East Asian Arch Psychiatry 2016;26:137-40
THEME PAPER
Dr Kit-i Che, MBChB, FHKCPsych, FHKAM (Psychiatry), Psychiatric Outpatient Department, Alice Ho Miu Ling Nethersole Hospital, Hong Kong SAR, China.
Address for correspondence: Dr Kit-i Che, Psychiatric Outpatient Department, Alice Ho Miu Ling Nethersole Hospital, Tai Po, New Territories, Hong Kong SAR, China.
Email: cki537@ha.org.hk
Submitted: 3 July 2016; Accepted: 18 July 2016
Abstract
A 12-year-old girl presented to the mental health service for an abrupt onset of mental changes characterised by hearing voices and being paranoid. She appeared preoccupied and her mood was labile. There was no family history of mental illness, and no organic causes were identified. These symptoms subsided spontaneously in a week. However, she experienced 3 other similar psychotic episodes afterwards which happened in a near-monthly cycle. Her level of functioning was normal between these episodes. Throughout the course of the illness, it was noted that these mental state changes might be related to the menstrual cycle. In this case we discuss the recurrent periodic psychoses in adolescents and the important differential diagnoses to be considered, including menstrual psychosis, a rare and less well-understood clinical entity.
Key words: Adolescent; Psychotic disorders; Recurrence
Introduction
There have been many case reports of adolescents who present with recurrent psychotic episodes — the clinical symptoms range from stupor to psychomotor excitement, and they are usually accompanied by delusions or hallucinations. These episodes usually subside within 2 weeks but are often repeated. It has been observed that there is a tendency for these patients to repeat the same symptoms in a near-monthly cycle. These periodic psychoses of puberty have been reported to occur below the age of 20 years and comprise predominantly affective symptoms and paranoid symptoms.1 These recurrent brief psychotic episodes in adolescents appear to be manifestations of affective illness and may be treated or prevented as such.2
We present a young adolescent girl with periodic psychotic episodes to illustrate the important clinical diagnoses to be considered in these cases.
Case History
A 12-year-old Form 1 girl who lived with her parents and younger brother first presented to mental health services on 24 February 2014 with an abrupt onset of mental state changes preceded by interpersonal conflicts. She complained of hearing voices that asked her not to study at school and not to read messages on her mobile phone. She felt as if people on the streets were staring at her, and she believed her classmates were talking behind her back. She did not sleep well and she appeared to be tired with poor concentration. She became increasingly preoccupied and did not speak a word all day long at school. She felt guilty about reading cartoon pornography on the Internet more than a year ago and believed the police would soon come and catch her. She was also anxious about people knowing that she had previously read pornography. She denied any suicidal ideas. She was brought to the emergency department because of her poor mental state and admitted to the paediatric unit for organic work-up on her mental state changes.
With regard to her medical history, she was born full term by normal spontaneous delivery with no perinatal problems. She had achieved normal developmental milestones and was prescribed no long-term medications. Her age at menarche was 11 years and she had no family history of mental illness.
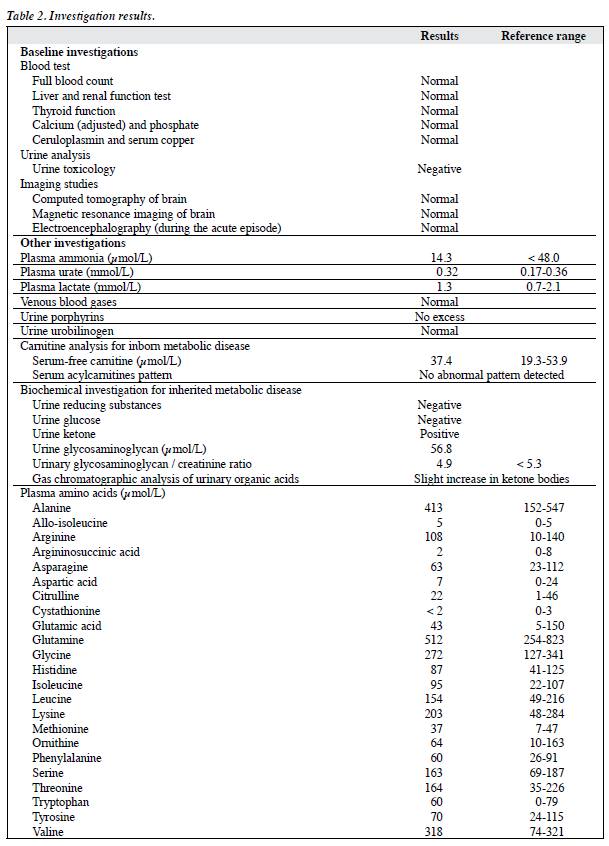
Organic work-up including full blood count, liver and renal function tests, thyroid function test, ceruloplasmin and serum copper levels, urine toxicology, computed tomographic scan of the brain, and electroencephalography were all unremarkable.
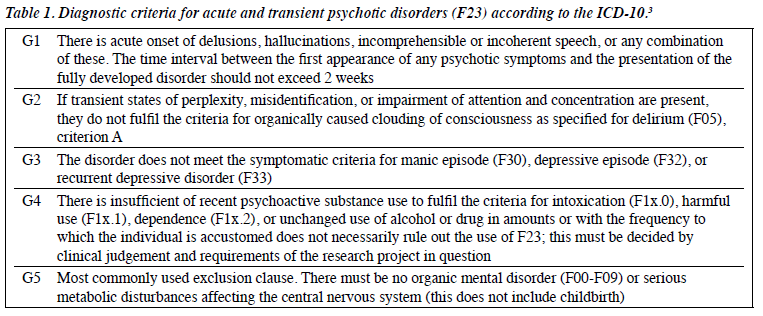
Her mental state improved gradually after admission. By the time she was seen by psychiatrist, which was about a week after her onset of mental state changes, all psychotic symptoms had subsided without any psychiatric treatment. The provisional psychiatric diagnosis was acute and transient psychotic disorder according to the ICD-10 criteria. Details of the diagnostic criteria are shown in Table 1.3 She was not prescribed any medication at that time and an outpatient psychiatric appointment was arranged to monitor her mental state following discharge.
She resumed school regularly after the first episode of psychosis. Her mental state deteriorated suddenly again on 14 March 2014, about 3 weeks after the first episode. She presented with similar symptomatology characterised by increased perplexity, not responding to others, and feeling guilty about having watched pornography before. Again she firmly believed that people around her, even strangers, knew that she had read pornography. Symptoms subsided spontaneously after a week, approximately 2 days after commencement of risperidone 0.5 mg/day.
The third episode started on 12 April 2014 after she was terrified by witnessing a classmate having a convulsion while on a school trip. She had a similar presentation that included perplexity, irrelevant speech, poor sleep, and a reduced oral intake since she believed the water to be poisonous. She also refused medication as she believed the drug resulted in abnormal hair growth on her arms (physical examination excluded any such abnormal hair growth). She returned to her pre-morbid mental state after a week and risperidone was increased to 1 mg/day.
The fourth episode started on 11 May 2014 with no apparent stressor. She presented with sudden onset of perplexity and ideas of reference. Symptoms subsided after a week. A paediatrician was consulted about the need for any further organic work-up. Magnetic resonance imaging of the brain was arranged and the paediatrician suggested metabolic screening tests be done during the acute phase of mental state changes in the future. Risperidone was increased to 1.5 mg/day. It was noted that the patient started menstruation soon after admission. Unfortunately, there was a lack of information about previous menstrual cycles so any connection with onset of these psychotic episodes could not be determined.
In summary, the patient presented to the mental health service at the age of 12 years. She experienced 4 brief psychotic episodes from which she made a complete recovery after a week. These episodes happened in a near- monthly cycle. Her level of functioning was normal in between. She had no family history of mental illness. Acute infections, metabolic disorders, and intoxication were excluded. Results of the investigations are summarised in Table 2. Her last psychotic episode was in May 2014, and she has been maintained on risperidone 1.5 mg/day since then with stable mental state.
Discussion
Recurrent episodes of psychotic features in adolescents have been the subject of clinical discussion for decades. Different cases have been reported worldwide in Germany, America, and Japan.1,2,4-6
Important clinical differential diagnoses include metabolic disorders, especially in patients who present with periodic changes to mental state. Hereditary metabolic disorders (HMD) are rare but important causes of psychiatric disorders among adolescents and these include Wilson’s disease, remethylation disorders, and porphyria.7 Some HMD can elicit psychiatric signs years before other more specific organic signs appear.8 The diagnosis of the disease at the ‘psychiatric’ stage corresponds to a relatively early physical / organic phase when timely treatment can help prevent the occurrence of irreversible outcomes.9 Although HMD that present purely with psychiatric symptoms are very difficult to diagnose, it is important for psychiatrists to be aware of these possible differential diagnoses.
Another rare but clinically important differential diagnosis, especially in girls who present with mental state changes on a near-monthly basis, is menstrual psychosis. The connection between menstruation and psychological disorder was first observed in the 18th century although this concept was not universally accepted and there remains scepticism about such a diagnosis.10 Menstrual psychosis has the following characteristics: (1) acute onset against a background of normality, (2) brief duration with fully recovery, (3) psychotic features: confusion, delusions, hallucinations, stupor, mutism, or a manic syndrome, and (4) a circa-menstrual (approximately monthly) periodicity, in rhythm with the menstrual cycle.10 The key to diagnosis is identification of the periodic recurrent psychotic episodes in relation to menstrual cycle. It requires accurate dating of both the menstrual period and the onset of the psychotic episode for at least several episodes in order to establish the connection. This explains why, among the case reports worldwide, there are only about 80 cases with substantial evidence of a diagnosis of menstrual psychosis while more than 200 reported cases can only be accepted as ‘possible’ cases.11
The description of clinical symptoms in case reports of menstrual psychosis are also compatible with bipolar disorder, and it has been suggested that menstrual psychosis belongs to the family of manic depressive psychosis with menstruation as one of the triggers for the bipolar episodes. Indeed, psychotic symptoms are common in prepubertal major depressive disorder and adolescent mania.12,13 There are also case reports of manic depressive disorder showing a near-monthly rhythm of recurrence. It is therefore suggested that both psychotic features and near-monthly rhythms could be characteristics manifested by some adolescents with affective disorder.
Taking into account of all these, although the clinical symptoms described in this case are compatible with the diagnosis of acute and transient psychotic disorders, given the variable presentations of psychiatric symptoms in adolescents, longitudinal observations on the course of the illness would be of paramount importance.
Declaration
The author has disclosed no conflicts of interest.
References
- Abe K, Ohta M. Periodic psychosis of puberty: a review on near- monthly episodes. Psychopathology 1992;25:218-28.
- Abe K, Ohta M. Recurrent brief episodes with psychotic features in adolescence: periodic psychosis of puberty revisited. Psychiatry Clin Neurosci 1998;52 Suppl:S313-6.
- World Health Organization. International Classification of Diseases ICD-10 Version:2015. Available from: http://apps.who.int/ classifications/icd10/browse/2015/en. Accessed 1 Jul 2016.
- Altschule MD, Brem J. Periodic psychosis of puberty. Am J Psychiatry 1963;119:1176-8.
- Grünewald BD, Korte A, Schulte-Körne G. Psychotic episodes during menstruation in a 12-year-old girl: a case of menstrual psychosis. Eur Child Adolesc Psychiatry 2012;21:173-5.
- Teja JS. Periodic psychosis of puberty. A longitudinal case study. J Nerv Ment Dis 1976;162:52-7.
- Stein D, Blumensohn R, Witztum E. Perimenstrual psychosis among female adolescents: two case reports and an update of the literature. Int J Psychiatry Med 2003;33:169-79.
- Sedel F, Baumann N, Turpin JC, Lyon-Caen O, Saudubray JM, Cohen D. Psychiatric manifestations revealing inborn errors of metabolism in adolescents and adults. J Inherit Metab Dis 2007;30:631-41.
- Demily C, Sedel F. Psychiatric manifestations of treatable hereditary metabolic disorders in adults. Ann Gen Psychiatry 2014;13:27.
- Brockington I. Menstrual psychosis. World Psychiatry 2005;4:9- 17.
- Brockington IF. Menstrual psychosis: a bipolar disorder with a link to the hypothalamus. Curr Psychiatry Rep 2011;13:193-7.
- Ballenger JC, Reus VI, Post RM. The “atypical” clinical picture of adolescent mania. Am J Psychiatry 1982;139:602-6.
- Chambers WJ, Puig-Antich J, Tabrizi MA, Davies M. Psychotic symptoms in prepubertal major depressive disorder. Arch Gen Psychiatry 1982;39:921-7.