East Asian Arch Psychiatry 2010;20:87-91
ORIGINAL ARTICLE
Ms Sit-Fong Loh, MClinPsych, Department of Psychiatry, Universiti Kebangsaan Malaysia Medical Centre, Kuala Lumpur, Malaysia.
Prof Thambu Maniam, MBBS, MPM, FAMM, Department of Psychiatry, Universiti Kebangsaan Malaysia Medical Centre, Kuala Lumpur, Malaysia.
A/Prof Susan MK Tan, MD, DCH, MMed (Psych), Adv.M.Ch.Ado.Psych, AM, Department of Psychiatry, Universiti Kebangsaan Malaysia Medical Centre, Kuala Lumpur, Malaysia.
Dr Yahya Badi’ah, MD, MMed (Psych), Hospital Permai, Johor Bahru, Malaysia.
Address for correspondence: Ms Sit-fong Loh, Department of Psychiatry, Universiti Kebangsaan Malaysia Medical Centre, Jalan Yaacob Latif, Bandar Tun Razak, Cheras, 56000 Kuala Lumpur, Malaysia.
Tel: 603-91456164; Fax: 603-91737841; Email: sitfong@yahoo.com
Submitted: 17 September 2009; Accepted: 11 January 2010
Abstract
Objective: To describe the association between childhood adversity and depression in adult depressed patients in a Malaysian population.
Methods: Fifty-two patients, who met the criteria for major depressive disorder or dysthymia according to the Structured Clinical Interview based on the revised 3rd edition of the Diagnostic and Statistical Manual of Mental Disorders, were used as cases and compared with 52 controls matched for age and sex. Cases and controls were assessed using a sexual and physical abuse questionnaire and a Parental Bonding Instrument.
Results: There was a positive relationship between childhood abuse in general and childhood physical abuse with adult depressive disorder in particular. Nearly a quarter (23%) of depressed patients reported being abused in childhood compared with none in the control group. There was no significant association between childhood loss and depression in adulthood. Low level of parental care during childhood was significantly correlated with adult depressive disorder.
Conclusion: Clinicians should assiduously seek a history of childhood adversities in adult patients with depression. This information can influence clinical management by way of implementing secondary preventive measures. In all depressed patients, mental health professionals also need to look out for their poor attachment with parents during childhood. This may enable interventions directed at parenting skills and improved attachment relationships with their own children. These types of interventions together with pharmacotherapy may provide the optimal approach to the management of depression in adults and help prevent the cycle of depression perpetuating itself in the next generation.
Key words: Child abuse; Depression; Maternal behavior
摘要
目的:描述马来西亚成人抑郁患者的发病与其童年逆境的关系。
方法:研究包括52名符合《心理疾病诊断统计手册(第三版)》临床会诊量表标准的抑郁症患者,以及52名年龄与性别相互配合的人士作对照组,透过性虐待/身体虐待和父母教养方式问卷对两组作出评估。
结果:成人抑郁一般与其童年受虐,尤以身体虐待呈正相关。约四分一(23%)抑郁患者表示曾于童年受到虐待,而对照组则无相关经历。童年逆境与成人抑郁没有显著关系,但儿时父母关怀不足则与成年患上抑郁呈明显正相关。
结论:临床工作者必须积极寻找成人抑郁患者的童年逆境史;资讯有助临床管理。精神健康专职人员也需要为抑郁患者找出他们儿时与父母关系欠佳的原因,让治疗能定点于父母教育技巧并改善双方关系,加上药物治疗,有助医治成人抑郁症,减低他们下一代遇上类似经历的机会。
关键词:童年虐待、抑郁症、教养行为
Introduction
Self-reported childhood adversities are associated with mental disorders in adults, particularly depression.1 A wide variety of childhood experiences confer biological, psychological, and social disadvantages that contribute to vulnerability to depression. Such experiences range from parental mental illness or substance abuse, poor parenting, family turmoil or violence, death of or separation from parents, and childhood physical or sexual abuse. These childhood adversities are associated with difficulty forming successful marital relationships, playing a successful role as an adult, poor coping skills, as well as intrapsychic vulnerabilities such as low self-esteem, helplessness, and interpersonal dependency.
A population study by Pirkola et al2 found that 17% of adults reporting at least 1 childhood adversity had a current mental disorder, compared with 10% of those without any childhood adversity. They also found that paternal mental health problems associated particularly strongly with male depressive disorders (odds ratio [OR], 4.46), and maternal mental health problems with female depressive disorders (OR, 3.20). In a large, 3-year community longitudinal follow-up study,3 childhood abuse and multiple adversities were strongly associated with future suicidal behaviour, even after exclusion of the effect of mental disorders.
The objective of this study was to describe the association between childhood adversities in adult depressed patients and depression in a Malaysian population.
Methods
Sampling Frame and Recruitment Centre
This was a case-controlled study involving patients from the psychiatric clinics of the Hospital Kuala Lumpur and Universiti Kebangsaan Malaysia Medical Centre, who were selected through convenient sampling. The controls were recruited from patients’ relatives or hospital staff, matched for gender, age and education level, and were also administered the Structured Clinical Interview for the revised 3rd edition of the Diagnostic and Statistical Manual of Mental Disorders (SCID), so as to exclude those who were depressed.
Subjects
All patients who fulfilled inclusion criteria of major depressive disorder or dysthymia were interviewed upon obtaining written consent. The subjects had to be between 18 and 50 years and were able to converse in Bahasa Malaysia or English. Subjects with depression secondary to alcoholism, substance abuse or other organic causes were excluded from the study.
Procedures
The diagnosis of major depressive disorder or dysthymia was made using the patient version of the SCID4 administered by a trained researcher. The SCID is a semi-structured diagnostic questionnaire administered by an interviewer trained in making psychiatric diagnoses.
Self-rated questionnaires in English and Bahasa Malaysia, i.e. the Parental Bonding Instrument (PBI),5 Tennessee Self-Concept Scale (TSC),6 and Locke-Wallace Marital Adjustment Scale (L-WMAS)7 were administered to all participants. The PBI is a self-rated questionnaire to elicit a person’s memory of his or her upbringing. The questionnaire has 25 items measuring 2 principal dimensions of ‘care’ and ‘overprotection’ given by parents. These dimensions are tested as valid measures of the perceived characteristics and not the actual behaviours.5
The TSC is a self-rated questionnaire which reflects current self-perception of worth, self-confidence and action, whereas the L-WMAS is a self-reported questionnaire assessing marital happiness, extent of disagreement in certain areas of marriage, and the extent of the spouse’s role in decision-making and commitment to the marriage.
The history of childhood physical abuse was obtained through an interview using the Childhood History Questionnaire,8 which is a self-reported measure assessing an individual’s history of experiencing physical abuse. Any history of childhood sexual abuse was obtained through an interview focusing on the nature of the sexually abusive acts experienced, demographic characteristics of the perpetrator(s), age when the abuse began, duration, and frequency of the abuse.9 Socio-demographic data and any history of childhood loss through death or separation were also obtained through an interview.
Ideally, the control group should be the nearest ordinal siblings of the subjects who had grown up with them throughout childhood, so as to control for confounding factors that would bias the outcome. The researchers chose a non-depressed population as a control if no siblings were available, or the subjects did not allow the researchers to involve their siblings. The controls were then recruited from the outpatient clinic or staff. Efforts were taken to match both groups as closely as possible with respect to variables that had to be controlled. The controls went through the same interview and self-rated questionnaires as the subjects.
In this paper, we report results for the associations among childhood adversities, parental bonding, and depression. Data from the TSC and L-WMAS are not reported here.
Statistical Analysis
Demographic data, childhood adversities, and associated factors were analysed using the Chi-square test, Fisher’s exact test, Mann-Whitney U test, Spearman’s correlation test, as well as ORs. This study was approved by the Research Committee of Department of Psychiatry, Universiti Kebangsaan Malaysia, which also examined ethical issues.
Results
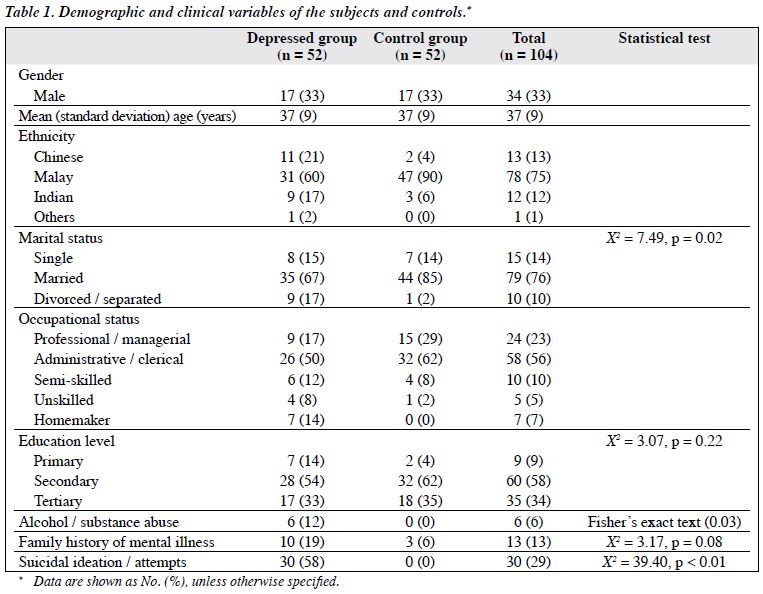
A total of 52 depressed patients and 52 matched controls were included in this study. Their socio-demographic and clinical variables are shown in Table 1.
Both depressed and control groups were matched in terms of gender and age. Females were predominant (67%). In terms of ethnic distribution, Malays (75%) were the majority, followed by Chinese (13%) and Indians (12%). However, there was a significant difference in terms of marital status between the depressed and control groups (p = 0.02). In the depressed group, 67% of the subjects were married whereas in the controls 85% were married.
There was a higher percentage of depressed subjects whose marriage did not succeed as they were divorced or separated (17% compared with 2% in the control group). Most subjects received secondary education. There was no significant difference in terms of education level between the depressed (54%) and control groups (62%).
In the depressed group, 12% had a history of alcohol or substance abuse compared with none in the controls (p = 0.03). Meanwhile, 19% of depressed patients had a family history of psychiatric illness compared with 6% in the controls, though this difference was not statistically significant (p = 0.08). There was a significant difference in terms of suicidal risk between the depressed and control groups; in the depressed group, 58% had a history of suicide attempts or thoughts of dying (p < 0.01).
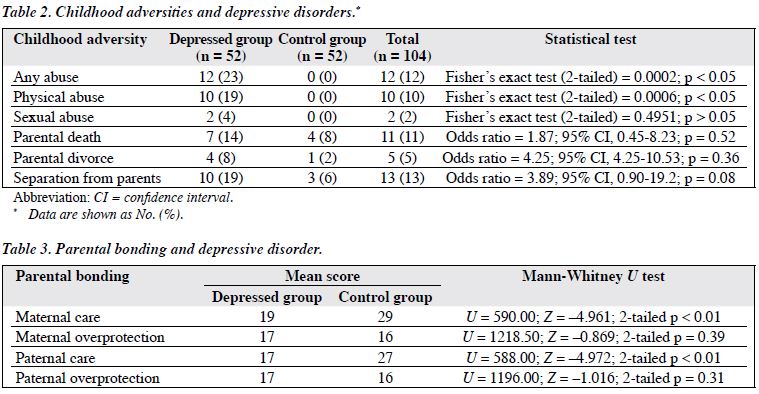
Table 2 shows the association between childhood adversity and depressive disorder. There was a significant difference in reported childhood abuse between the depressed and control groups. In the depressed group, 23% had a history of childhood abuse when considered in general (p < 0.05). However, when sub-classified into physical and sexual abuse, only physical abuse showed a significant difference (p < 0.05). As for childhood loss, there were no significant differences between the depressed and control groups in all sub-classifications of childhood parental death, parental divorce, and childhood separation.
Table 3 shows results describing the association between parental bonding and depressive disorder. There were significant differences in terms of maternal and paternal care between the depressed and control groups. The mean maternal care score for the depressed subjects was 19, compared with 29 in the controls (p < 0.01). Similar findings pertained to paternal care score (17 in the depressed group vs. 27 in the controls, p < 0.01). There were no significant differences in maternal and paternal overprotection in the 2 groups.
Discussion
According to this study, nearly a quarter (23%) of depressed subjects in this sample had experienced some form of abuse in childhood, which was similar to reports from elsewhere.10-12 Among the depressed subjects, 19% reported a history of physical abuse and 4% had a history of childhood sexual abuse.
In this study, physical abuse was much more common than sexual abuse. The somewhat low percentage of sexual abuse could be due to reticence to describe a topic that is embarrassing. In addition, the small sample size could have contributed to this low percentage. However, Sheldon13 quoted a figure of between 4% and 44% adult female psychotherapy referrals as having experienced childhood sexual abuse. This indicates that there is a wide range in the rate of sexual abuse in different studies. In the National Comorbidity Survey in the USA, childhood sexual abuse, whether alone or with other adversities, was associated with an increased risk of adult psychopathology.12
In our study, 19% of depressed subjects had a history of physical abuse, compared with 11% in the study by Springer et al.10 Physical abuse is known to be associated with increased risk of suicidal ideation and attempts.11 The latter study showed that suicidal ideation was very strongly associated with childhood physical abuse.
Whatever the ‘stress’ experienced as children, whether it be physical or sexual or even emotional, research has shown that it becomes ‘tolerable’ if there are supportive adults present who create a safe environment for the child to learn to cope with and to recover from the event.14 This critical role of secure relationships results in a more controlled stress reactions and allows the child to explore the world, meet challenges, and be frightened at times without sustaining the adverse neurological impact of chronically elevated levels of stress which induced hormones such as cortisol. The latter is believed to increase reactivity of selected brain systems to stress and threats.14 Thus, adequate parental care acts as a buffer against children developing depression. The depressed patients in this study had much lower levels of maternal and paternal care than the controls. It was therefore possible that such lower levels of care are insufficient to buffer the effect of negative life experiences that lead to depression.
It has also been postulated that adversities give rise to elevated cortisol levels, which may alter the development of brain circuits in ways that made them less capable of coping effectively with stress as they grow up.15 Not surprisingly, the depressed group had significantly poorer coping strategies as evidenced by alcohol or substance abuse and suicidality. They also had problems maintaining a marital relationship compared with the controls (17 % vs. 2%, p = 0.02).
This study failed to show any significant association between childhood parental death and depressive disorder in adulthood, which was in contrast to findings described by Brown and Harris.16 However, our finding was in keeping with the studies by Perris et al17 and Roy,18 who noted that parental death before the age of 15 and 17 years, respectively, was not associated with depressive disorder in adulthood. Breier et al19 also found no significant difference between the depressed (61%) and non-depressed groups (76%) in relation to the risk of parental death. Therefore, it is not possible to judge the effects of a parental death on a child using a single determination theory. Mireault and Bond20 suggested that perceived vulnerability to loss could be a better predictor of adult depression than the actual loss itself. Additionally, as postulated by Rutter et al,21 the disorder could actually stem from deficient care that follows the loss, rather than the loss per se.
Nearly 8% of the depressed group had a childhood history of parental divorce compared with 2% of the controls, but this difference was not statistically significant (p = 0.36). This finding was not consistent with that found by Roy18 and Gilman et al22 who attributed parent-child separations mostly due to divorce as a significant predictor of depression. The negative finding in this study could be due to the small sample size; only 4 depressed subjects had experienced early parental divorce.
Limitations of this study included under-reporting by respondents (due to embarrassment, or unwillingness to disclose painful memories), and the small sample size resulting in lack of sufficient power to identify differences as statistically significant. Another limitation entailed recall bias: depressed persons might be biased towards recalling more negative experiences, whereas the non-depressed might recall or report less adverse life experiences to avoid embarrassment in talking about perceived shameful private experiences like sexual. It may be inferred that resorting to the relatives of patients to recruit controls may possibly introduce significant bias, as they might have been more likely to share the same psychosocial environment in childhood. We surmise that the effect of including them would, if anything, reduce the differences between the subjects and controls for some of the measures.
Our findings have importance in that clinicians should assiduously seek a history of childhood adversities in adult patients with depression. This kind of information might influence clinical management as there is some evidence that such adults might not respond well to conventional antidepressant treatment.23 In which case a bio-psychosocial approach to manage adult depressed patients with a history of chronic childhood adversities might be particularly beneficial.
As a means of secondary prevention, mental health professionals also need to look out for poor attachment with parents during childhood in adult patients who are depressed. This could enable interventions to enhance parenting skills and improvement of attachment relationships with their own children, and thus try to prevent the cycle of depression perpetuating into the next generation.
Acknowledgement
The authors would like to thank the Research Committee of the Department of Psychiatry, Universiti Kebangsaan Malaysia (National University of Malaysia) Medical Centre for approval to conduct this study. There was no conflict of interest in this study.
References
- Kessler RC, Davis CG, Kendler KS. Childhood adversity and adult psychiatric disorder in the US National Comorbidity Survey. Psychol Med 1997;27:1101-19.
- Pirkola S, Isometsä E, Aro H, Kestilä L, Hämäläinen J, Veijola J, et al. Childhood adversities as risk factors for adult mental disorders: results from Health 2000 study. Soc Psychiatry Psychiatr Epidemiol 2005;40:769-77.
- Enns MW, Cox BJ, Afifi TO, De Graaf R, Ten Have M, Sareen J. Childhood adversities and risk for suicidal ideation and attempts: a longitudinal population-based study. Psychol Med 2006;36:1769-78.
- Williams JB, Gibbon M, First MB, Spitzer RL, Davies M, Borus J, et al. The Structured Clinical Interview for DSM-III-R (SCID). II. Multisite test-retest reliability. Arch Gen Psychiatry 1992;49:630-6.
- Parker G, Tupling H, Brown LB. A parental bonding instrument. Br J Med Psychol 1979;52:1-10.
- Roid GH, Fitts WH. Tennessee Self-Concept Scale: revisited manual. Los Angeles, CA: Western Psychological Services; 1988.
- Locke HJ, Wallace KM. Short marital adjustment and prediction tests. Their reliability and validity. Marriage Farm Living 1959;21:251-5.
- Litty CG, Kowalski R, Minor S. Moderating effects of physical abuse and perceived social support on the potential to abuse. Child Abuse Negl 1996;20:305-14.
- Gold SN, Hughes DM, Swingle JM. Characteristics of childhood sexual abuse among female survivors in therapy. Child Abuse Negl 1996;20:323-35.
- Springer KW, Sheridan J, Kuo D, Carnes M. Long-term physical and mental health consequences of childhood physical abuse: results from a large population-based sample of men and women. Child Abuse Negl 2007;31:517-30.
- McHolm AE, MacMillan HL, Jamieson E. The relationship between childhood physical abuse and suicidality among depressed women: results from a community sample. Am J Psychiatry 2003;160:933-8.
- Molnar BE, Buka SL, Kessler RC. Child sexual abuse and subsequent psychopathology: results from the National Comorbidity Survey. Am J Public Health 2001;91:753-60.
- Sheldon H. Childhood sexual abuse in adult female psychotherapy referrals. Incidence and implications for treatment. Br J Psychiatry 1988;152:107-11.
- Excessive stress disrupts the architecture of the developing brain. National Scientific Council on the Developing Child. 2005; Working Paper No. 3. http://www.developingchild.net/pubs/wp/excessive_stress.pdf . Accessed 25 Aug 2009.
- Gunnar MR, Donzella B. Social regulation of the cortisol levels in early human development. Psychoneuroendocrinology 2002;27:199- 220.
- Brown GW, Harris T. The social origins of depression. London: Tavistock Publications; 1978.
- Perris C, Holmgren S, von Knorring L, Perris H. Parental loss by death in the early childhood of depressed patients and of their healthy siblings. Br J Psychiatry 1986;148:165-9.
- Roy A. Early parental separation and adult depression. Arch Gen Psychiatry 1985;42:987-91.
- Breier A, Kelsoe JR Jr, Kirwin PD, Beller SA, Wolkowitz OM, Pickar D. Early parental loss and development of adult psychopathology. Arch Gen Psychiatry 1988;45:987-93.
- Mireault GC, Bond LA. Parental death in childhood: perceived vulnerability, and adult depression and anxiety. Am J Orthopsychiatry 1992;62:517-24.
- Rutter M, Taylor EA, Hersov LA. Child and adolescent psychiatry: modern approaches. 3rd ed. Oxford: Blackwell Science; 1995.
- Gilman SE, Kawachi I, Fitzmaurice GM, Buka SL. Family disruption in childhood and risk of adult depression. Am J Psychiatry 2003;160:939- 46.
- Klein DN, Arnow BA, Barkin JL, Dowling F, Kocsis JH, Leon AC, et al. Early adversity in chronic depression: clinical correlates and response to pharmacotherapy. Depress Anxiety 2009;26:701-10.