East Asian Arch Psychiatry 2015;25:159-163
ORIGINAL ARTICLE
Prof. M. S. Bhatia, MD, Department of Psychiatry, University College of Medical Sciences & GTB Hospital, Dilshad Garden, Delhi, India.
Dr Shruti Srivastava, DNB, Department of Psychiatry, University College of Medical Sciences & GTB Hospital, Dilshad Garden, Delhi, India.
Dr Priyanka Gautam, MD, Department of Psychiatry, University College of Medical Sciences & GTB Hospital, Dilshad Garden, Delhi, India.
Dr Rashmita Saha, MD, Department of Psychiatry, University College of Medical Sciences & GTB Hospital, Dilshad Garden, Delhi, India.
Dr Jaswinder Kaur, MD, Department of Psychiatry, University College of Medical Sciences & GTB Hospital, Dilshad Garden, Delhi, India.
Address for correspondence: Prof. M. S. Bhatia, D-1, Naraina Vihar, New Delhi 110028, India.
Tel: 09810161790; Fax: 0091-11-22590595; Email: manbhatia1@rediffmail.com
Submitted: 2 July 2015; Accepted: 21 September 2015
Abstract
Objective: Intellectual disability in a child places great stress on a family and caregiver and this leads to significant socio-occupational dysfunction and impaired quality of life for caregivers. This study aimed to assess socio-demographic characteristics, burden, and psychiatric morbidity of the caregivers of persons with intellectual disability, as well as to determine the variables that correlated with burden and psychiatric morbidity.
Methods: An observational study was carried out in an outpatient psychiatric unit of a tertiary care teaching hospital in India from October 2014 to April 2015. A total of 100 caregivers of intellectually impaired individuals were assessed for burden and psychiatric morbidity.
Results: In all, 39% of the caregivers had a high burden score, 46% perceived mild-to-moderate burden severity, and 15% perceived no to mild burden. Mild-to-moderate depressive symptoms were present in 23% and 16% had severe–to–extremely severe depressive symptoms. Mild-to-moderate anxiety symptoms were evident in 19% of caregivers and a further 19% had severe–to–extremely severe anxiety symptoms.
Conclusion: Routine assessment of burden and psychiatric morbidity in the caregiver will help to reduce their burden and thus help them care for their children more appropriately and efficiently.
Key words: Caregivers / psychology; Intellectual disability; Mental disorders
Introduction
Intellectual disability is defined as a neurodevelopmental disorder characterised by deficits in intellectual and adaptive functioning that present before 18 years of age.1 Aetiology of intellectual disability is heterogeneous and encompasses a broad spectrum of functioning, disability, needs, and strengths. The term replaces the older term of “mental retardation”. Intellectual disability involves impairment of general mental abilities that impact adaptive functioning in 3 domains, namely conceptual, social and practical, that in turn determine individual capacity to cope with everyday tasks.1 Intellectual disability is a highly prevalent and highly disabling condition. It is generally considered that 2% of the Indian population constitutes persons with intellectual disability and its prevalence varies from 0.22 to 32.7 per 1000.2
The disorder is considered chronic and often co- exists with other mental conditions such as depression,3 attention-deficit / hyperactivity disorder,4 and autism spectrum disorder.4,5 They can also develop any other kind of neuropsychiatric disorder similar to the general population.6-9 The frequency and type of psychiatric or behavioural disorder vary according to the severity of intellectual disability, as well as a variety of other conditions, including medical problems, environmental changes, and life circumstances.9 Studies reveal that around 19% of the severely retarded and 4% of the mildly retarded also manifest epilepsy.7 Defects in movement and hearing are most prominent among the mildly retarded, while the frequency of specific speech disturbances is greater among the severely retarded.7 Visual defects have also been observed in about a third of these patients.7
Intellectual disability in a child is a stress for the family and caregiver and disability assessment studies have shown that mental retardation and other disorders lead to significant socio-occupational dysfunction and impaired quality of life for caregivers.10 Previous study has revealed that parental application for placement of children with severe impairment was significantly related to high parental
In earlier studies, the mean burden was minimal to moderate in all families with children with intellectual disability. Children suffering from intellectual disability are considered a burden by their family members. Negative parental attitude leads to rejection of intellectually impaired children. This adversely affects interaction within the family. Such children should be offered support by family members to enable them to cope with stressful situations and in their rehabilitation.12,13
To date, studies report that stress is related to the severity of intellectual disability, being maximum in those with severe-to-profound retardation. Among parents, mothers perceive more stress and burden in caring for their disabled children than fathers.14 These studies also revealed that caregivers of intellectually disabled individuals face various kinds of challenges, such as psychological, social, and economic challenges due to poverty. Caregivers living with persons who have intellectual disability feel stressed and burdened. They also feel sadness for a multitude of reasons including the task of giving care, worries about the future life of their children, and the disturbing behaviour of their children. In addition, they are stressed because of inadequate social services for their children and the stigma attached to mental illness.12-14
Stigma is an important issue to be addressed in cases of intellectual disability. Only few studies have specifically focused on this issue rather than mental illness. In earlier studies, overall attitude to those with intellectual disability was relatively positive although social contact was viewed with ambivalence. Stigma associated with intellectual disability is present across all ethnic groups, although it appears to be increased among those from developing countries.15,16
These caregivers can suffer psychiatric illness because of their burden or stress, and this can further complicate their situation. The strong impact and negative consequences of burden and stress on caregivers result in a reduction in their caregiving ability, whereas subjective gains and satisfaction may enhance this ability.17 The present study was planned to assess the burden and psychiatric morbidity among caregivers of patients diagnosed with intellectual disability and to determine their correlates.
Study Objectives
This study aimed to: (1) assess socio-demographic characteristics of the caregivers of persons with intellectual disability; (2) assess the burden on caregivers of persons with intellectual disability; (3) assess the psychiatric morbidity of caregivers of intellectually disabled persons; and (4) determine the variables that correlated with burden and psychiatric morbidity.
Methods
This was an observational study carried out in an outpatient psychiatric unit of a tertiary care teaching hospital in the capital city of India from October 2014 to April 2015. Caregivers of all the intellectually disabled individuals, who gave written informed consent, were assessed after establishment of diagnosis of intellectual disability by clinical psychologists using appropriate tests. Tests used for assessment of intelligence quotient (IQ) included the Wechsler Adult Intelligence Scale, Wechsler Intelligence Scale for Children, Stanford-Binet Intelligence Scale, and Vineland Social Maturity Scale.
Caregivers who were living with children of intellectual disability, aged > 18 years, and gave informed consent were included in this study. Those who were critically ill or suffering from any psychotic illness and who withheld informed consent were excluded.
Tools for the Study
Socio-demographic data were recorded using a semi- structured performa. Caregiver burden was measured using the Zarit Burden Interview, a popular caregiver self- reported measure that contains 22 items.18,19 Each item is scored on a 5-point scale with response options scored from 0 to 4. Hébert et al19 showed that this interview has good internal consistency and reliability, with a Cronbach’s alpha coefficient of 0.92.
For the assessment of psychiatric symptoms, Depression Anxiety Stress Scale (DASS) was used.20,21 It is a 42-item self-reported inventory that yields data for 3 factors: depression, anxiety, and stress. Reliability of the 3 scales is considered good and test-retest reliability is considered adequate with 0.71 for depression, 0.79 for anxiety, and 0.81 for stress.20
Severity of intellectual disability was recorded as per the ICD-10 guidelines.22 Co-morbidities in the individuals were recorded on the basis of clinical evaluation and laboratory assessment. Appropriate steps were taken to manage any disorders or co-morbidities identified in the individuals and the caregivers.
Socio-demographic variables were compared with Zarit Burden Interview scores and DASS scores. Categorical variables were compared using analysis of variance (ANOVA) and continuous variables correlated using Pearson correlation. Pearson correlation analysis was also used to correlate Zarit Burden Interview score with DASS scores. All the measures were computed using the Statistical Package for the Social Sciences Windows version 21 (SPSS Inc., Chicago [IL], US).
Results
A total of 100 individuals were recruited to the study. Socio-demographic characteristics revealed that 62% of caregivers were female and 38% were male. The mean age of caregivers was 39.40 years. Most caregivers (92%) were married. Besides, 32% of the caregivers were illiterate, 24% studied up to primary school level, 10% up to middle school level, 22% up to high school level, 7% attained intermediate education, and 5% were graduates. Most caregivers were housewives (40%); 43% were semi-skilled or skilled workers, 6% were unskilled workers, 4% were professionals, and 7% were unemployed. Most caregivers (88%) were a parent of the intellectually disabled individual, 2% were a spouse, and 7% were a sibling. Besides, 81% of the caregivers were from an urban area and most belonged to the nuclear family (72%). The mean monthly family income was US$122.25.
Socio-demographic characteristics of the intellectually disabled individuals revealed that most were male (70%) with a mean age of 14.66 years. Most of them were unmarried (99%) and unemployed (98%), and 81% were from an urban area. Most individuals (36%) belonged to the category of moderate mental retardation: 31% were mildly retarded and another 31% had severe retardation, 2% were profoundly retarded. The mean (± standard deviation [SD]) IQ was 41.2 ± 13.3.
The Zarit Burden Interview and DASS scores in caregivers are shown in Table 1. The mean (± SD) Zarit Burden Interview score was 39.33 ± 17.86, whereas the mean DASS depression subscale score being 10.05 ± 10.51, anxiety subscale score being 7.94 ± 8.78, and stress subscale score being 11.77 ± 10.34.
Table 2 shows the burden and clinical symptom severity assessments of caregivers based on the Zarit Burden Interview and DASS, respectively. Burden analysis showed that 39% of the caregivers had a high burden score, 46% perceived a mild-to-moderate burden severity, and 15% perceived no to mild burden. Analysis of DASS scores revealed that 61% had no depressive symptoms, 23% had mild-to-moderate depressive symptoms, and 16% had severe–to–extremely severe depressive symptoms. Anxiety subscale assessment showed that 62% had no anxiety disorder, 19% had mild-to-moderate anxiety symptoms, and another 19% had severe–to–extremely severe anxiety symptoms.
Socio-demographic variables of caregivers were compared with Zarit Burden Interview score and DASS scores. Analysis of categorical variables using ANOVA did not reveal any significant difference except for gender. Female caregivers experienced more burden (44.35 ± 16.35) compared with males (31.13 ± 17.35) and this difference was statistically significant (F = 14.705, p < 0.001). Similarly female caregivers suffered significantly more depression (F = 4.634, p = 0.03), anxiety (F = 7.744, p = 0.01), and stress (F = 3.945, p = 0.05).
Table 3 shows Pearson correlation analysis between various continuous socio-demographic variables of the caregivers and intellectually disabled individuals with DASS scores and Zarit Burden Interview scores. Bivariate analysis of socio-demographic variables did not reveal any statistically significant difference in study variables across different categories but on Pearson correlation, increasing age of the caregiver was positively correlated with increasing DASS depression (r = 0.248, p = 0.01) and stress (r = 0.227, p = 0.02) subscale scores, as well as increasing Zarit Burden Interview score (r = 0.211, p = 0.04). A significant negative correlation was also found for family income with DASS anxiety subscale score (r = –0.267, p = 0.01). Age of the intellectually disabled individual was also significantly correlated with DASS anxiety subscale score (r = 0.232, p = 0.02). Intelligence quotient was negatively correlated with Zarit Burden Interview score (r = –0.109, p = 0.28) and all 3 subscales of DASS including depression (r = –0.102, p = 0.31), anxiety (r = –0.006, p = 0.95), and stress (r = –0.113, p = 0.26). This means that the perceived burden and DASS scores increased with decreasing IQ or increasing severity of mental retardation, though this correlation was not statistically significant.
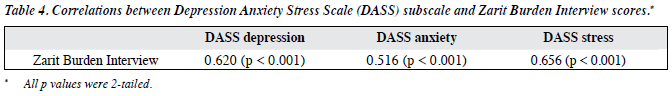
Table 4 shows that Zarit Burden Interview score was significantly and positively correlated with all 3 DASS subscale scores of depression (r = 0.620, p < 0.001), anxiety (r = 0.516, p < 0.001), and stress (r = 0.656, p < 0.001).
Discussion
This study revealed that caregivers of people with intellectual disability perceived a significant burden and suffered psychiatric morbidities in the form of depressive and anxiety disorders. Results revealed that 46% experienced at least a mild-to-moderate level of burden. Earlier studies have also revealed that a significant burden is perceived by the caregivers of intellectually impaired individuals.12,13,23
Gender plays an important role: female caregivers experience more burden and psychiatric morbidity. In a study of stress in parents of intellectually challenged, Upadhyaya and Havalappanavar24 evaluated fathers and mothers separately and found that the mothers experienced higher stress than the fathers. When different areas of stress were considered, mothers were more stressed compared with fathers in daily care, emotions and social stress. There was no difference in the degree of financial stress.24
Caregiver burden was positively and significantly correlated with the age of the caregiver and presence of psychiatric morbidity. Burden was negatively correlated with family income as well as the age and IQ of the patient, though not statistically significant. This means that the burden perceived by caregivers decreases with financial support, increasing age of the intellectually disabled individual, and decreasing severity of the intellectual disability. Earlier studies also revealed that this burden is predicted by the presence of psychiatric morbidity in the caregiver, as well as the level of functioning and education level of the child.14,23 Studies related to the functional disability and burden show that disability in participation in society and personal care are the main areas that contribute to higher family burden.25
Apart from burden, we addressed the psychiatric morbidity of caregivers. They are at high risk of developing psychiatric disorders, as they suffer from multiple constraints such as financial problems, social ostracism, and psychological trauma. There is evidence that children with mental health problems are more likely to have mothers who screen positive for a mental illness.26 We found that 35% to 39% of caregivers suffered depression, anxiety, and stress. The scores for severity of these disorders were directly and significantly correlated with the burden experienced by the caregivers.
There are studies showing that psychiatric morbidity among caregivers of children and adolescents with neuropsychiatric disorders in general is very high, with burden of care being the most important factor responsible.27
There are very few studies that evaluate the factors associated with psychiatric co-morbidity in caregivers of intellectually disabled children. In these caregivers, factors associated with psychiatric morbidity include the child’s level of functioning as assessed by the clinician, the child’s high degree of impairment as assessed by the caregiver, and the high level of caregiver burden. Caregiver burden was found to be the strongest predictor of psychiatric morbidity among caregivers.28 Although this study did not consider all perspectives related to the burden, such as social and cultural, and screening tools to measure psychiatric morbidity as well as definitive diagnostic tools were lacking, it provides an insight into the sufferings of caregivers and their mental health. Parents are major contributors to the development of their children. We need to address the burden and psychiatric co-morbidity in caregivers to enhance their caregiving ability. There are various psychological measures with proven efficacy that can be directed at caregivers to improve their coping ability. Parent training and education about the nature of disabilities in their children, behavioural problems, and future requirements can help increase their coping mechanisms to manage this chronic stress.29,30
Conclusion
The present findings have practical implications for assessing the health needs of those who are involved in the process of giving care to intellectually disabled children. We must understand that as a developing country with limited resources it is not possible to develop positive health in individuals with intellectual disability if their caregivers are overburdened and suffering from psychiatric illness. Routine assessment of burden and psychiatric morbidity in the caregiver will help to reduce their burden. Addressing these issues will help them cope with the challenges and care for their children more appropriately and efficiently.
References
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed. Washington DC: American Psychiatric Association; 2013.
- ICMR. In: Madhavan T, Kalyan M, Naidu S, Peshwaria R, Narayan J, editors. Mental retardation: A manual for psychologists. National Institute for the Mentally Handicapped (under the Ministry of Social Justice and Empowerment, Government of India), Andhra Pradesh, India; 1983.
- Janowsky DS, Davis JM. Diagnosis and treatment of depression in patients with mental retardation. Curr Psychiatry Rep 2005;7:421-8.
- Lindblad I, Gillberg C, Fernell E. ADHD and other associated developmental problems in children with mild mental retardation. The use of the “Five-To-Fifteen” questionnaire in a population-based sample. Res Dev Disabil 2011;32:2805-9.
- Nordin V, Gillberg C. Autism spectrum disorders in children with physical or mental disability or both. II: Screening aspects. Dev Med Child Neurol 1996;38:314-24.
- Khess CR, Dutta I, Chakrabarty I, Bhattacharya P, Das J, Kothari S. Comorbidity in children with mental retardation. Indian J Psychiatry 1998;40:289-94.
- Göstason R. Psychiatric illness among the mentally retarded. A Swedish population study. Acta Psychiatr Scand Suppl 1985;318:1- 117.
- Silka VR, Hauser MJ. Psychiatric assessment of the person with mental retardation. Psychiatr Ann 1997;27:162-9.
- Hauser MJ. The role of the psychiatrist in mental retardation. Psychiatr Ann 1997;27:170-4.
- Malhotra S, Khan W, Bhatia MS. Quality of life of parents having children with developmental disabilities. Delhi Psychiatry J 2012;15:171-6.
- Embar P. Workshop for the parents of the mentally retarded. Indian J Ment Retard 1969;2:21-5.
- Kaur R, Arora H. Attitudes of family members towards mentally handicapped children and family burden. Delhi Psychiatry J 2010;13:70-4.
- Ambikile JS, Outwater A. Challenges of caring for children with mental disorders: Experiences and views of caregivers attending the outpatient clinic at Muhimbili National Hospital, Dar es Salaam — Tanzania. Child Adolesc Psychiatry Ment Health 2012;6:16.
- Sethi S, Bhargava SC, Dhiman V. Study of level of stress and burden in the caregivers of children with mental retardation. East J Med 2007;12:21-4.
- Ditchman N, Werner S, Kosyluk K, Jones N, Elg B, Corrigan PW. Stigma and intellectual disability: potential application of mental illness research. Rehabil Psychol 2013;58:206-16.
- Scior K, Addai-Davis J, Kenyon M, Sheridan JC. Stigma, public awareness about intellectual disability and attitudes to inclusion among different ethnic groups. J Intellect Disabil Res 2013;57:1014-26.
- Singh K, Kumar R, Sharma N, Nehra DK. Study of burden in parents of children with mental retardation. J Indian Health Psychol 2014;8:13- 20.
- Zarit SH, Reever KE, Bach-Peterson J. Relatives of the impaired elderly: correlates of feelings of burden. Gerontologist 1980;20:649- 55.
- Hébert R, Bravo G, Préville M. Reliability, validity, and reference values of the Zarit Burden Interview for assessing informal caregivers of community-dwelling older persons with dementia. Can J Aging 2000;19:494-507.
- Lovibond PF. Long-term stability of depression, anxiety, and stress syndromes. J Abnorm Psychol 1998;107:520-6.
- Brown TA, Chorpita BF, Korotitsch W, Barlow DH. Psychometric properties of the Depression Anxiety Stress Scales (DASS) in clinical samples. Behav Res Ther 1997;35:79-89.
- World Health Organization. International Classification of Diseases, Clinical Description and Diagnostic Guidelines. 10th ed. Geneva: WHO; 1992.
- Dada MU, Okewole NO, Ogun OC, Bello-Mojeed MA. Factors associated with caregiver burden in a child and adolescent psychiatric facility in Lagos, Nigeria: a descriptive cross sectional study. BMC Pediatrics 2011;11:110.
- Upadhyaya GR, Havalappanavar NB. Stress in parents of mentally challenged. J Indian Acad Appl Psychol 2008;34:53-9.
- Irazábal M, Marsà F, García M, Gutiérrez-Recacha P, Martorell A, Salvador-Carulla L, et al. Family burden related to clinical and functional variables of people with intellectual disability with and without a mental disorder. Res Dev Disabil 2012;33:796-803.
- Grupp-Phelan J, Wade TJ, Pickup T, Ho ML, Lucas CP, Brewer DE, et al. Mental health problems in children and caregivers in the emergency department setting. J Dev Behav Pediatr 2007;28:16-21.
- Okewole A, Dada MU, Ogun O, Bello-Mojeed M, Usoh T. Prevalence and correlates of psychiatric morbidity among caregivers of children and adolescents with neuropsychiatric disorders in Nigeria. Afr J Psychiatry (Johannesbg) 2011;14:306-9.
- Gallagher S, Phillips AC, Oliver C, Carroll D. Predictors of psychological morbidity in parents of children with intellectual disabilities. J Pediatr Psychol 2008;33:1129-36.
- Akkok F. An overview of parent training and counselling with the parents of children with mental disabilities and autism in Turkey. Int J Adv Counsel 1994;17:129-38.
- Karayanni M. Counseling parents with a Down’s syndrome child. Int J Adv Counsel 1989;12:153-64.