of stigmatisation, frustrations due to inability to fulfil personal plans, and commonly there is “burn out”.4 These burdens are associated with a number of specific patient and caregiver factors. Patient factors such as frequency of behavioural problems, length of illness and severity of illness have been positively related to caregivers’ burdens.5,6
There is also an increase in the prevalence of psychiatric morbidity among caregivers of patients with mental disorders, in particular depression and anxiety owing to financial difficulties and disruption of leisure activities.7-10 Several studies have tried to evaluate the link between family functioning and depression.9,11,12 Among the spouses of patients suffering from mental disorders, female spouses have prevalence rates for all psychiatric illness that are 1.8 to 2.5 times that of male spouses.13 Many caregivers’ variables have been reported as being significantly related to their development of depression, including the general stress of coping with chronic psychiatric illness.11
A study on patients with chronic schizophrenia and family burden found that 80% of such families reported that providing care disrupts their routine, 71% reported strained family relationship, and 62% faced financial burden.14
The greatest burden (experienced by 90% of families) was concern about the patient’s future and recovery.14 Another study found that mothers of children with schizophrenia had higher rates of depression and anxiety than controls.15
However it is unclear whether family dysfunction leads to the depression or vice versa.16,17 The family members with depressive symptoms often go undetected and untreated, it is therefore necessary to assess for emotional disturbance in caregivers and manage them accordingly. The objective of this study was therefore to determine the prevalence of depressive disorders among caregivers of patients with schizophrenia, its association with patients’ and caregivers’ socio-demographic characteristics, and association between depressive disorders and family functioning.
Methods
Study Setting
This study was conducted at the outpatient clinic of Hospital Permai Johor Bahru. This is one of the premier mental institutions and the second largest psychiatric hospital in Malaysia, which is a secondary and tertiary referral centre. Its services include inpatient and outpatient psychiatry comprising: child and adolescent psychiatry, community psychiatry, substance abuse, and forensic psychiatry. Apart from providing services for the state of Johor, the hospital also provides services mainly for the southern and eastern states of Malaysia. The outpatient psychiatry clinics (run by medical officers and psychiatrists) operate 3 days a week and the average number of patients attending the outpatient clinic is about 150 per week.
Study Design and Sample
This was a cross-sectional study carried out from 1 August to 30 October 2008. The sample comprised caregivers of patients with schizophrenia who attended outpatient clinic of the hospital.
The patients’ diagnosis of schizophrenia was made by clinical interview based on the 4th edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) criteria.18 Inclusion criteria were: being caregivers of any patients with schizophrenia aged above 18 years, who gave informed consent to participate in the study. Caregivers who had difficulty understanding or completing the questionnaires were excluded.
Calculation of Sample Size
The sample size calculation was based on the following formula19:
n = [z2 p(1-p)]/d2, i.e.
n = [1.962 * 0.22 * (1-0.22)]/0.052 = 263
In this formula, the expected proportional prevalence (p) for depressive disorders was estimated as 22% (based on the prevalence of major depressive disorders among caregivers).8,9 Using the formula, the sample size calculated was 263.
Clinical Interview for the Revised Third Edition and Fourth Edition of the Diagnostic and Statistical Manual of Mental Disorders
Clinical Interview for the revised 3rd edition and 4th edition of the Diagnostic and Statistical Manual of Mental Disorders18 was used to ascertain the diagnosis of schizophrenia.
General Health Questionnaire
In this study, a Malay translation of the General Health Questionnaire–30 (GHQ-30)20 was used. This version was validated in the local community.20 The cut-off point of 7/8 was used to determine cases, which yields a specificity of 96% and a sensitivity of 93%.18
McMaster Family Assessment Device
The McMaster Model of the Family Functioning (MMFF) questionnaire was a clinically oriented conceptualisation of families, which evaluated the structural and organisational properties of the family and patterns of transactions among family members so as to distinguish between those who were healthy and unhealthy interactions.21
The model identifies 6 dimensions of family functioning. Problem-solving (the first dimension) refers to the family’s ability to solve problems at the level that maintains effective family functioning. The second dimension is Communication, which is the exchange of information among family members. The third dimension is Roles, which is the family’s established patterns of behaviour for handling a set of family functions, including: provision of resources, providing nurturance, supporting personal development, maintaining and managing family systems, and providing adult sexual gratification. The scale also looks into whether tasks are clearly and equitably assigned to family members and whether they are carried out in a responsible manner. Affective Responsiveness is the fourth dimension and assesses the extent to which individual family members are able to experience appropriate affect over a range of stimuli. The fifth dimension, Affective Involvement, is the extent to which the family members are interested in and place a value on each others’ activities and concerns. The final dimension of the MMFF is Behaviour Control, which assesses the way in which a family maintains standards of behaviour of its members.21
The Family Assessment Device (FAD) is made up of 7 scales, one is General Functioning which assesses the overall health / pathology of the family. The other 6 deal with the 6 dimensions mentioned previously. This questionnaire is self-rated and can be filled out by family members aged over 12 years. The questionnaire consists of 60 items and the subjects have to rate their agreement or disagreement with how well an item describes their families by selecting between 4 alternative responses (ranging from strongly agree to strongly disagree).21
Concurrent validity was good at R = 0.53 and predictive validity was powerful. The test-retest reliability for the different scales was good and ranged from 0.66 for Problem-solving to 0.76 for Affective Responsiveness. Cut-off points had been developed for each of the scales and were found to have good sensitivity and specificity. This FAD has been translated to Malay and back-translated into English. The FAD Malay version has been successfully used by other local researchers22-24 and was therefore selected for use in this study.
Mini International Neuropsychiatric Interview
The interviewer was trained in the use of the Mini International Neuropsychiatric Interview (MINI)25 by an experienced senior psychiatrist. The inter-rater reliability for this study was ascertained by randomly interviewing 1% of the cases. Calculation of reliability coefficients for a 2-point category scale revealed that both the senior psychiatrist and the interviewer had a kappa of 1.
Operational Definitions
Caregivers
A caregiver who accompanied the patient could be a mother, father, husband, wife, partner, relative, son, daughter or a friend living in the same household.26
Depressive Disorder
Depressive disorders were diagnosed based on the MINI25 and defined according to the criteria from the 4th edition of the DSM-IV,18 and consisted of major depressive disorders and dysthymic disorders.
Family Functioning
These were the 7 domains of family functioning. If the mean was greater than the cut-off point it indicated an unhealthy family. This suggested that the family was having difficulties with the area of functioning. However, in order to effectively identify the presence of significant family dysfunction, at least 6 of the 7 dimensions needed to be affected.21
Statistical Analysis
Data were analysed using the Statistical Package for Social Sciences (SPSS) computer program, Windows version 10. Independent t tests (parametric) were used to compare the means of normally distributed continuous data in 2 groups. The Chi-square tests were used as a test of significance for categorical variables with 2 x 2 tables and the Mann- Whitney U test was used to analyse differences between 2 groups with categorical and continuous data.
Ethical Consideration
This research project was approved by the Research and Ethics Committee, University Kebangsaan Malaysia and Hospital Permai, Johor Bahru, Johor. Informed consent was obtained from the patient and caregiver. The purpose of the study was explained. All the respondents were assured of data confidentiality, and subjects were included on a voluntary basis. The data were then keyed into the SPSS software anonymously.
Results
A total of 310 patients with schizophrenia attended the psychiatric outpatient clinic of Hospital Permai Johor Bahru between August and October 2008, of whom 280 patients were accompanied by caregivers and 30 came alone. Thirty two caregivers were excluded because of communication problems whilst 5 refused to participate.
A total of 243 participants were enrolled into the study, 11 refused consent and were excluded. Of the 232 participants, 33 were identified as having psychological distress based on GHQ-30 cut-off of 7/8 and were further assessed by MINI. To evaluate the specificity of MINI in detecting depressive disorder, the MINI was also randomly administered to 20 (10%) of the participants who were screened as non-cases by the GHQ-30. The time from the initial phase of self-reported questionnaires and the interview ranged from 7 to 14 days.
Demographic Characteristics of Patients
The mean age of patients with schizophrenia was 37 years, and the majority were males. Almost two thirds of the patients were Malay and studied up to the secondary level, and two thirds were single and unemployed. The median (standard deviation [SD]) number of admissions within 5 years was 1 (2). The median duration of their illness was 8 years. Also, 7% had a history of substance misuse, and half of these patients were treated with atypical antipsychotics.
Socio-demographic Characteristics of Caregivers
The mean (SD) age of the caregivers was 47 (14) years, most were male, and almost two thirds were Malay. Half of them had received secondary education, a quarter had studied up to the primary level, 10% up to tertiary level, and only a small proportion had had no formal education. The majority were married and almost two thirds were employed and had an average monthly income of RM1890 (about US$550).
Clinical Variables of Caregivers
Almost half of the caregivers were parents, and one third were either nephews, uncles or aunties; a small proportion were sons or daughters. Almost two thirds of the sample did not have a recent stressor (in the past 3 months). The median number of children was 3. The median number of family members who stayed together with the patient was 4 and the median contact hours per day was 12.
Prevalence of Depressive Disorder in Caregivers
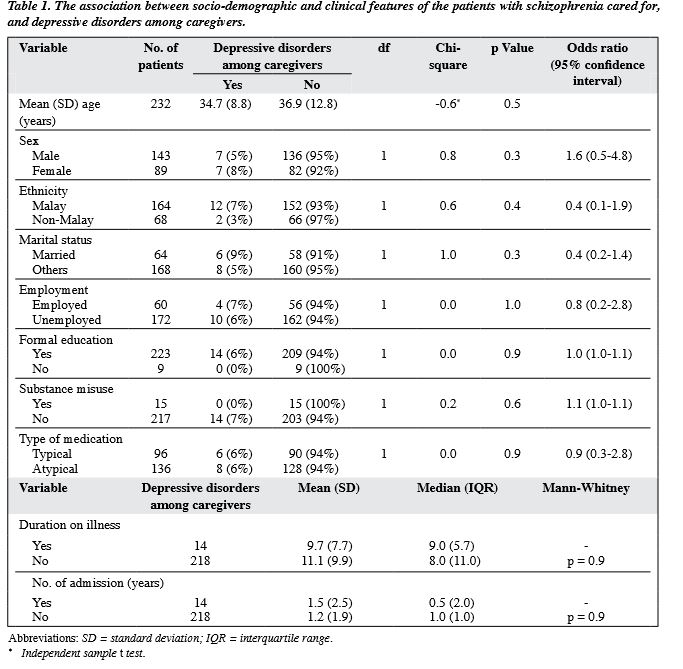
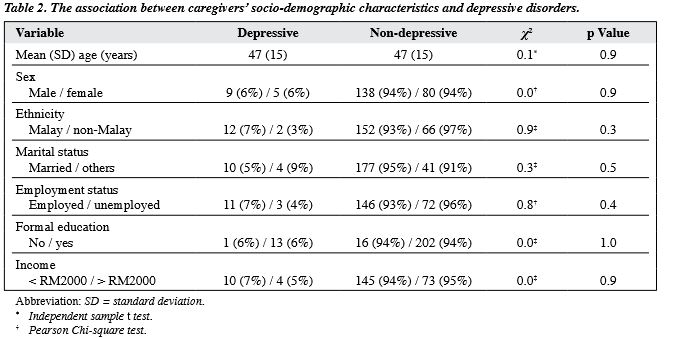
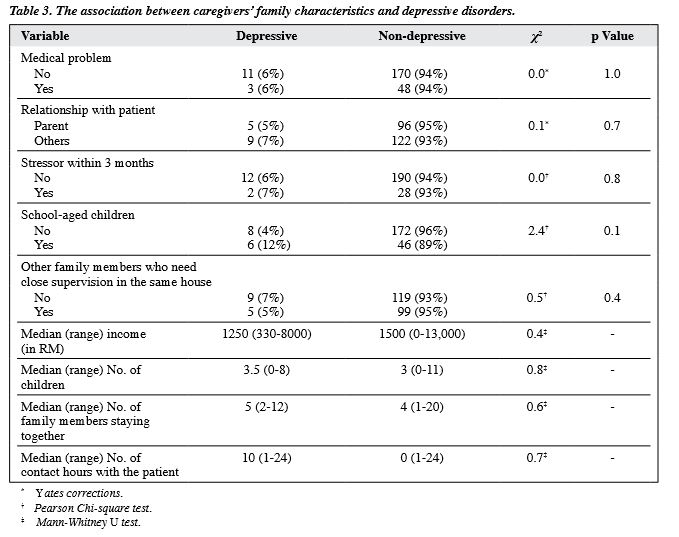
The prevalence of psychological distress in this study, as determined by GHQ-30 at cut-off points of 7/8, was 14% (n = 33). In this sample, the prevalence of depressive disorders based on the MINI was 6% (n = 14); 5% (n = 11) had major depressive disorders, and 1% had dysthymia (n = 3). There was no significant association between caregivers with and without depressive disorders with respect to the socio-demographic characteristics and clinical features of those in their care (Table 1); no significant correlation was also shown between caregivers’ depressive disorders and their own socio-demographics (Table 2) and family characteristics (Table 3).
Family Functioning Dimension
The family functioning among caregivers of patients with schizophrenia showed that almost all domains in family functioning were unhealthy (p < 0.05) except for Problem- solving and General Functioning.
Association between Depressive Disorders and Family Functioning
There were significant differences between depressive disorders and family functioning dimensions in terms of Communication and Roles (Table 4; p < 0.05).
Discussion
Although there have been studies on the caregivers of patients with schizophrenia,14,27,28 the present study was the first that examined family functioning. In contrast to previous studies,14,27,28 we found the majority of our respondents were male. In Malaysia it was not uncommon for males to accompany patients to hospital and for females usually to stay at home attending to housework. We found that the prevalence of psychological distress was 14%; and half of these met the DSM-IV criteria for depressive disorder, which was lower than that in other studies.14,27,29 This was probably because of a gender bias; the majority of our caregivers that accompanied patients to hospital were males, whilst females had a higher prevalence of depression. The differences in methodology used for diagnosis of depression could also have influenced the findings: we used a diagnostic tool, while the previous study used a screening instrument (i.e. the Centre for Epidemiological Studies Depression Scale).30 Moreover, we used a broader definition of caregivers, so that the subjects that were recruited might or might not have been the primary caregivers.
Another possible reason was that the patients’ symptoms were not measured. Several studies have found that patients’ positive symptoms were significantly related to caregivers’ depression.31,32 A study on burden of care of schizophrenia in Malay families in Kelantan found that the severity of the burden among caregivers was significantly correlated with the number of problem behaviours and previous admissions; Malay caregivers were generally more able to tolerate the negative symptoms and did not require many admissions.28 Due to some technical difficulties, in this study the severity of positive symptoms was not measured. The median number of admissions for our patients within 5 years was only 1, and thus they might have had relatively mild symptoms.
Family Functioning
Family functioning among caregivers of patients with schizophrenia showed that most of the domains of the family functioning were unhealthy, which was consistent with the previous study.33 Although we could not determine the cause for the unhealthy family functioning, we could postulate this was due to the presence of emotional distress, frustration, and burnout often associated with taking care of patients with schizophrenia. However the causal relationship between family functioning and course of illness is rather unclear. Although a family member’s illness could have a negative impact on family functioning, the dysfunctional family might also precipitate, exacerbate, or delay recovery from an illness episode. Our finding supported the relationship between depressive disorders and unhealthy family functioning. In this study, there were significant differences between dimension of family functioning in terms of Communication and Roles, and depressive disorders. Unal et al12 reported that the general functionality level was low in families with schizophrenia and subscales of Communication, whilst Behaviour Control was reported as highly ineffective.
There were several limitations in this study that needed to be highlighted. The results could only represent the study population, there being no comparison between participants and those who refused. Although the use of self-reported questionnaires was cost-efficient, they could be considered a limitation and might contribute to information bias. The severity of positive symptoms, violent behaviour, life events, premorbid personality, and severity of the illness were not assessed in this study. Many of the latter could have given rise to a strong and immediate relationship with the level of psychological distress, which could act as powerful confounders.
The caregiver sample size (n = 232) was rather small. This would give rise to type II error; a larger sample size may have given more accurate information. This study could have been improved by prolonging its duration beyond 3 months. The prevalence of psychological distress suggested that about 10% of caregivers suffered from psychological distress. Among caregivers who are psychologically distressed, approximately half had reached clinical depression and they were mostly undiagnosed and untreated.
This study demonstrated that depression had a significant effect on family functioning in the caregivers of patients with schizophrenia. Since this was a cross-sectional study, the causal link was not established. The results suggest that active assessment of family mental health and functioning in patients with schizophrenia is crucial. Future prospective studies should be carried out to examine the mental health of caregivers of both schizophrenia and other mental health problems with a larger sample size.
Acknowledgements
We would like to thank the Director of Hospital Universiti Kebangsaan Malaysia and all caregivers who had agreed to participate in this study.
References
- 1. Birchwood M, Cochrane R. Families coping with schizophrenia: coping styles, their origins and correlates. Psychol Med 1990;20:857-65.
- Boye B, Bentsen H, Ulstein I, Notland TH, Lersbryggen A, Lingjaerde O, et al. Relatives’ distress and patients’ symptoms and behaviours: a prospective study of patients with schizophrenia and their relatives. Acta Psychiatr Scand 2001;104:42-50.
- Gallagher SK, Mechanic D. Living with the mentally ill: effects on the health and functioning of other household members. Soc Sci Med 1996;42:1691-701.
- Martens L, Addington J. The psychological well-being of family members of individuals with schizophrenia. Soc Psychiatry Psychiatr Epidemiol 2001;36:128-33.
- Biegel DE, Milligan SE, Putnam PL, Song LY. Predictors of burden among lower socioeconomic status caregivers of persons with chronic mental illness. Community Ment Health J 1994;30:473-94.
- 6. Chakrabarti S, Kulhara P, Verma SK. The pattern of burden in families of neurotic patients. Soc Psychiatry Psychiatr Epidemiol 1993;28:172-7.
- Hatfield AB. Psychological costs of schizophrenia to the family. Soc work 1978;23:355-9.
- Esther AA. Coping strategies and depression in caregivers of patients with mental disorders: a case study in a tertiary hospital in Nigeria. Nig J Health and Biomed Sci 2003;2:103-7.
- Heru A, Ryan C. Depressive symptoms and family functioning in the caregivers of recently hospitalized patients with chronic / recurrent mood disorders. Int J Psychosoc Rehabil 2002;7:53-60.
- Cochrane JJ, Goering PN, Rogers JM. The mental health of informal caregivers in Ontario: an epidemiological study. Am J Public Health 1997;87:2002-7.
- Song LY, Biegel DE, Milligan SE. Predictors of depressive symptomatology among lower social class caregivers of persons with chronic mental illness. Community Ment Health J 1997;33:269-86.
- Unal S, Kaya B, Cekem B, Ozişik HI, Cakil G, Kaya M. Family functioning in patients with schizophrenia, bipolar affective disorder and epilepsy [in Turkish]. Turk Psikiyatri Derg 2004;15:291-9.
- Wittmund B, Wilms HU, Mory C, Angermeyer MC. Depressive disorders in spouses of mentally ill patients. Soc Psychiatry Psychiatr Epidemiol 2002;37:177-82.
- Noryati AA. Chronic schizophrenia and family burden. Master of Medicine (psych) [thesis]. Universiti Kebangsaan Malaysia; 1991.
- Espina A, Ortego A, Ochoa de Alda I, Gonzalez P. Dyadic adjustment in parents of schizophrenics. Eur Psychiatry 2003;18:233-40.
- Tarrier N, Lowson K, Barrowclough C. Some aspects of family interventions in schizophrenia. II: Financial considerations. Br J Psychiatry 1991;159:481-4.
- Butzlaff RL, Hooley JM. Expressed emotion and psychiatric relapse: a meta-analysis. Arch Gen Psychiatry 1998;55:547-52.
- Diagnostic and Statistical Diagnosis for Mental Disorders, fourth edition. American Psychiatric Association; 1993.
- Lwanga SK, Lemeshow S. Sample size determination in health studies: a practical manual. Geneva: World Health Organization; 1991.
- Hamid A, Hatta S. A validation study of the Malay language translation of General Health questionnaire-30. Malays Psychiatr J 1996;2:34-8.
- Epstain NB, Keitner GI, Bishop DS. Family functioning in the families of psychiatric patients. Compr Psychiatry 1986;27:302-12.
- Zulkifli G. Marital and family functioning as perceived by spouses of depressed patients. Master of Medicine (Psych) [thesis]. Universiti Kebangsaan Malaysia; 1995.
- Loh CC. Family functioning in alcohol dependents — a controlled study. Master of Medicine (Psych) [thesis]. Universiti Kebangsaan Malaysia; 1995.
- Eni R. Individual coping and family functioning of patients with diabetes mellitus and the relationship with diabetic control. Master of Medicine (Psych) [thesis]. Universiti Kebangsaan Malaysia; 1997.
- Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, et al. The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry 1988;59 Suppl 20:S22-33.
- Salleh MR. The burden of care of schizophrenia in Malay families. Acta Psychiatri Scand 1994;89:180-5.
- 27. Nora MZ. A preliminary study on quality of life and psychiatric morbidity among the primary caregivers of patients with chronic schizophrenia in the hospital Universiti Kebangsaan Malaysia. Master of Medicine (Psych) [thesis]. Universiti Kebangsaan Malaysia; 2004.
- Siti Salwa R. Quality of life and psychological well being of caregivers of patients with schizophrenia receiving assertive community treatment — a cross sectional study. Master of Medicine (Psych) [thesis]. Universiti Kebangsaan Malaysia; 2008.
- Magaña SM, Ramírez García JI, Hernández MG, Cortez R. Psychological distress among Latino family caregivers of adults with schizophrenia: the roles of burden and stigma. Psychiatr Serv 2007;58:378-84.
- Schene AH, van Wijngaarden B, Koeter MW. Family caregiving in schizophrenia: domains and distress. Schizophr Bull 1998;24:609-18.
- Raj L, Kulkara PJ. Social burden of positive and negative symptoms of schizophrenia. Int J Soc Psychiatry 1999;37:242-50.
- Provencher HL, Mueser KT. Positive and negative symptom behaviors and caregiver burden in the relatives of persons with schizophrenia. Schizophr Res 1997;26:71-80.
- Noh S, Turner RJ. Living with psychiatric patients implications for the mental health of family members. Soc Sci Med 1987;25:263-72.