East Asian Arch Psychiatry 2019;29:103-11 | https://doi.org/10.12809/eaap1832
ORIGINAL ARTICLE 
Simon KH Hon, MBBS, FHKCPsych, FHKAM (Psychiatry), Department of General Adult Psychiatry, Castle Peak Hospital, Hong Kong SAR, China Bonnie WM Siu, MBChB, MRCPsych (UK), FHKCPsych, FHKAM (Psychiatry), FRCPsych (UK), Department of Forensic Psychiatry, Castle Peak Hospital, Hong Kong SAR, China
CW Cheng, MBBS, FHKCPsych, FHKAM (Psychiatry), Department of General Adult Psychiatry, Castle Peak Hospital, Hong Kong SAR, China
Wilson CW Wong, MBChB, FHKCPsych, FHKAM (Psychiatry), Department of General Adult Psychiatry, Castle Peak Hospital, NT, Hong Kong SAR, China Edna B Foa, PhD, University of Pennsylvania Perelman School of Medicine, Philadelphia, USA
Address for correspondence: Dr Simon KH Hon, 15 Tsing Chung Koon Road, Tuen Mun, Hong Kong SAR, China.
Email: honkinghim@yahoo.com
Submitted: 4 April 2018; Accepted: 12 October 2018
Abstract
Background: The Obsessive-Compulsive Inventory-Revised (OCI-R) is a psychometrically sound and valid self-report measure for evaluating the severity of six dimensions of obsessive-compulsive symptoms: washing, obsessing, hoarding, ordering, checking, and neutralising. We aimed to validate the Chinese version of the OCI-R (C-OCI-R) in patients with obsessive-compulsive disorder (OCD) in Hong Kong.
Methods: The C-OCI-R was forward and backward translated and reviewed by an expert panel and a focus group. The internal consistency and test-retest reliability (2-week interval) were examined. Confirmatory factor analysis was used to examine the construct validity of the C-OCI-R. Concurrent validity was examined by the correlation between the C-OCI-R and the Yale-Brown Obsessive-Compulsive Scale (Y-BOCS), whereas divergent validity was examined by the correlation of the C-OCI-R with the Beck Depression Inventory-Second Edition and the Hamilton Depression Rating Scale.
Results: 130 OCD patients were recruited. The C-OCI-R showed excellent internal consistency (Cronbach’s alpha = 0.92) and test-retest reliability (Spearman’s rho correlation coefficient = 0.96). The original six-factor model was supported by confirmatory factor analysis. Concurrent validity and divergent validity were established. However, the neutralising subscale may need further development, and the divergent validity of the obsessing subscale was unsatisfactory. The structure of OCD symptoms was similar in Chinese and western patients.
Conclusion: The C-OCI-R is a valid and reliable measure for assessing the severity of obsessive- compulsive symptoms in local Chinese patients with OCD.
Key words: Obsessive-compulsive disorder; Validation studies
Introduction
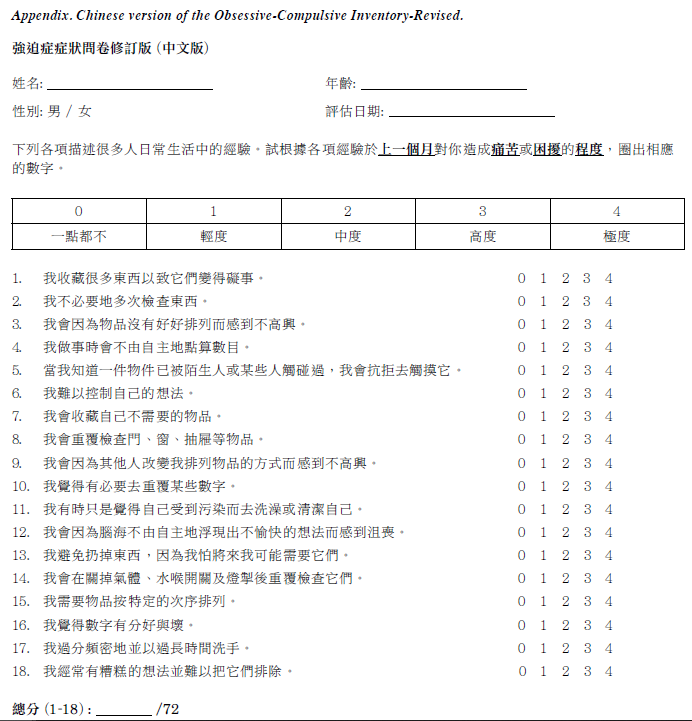
Obsessive-compulsive disorder (OCD) is characterised by ego-dystonic obsessions and compulsions. Among United States adults, the 12-month prevalence of OCD was 1.2%.1 In Hong Kong, the only large-scale community survey was conducted in the 1980s and reported a lifetime prevalence of OCD of 1%.2 Self-report instruments for comprehensive measurement of the heterogeneous clinical picture of OCD have been developed for disease screening, assessment of symptom severity, and monitoring of treatment progress. In particular, the Obsessive-Compulsive Inventory-Revised (OCI-R) is brief, time-efficient, and has good psychometric properties. It is the most translated questionnaire of similar type and is reliable and valid for self-measuring OCD severity across different cultures.3 The OCI-R comprises 18 items in six subscales (three each), including washing, obsessing, hoarding, ordering, checking, and neutralising. It assesses the associated distress of each item in the past month on a 5-point Likert scale from ‘not at all’ (0) to ‘extremely’ (4). The total score ranges from 0 to 72 and the subscale scores from 0 to 12. It takes about 5 minutes to complete. The OCI-R has good psychometric properties in a mixed clinical and non-clinical sample.4 It has a stable six-factor structure and has high internal consistency (r = 0.81-0.93), good to excellent test-retest reliability (r =0.57-0.91), and good convergent validity (r = 0.53) with the Yale-Brown Obsessive-Compulsive Scale (Y-BOCS).4
The reliability and validity of the OCI-R subscales and the sensitivity of the OCI-R in measuring treatment effects have also been reported.5,6 In a receiver operating characteristic curve analysis for the OCI-R, the optimal cut-off score was 21 for distinguishing patients with OCD from non- patients (65.6% sensitivity and 63.4% specificity) and 18 for distinguishing patients with OCD from anxious controls (74.0% sensitivity and 75.2% specificity).4 Replication of studies across different cultures requires standardised and validated tools. Although the OCI-R has been translated into Mandarin-Chinese in mainland China, the validity and reliability of the translated version was undermined because the sample was mostly students and few patients with OCD and only data of the students were used for factor analyses,7,8 and therefore the clinical diagnoses of patients were not confirmed.8 The present study aimed to develop and validate another Chinese version of the OCI-R (C-OCI- R) in a sample of patients with OCD in Hong Kong.
Methods
The study was approved by the New Territories West Cluster Research Ethics Committee (NTWC/CREC/15069). Written informed consent was obtained from each patient before the assessment. Between 1 November 2015 and 31 March 2016, 290 patients were diagnosed as having OCD at the General Adult Psychiatry Clinic of the Tuen Mun Mental Health Centre. The centre provides psychiatric outpatient services to a population of 1.07 million residing in the Tuen Mun and Yuen Long districts of Hong Kong.9 Inclusion criteria were ethnic Chinese aged 18 to 64 years with a principal diagnosis of OCD according to the DSM- IV-TR.10 Exclusion criteria were the presence of current or past schizophrenia spectrum and other psychotic disorders, bipolar and related disorders, neurocognitive disorders, intellectual disabilities, or autism spectrum disorder. Those with OCD as a secondary diagnosis or with a current substance-related disorder or chronic neurological disorder were also excluded.
International guidelines for cross-cultural validation of self-report measures were observed.11 The OCI-R was translated into Chinese separately by a psychiatrist and a translator. The two drafts were compared and discrepancies were resolved through consensus. The C-OCI-R was then back-translated into English by two other psychiatrists who had never seen the original English version. The translator and the fourth psychiatrist compared the original English version and the back-translated version until both versions were comparable in terms of wording, cultural appropriateness, fluency, and clarity. The content validity and cultural relevance of the C-OCI-R was evaluated by an expert panel. In a focus group, the C-OCI-R was well accepted as a rating scale for OCD with satisfactory face validity. The C-OCI-R was pilot tested in five patients with OCD in different sexes, age groups, and education levels. The administrative time was acceptable and there was no problem in understanding the wordings. The final version (appendix) was then used.
Other measurements included the Chinese bilingual version of the Structured Clinical Interview for DSM-IV- TR Axis I Disorders, Research Version, Patient Edition (CB-SCID-I/P),12 the Yale-Brown Obsessive-Compulsive Scale (Y-BOCS),13,14 the Beck Depression Inventory- Second Edition (BDI-II),15 and the Hamilton Depression Rating Scale (HDRS).16
The CB-SCID-I/P has good agreement among raters and between raters and clinicians. The overall kappa value was 0.81 for anxiety disorders, and the inter-rater reliability was 0.87 for psychiatric patients in a multisite study.17-19
The Y-BOCS is a semi-structured, clinician- administered measure that assesses the severity of obsessions and compulsions over the previous week based on patient-provided information and clinical observation.13,14 It contains both a symptom checklist and a 10-item severity scale, which assesses the severity of distress, frequency, interference, resistance, and symptom control, and yields three scores: (1) obsession severity score (range, 0-20), (2) compulsion severity score (range, 0-20), and (3) total score (range, 0-40). The Y-BOCS is considered the gold standard for assessing symptom severity.20 It has good inter- rater reliability (r = 0.80-0.99) and test-retest reliability (r = 0.81-0.97) over a 2-week interval, and acceptable to good internal consistency (Cronbach’s alpha = 0.69-0.91).21
The BDI-II is a 21-item self-report questionnaire for assessing the severity of depressive symptoms over a 2-week period.15 It consists of two dimensions: depressive and physical symptoms. Total scores range from 0 to 63. The Chinese version of the BDI-II has an internal consistency coefficient of 0.94.22
The HDRS is a 17-item clinician-rated scale of depressive symptoms.16 Total scores range from 0 to 50. The Chinese version of the HDRS has excellent inter- rater reliability (r = 0.92) and good internal consistency (Cronbach’s alpha = 0.71).23
The CB-SCID-I/P was performed to ascertain the diagnosis. The Y-BOCS and the HDRS were then administered, followed by the C-OCI-R and the BDI-II to minimise undue influence to the clinician-rated questionnaires. Each interview took approximately 90 minutes. 37 of the participants completed the C-OCI-R 2 weeks later for evaluation of test-retest reliability.
Data were analysed using PASW Statistics (Windows version 18; SPSS Inc, Chicago [IL], US). Confirmatory factor analysis (CFA) was conducted to confirm the latent structure of the C-OCI-R using AMOS software version 19.0. All participants had no more than 5% missing values. Missing value imputation was performed by k-nearest- neighbour imputation using R 3.0.3 (package visualisation and imputation of missing values). The significance level was set at p < 0.05. The normality of data was examined by the Shapiro-Wilk test. Cronbach’s alphas and correlation coefficients were calculated to determine the internal consistency and test-retest reliability of the C-OCI-R. CFA was performed to analyse the interrelationship between items in the C-OCI-R and to explain these in terms of their common underlying components. Goodness-of-fit was evaluated, with normed fit index of ≥ 0.9, goodness of fit index of ≥ 0.9, comparative fit index of ≥ 0.9, and root mean square error of approximation of ≤ 0.08.24 The Y-BOCS was used to calculate concurrent validity as it is considered a gold standard for measuring the severity of OCD symptoms.20 Divergent validity was determined by the correlation of the C-OCI-R with the BDI-II and the HDRS. To avoid underestimation of divergent validity,25 participants with current depressive disorders (n = 17) were excluded, as the correlation between the C-OCI-R and depressive symptoms was invariably higher in patients with depressive disorder.
Results
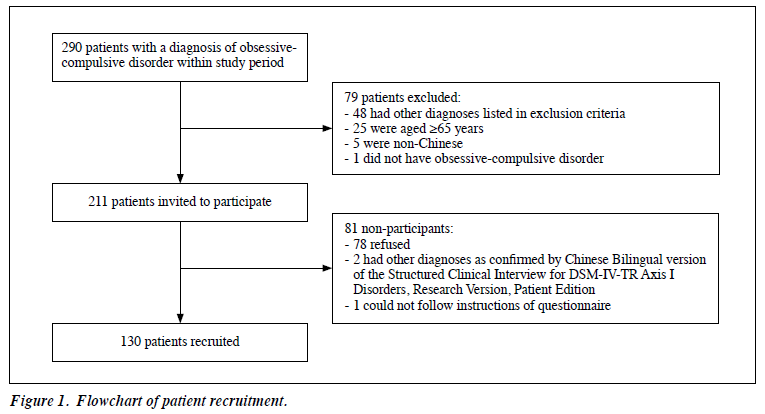
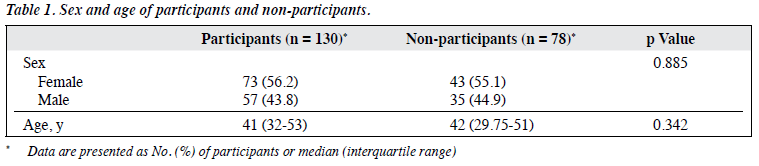
Of the 290 patients, 79 were excluded and 211 were invited to participate (Figure 1). Of the latter, 81 did not and 130 did participate. The participants and non-participants were comparable in terms of sex and age (Table 1). For the 73 female and 57 male participants, the median age was 41 (interquartile range, 32-53) years; the median years of education was 11 (interquartile range, 9-16); the median age of onset of OCD was 20 (interquartile range, 15-30) years; and the median duration of OCD was 15 (interquartile range, 10-27) years. 75 of the participants had psychiatric comorbidities, including current depressive disorder (n = 17), prior depressive disorder currently in remission (n = 55), and anxiety disorder (n = 3).
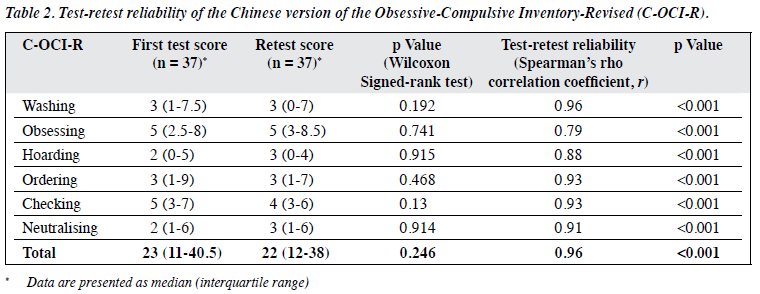
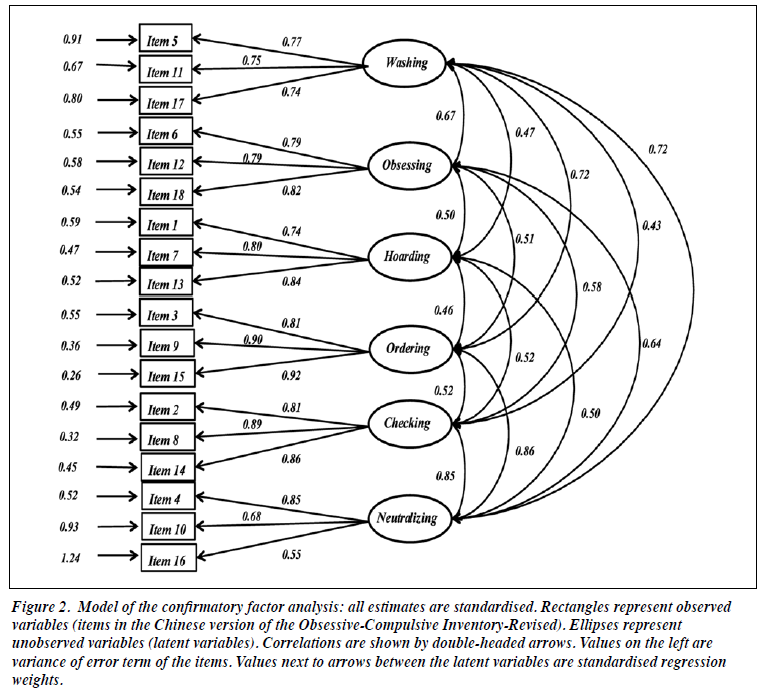
The median C-OCI-R score was 25 (interquartile range, 17-42). The median scores for subscales were 4 for washing, 6 for obsessing, 3 for hoarding, 4 for ordering, 6 for checking, and 3 for neutralising. Internal consistency was excellent (Cronbach’s alpha, 0.92) for the C-OCI-R and good to excellent for subscales of washing (0.79), obsessing (0.84), hoarding (0.83), ordering (0.91), checking (0.89), and neutralising (0.74). Test-retest reliability was excellent (r = 0.96) for C-OCI-R and good to excellent (r = 0.79-0.96) for subscales (Table 2). The six-factor solution showed a normed fit index of 0.89, a goodness of fit index of 0.88, a comparative fit index of 0.96, and a root mean square error of approximation of 0.056. All these indices suggested a good fit of the six-factor structure.26 The standardised factor loadings of the CFA are shown in Figure 2.
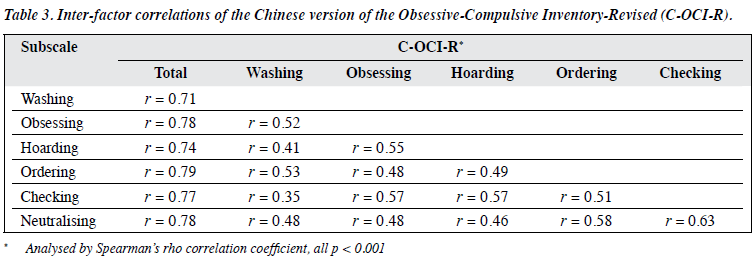
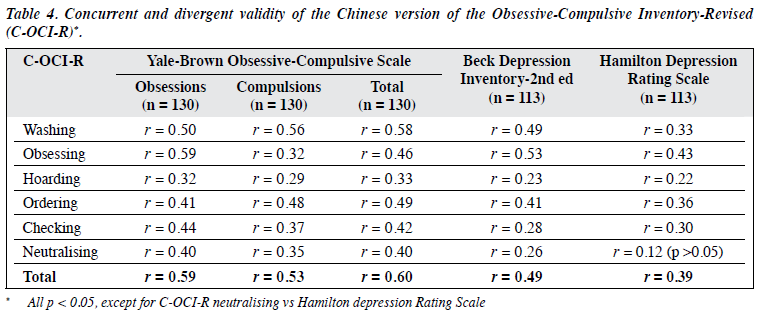
Correlations between the total and subscale scores of C-OCI-R were high (r = 0.71-0.79). However, correlations between the six subscales were low to moderate (r = 0.35- 0.63), indicating that the subscales were related to each other but not redundant (Table 3). Correlation between the C-OCI-R score and the Y-BOCS score was moderate (Spearman’s r = 0.60, p < 0.001). The obsessing subscale of the C-OCI-R showed the highest correlation with the obsession subscale of the Y-BOCS (Spearman’s r = 0.59, p < 0.001), indicating that the C-OCI-R and its obsessing subscale had good concurrent validity (Table 4). Correlation between the C-OCI-R score and the BDI-II score was low (Spearman’s r = 0.49, p < 0.001), as was between the C-OCI-R score and the HDRS score (Spearman’s r = 0.39, p < 0.001). Compared with other subscales, the obsessing subscale of the C-OCI-R had the highest correlation with the BDI-II (Spearman’s r = 0.53, p < 0.001) and the HDRS (Spearman’s r = 0.43, p < 0.001). These results suggested a good divergent validity of the C-OCI-R.
Discussion
Our results confirmed that the C-OCI-R is a reliable and valid tool to assess the severity of OCD symptoms in the local population. CFA confirmed the original six-factor structure.4 The C-OCI-R is a good fit of the original version. The inter-factor correlations of the subscales were low to moderate, whereas the correlations between total and subscale scores were high, indicating that the subscales cover different aspects of OCD while sharing a common theme (OCD symptoms). This confirms the construct validity of the C-OCI-R and the underlying assumption of heterogeneous OCD symptoms belonging to a joint disorder category of OCD. The C-OCI-R demonstrated excellent internal consistency and test-retest reliability. The C-OCI-R is a reliable instrument to measure OCD symptoms.
The neutralising subscale had the lowest internal consistency (Cronbach’s alpha = 0.74), consistent with previous studies.4,5,7,25 The three items of the neutralising subscale are all related to numbers and counting-complaints, and are designed to capture covert neutralising strategies on a superstitious basis. Item 16 (“I feel that there are good and bad numbers”) was criticised during the development stage, as Chinese people commonly think certain number is good (8 is associated with good fortune in Chinese culture) or bad (4 and 7 are associated with death and bad luck, respectively). Such beliefs may be normal in the Chinese context, and endorsement of item 16 may not necessarily indicate the presence of OCD symptom.
Similarly, item 4 (“I feel compelled to count while I am doing things”) may not be exclusive to the rubric of neutralising. It may also be endorsed by OCD patients presented with other symptom subtypes (checking, washing) who simply count how often they have already repeated a particular ritual. In such case, the counting is not motivated by superstitious beliefs, but by a need to define an artificial criterion for action completion (eg, I always have to wash my hands thirty times).27 In fact, numbers and counting-complaints are easily observed in various presentations of OCD, especially in patients with the sense of incompleteness.28 This explains that the inter-factor correlation between neutralising and checking was the highest (r = 0.63) among different subscales.
The relatively low internal consistency of the neutralising subscale can be explained by the fact that the three items seem to tap into different constructs, and that items 4 and 16 are not specific for neutralising strategy. Moreover, these items focus only on numbers and counting but fail to capture other clinically relevant neutralisation phenomena. For example, overt neutralisation by repeating compulsions based on superstitious beliefs, or covert praying rituals to undo blasphemous obsessions. Hence, the relatively low median score in the neutralising subscale may underestimate the actual severity of neutralising symptoms. To further refine the C-OCI-R, removal of items 4 and 16 and addition of other neutralisation strategies unrelated to numbers and counting should be considered.
The median score in the hoarding subscale was also low, consistent with previous studies.4,28-30 This could be due to a low frequency of hoarding in OCD patients31 or weak relevance between hoarding and OCD.32,33 Patients with OCD have no more elevated score in hoarding subscale than non-clinical participants.5 Although the inter- factor correlations between hoarding and other subscales were moderate, the correlations of the C-OCI-R hoarding subscale with the Y-BOCS, BDI-II, and HDRS were consistently lower (r = 0.22-0.33) than other subscales, supporting the assumption that hoarding symptom may be a distinct construct from OCD. Given the adoption of hoarding disorder as a distinctive category from OCD in the latest DSM-5 and the coming International Classification of Diseases 11 Edition, the relationship between the hoarding subscale and the other subscales and its relevance in the C-OCI-R should be further examined.34,35
The C-OCI-R had good concurrent validity. The correlation between the C-OCI-R score and the Y-BOCS score was moderate (r = 0.60), as was correlation between the original OCI-R score and the Y-BOCS score (r = 0.53).4 The obsessing subscale of the C-OCI-R had the highest correlation with the Y-BOCS obsession subscale. Correlation was likely attenuated as the focus of the two instruments differs: the C-OCI-R measures the distress associated with specific OCD complaints, whereas the Y-BOCS measures severity of five different parameters (time, interference, distress, resistance, and control).28 In addition, method variance may be another reason, as the C-OCI-R is a self-report measure whereas the Y-BOCS is a semi-structured interview. However, a study reported the same range of moderate correlation between the OCI-R and the Y-BOCS-SR (a self-report version of the Y-BOCS), suggesting the inherent method variance is less important than differences in the contents covered by the two measures.25
Convergent validity was supported by the high correlation (r = 0.85) between the original OCI-R and the Maudsley Obsessive-Compulsive Inventory, which is a self-report measure.4,36 However, so far none of the self- report measures of OCD symptoms has been translated and validated in Hong Kong, and hence no comparison can be made between the C-OCI-R and other self-report measure of OCD severity.
Divergent validity was demonstrated by the low correlation of the C-OCI-R score with the BDI-II score (r = 0.49) and the HDRS score (r = 0.39). The correlation of the C-OCI-R with the Y-BOCS was clearly higher than that of the C-OCI-R with the BDI-II and the HDRS. However, the correlation of the original OCI-R with the BDI (r = 0.70) and the HDRS (r = 0.58) were higher. The higher correlations between OCD and depression may reflect the high levels of depression observed in OCD patients.4
Subsequent studies in clinical and non-clinical samples reported a lower correlation in divergent validity with the BDI (r = 0.39-0.41).28,37 The weak divergent validity with depression measures is a substantial shortcoming of all OCD measures.28,38 Overall, our findings support the divergent validity of the C-OCI-R score.
The divergent validity of the obsessing subscale of the C-OCI-R was unsatisfactory, consistent with previous studies,25,30,37 indicating that there is an overlap between obsession and depression. The correlations of the obsessing subscale of the C-OCI-R with the BDI-II (r = 0.53) and the HDRS (r = 0.53) were similar to the correlation between the obsessing subscale of the C-OCI-R and the Y-BOCS (r = 0.46). Depressive symptoms have a stronger association with obsessional than compulsive symptoms,39 which could explain the significant correlation between the obsessing subscale and depressive measures in the present study.
This study has some limitations. Patients were sampled from a single psychiatric centre. Although OCD patients with current comorbid depressive disorders were not excluded, the number of such patients turned out to be lower than expected (n = 17). Given the high comorbidity rate of OCD with depressive disorders, the present sample might not be representative of all OCD patients, thereby limiting the generalisability of our results.40 In addition, the present study is a cross-sectional study, some psychometric properties such as sensitivity to change and predictive validity of the C-OCI-R were not explored. Future studies should include a larger and more representative sample and patients with OCD as a secondary diagnosis to improve the generalisability of the results. A longitudinal study can explore the sensitivity to change and predictive validity of the C-OCI-R. In addition, future research should focus on the validation of the neutralising subscale to determine if further refinement is needed. Finally, further studies should include other non-clinical participants aiming at evaluating the psychometric properties of the C-OCI-R as a screening tool.
Conclusion
The C-OCI-R is a brief, reliable, and valid measure for assessing severity of a broad range of OCD symptoms in both clinical and research settings. Validation of the C-OCI-R may facilitate future studies of OCD in Hong Kong.
Acknowledgement
The authors would like to thank Ms Eunice Tang and Mr Edward Choi for their help in the translation and validation process, and all participants for their support.
Declaration
The authors have no conflict of interest to disclose.
References
- Ruscio AM, Stein DJ, Chiu WT, Kessler RC. The epidemiology of obsessive-compulsive disorder in the National Comorbidity Survey Replication. Mol Psychiatry 2010;15:53-63. Crossref
- Chen CN, Wong J, Lee N, Chan-Ho MW, Lau JT, Fung M. The Shatin community mental health survey in Hong Kong. II. Major findings. Arch Gen Psychiatry 1993;50:125-33. Crossref
- Overduin MK, Furnham A. Assessing obsessive-compulsive disorder (OCD): a review of self-report measures. J Obsessive Compuls Relat Disord 2012;1:312-24. Crossref
- Foa EB, Huppert JD, Leiberg S, Langner R, Kichic R, Hajcak G, et al. The Obsessive-Compulsive Inventory: development and validation of a short version. Psychol Assess 2002;14:485-96. Crossref
- Huppert JD, Walther MR, Hajcak G, Yadin E, Foa EB, Simpson HB, et al. The OCI-R: validation of the subscales in a clinical sample. J Anxiety Disord 2007;21:394-406. Crossref
- Abramowitz JS, Tolin DF, Diefenbach GJ. Measuring change in OCD: sensitivity of the Obsessive-Compulsive Inventory-Revised. J Psychopathol Behav Assess 2005;27:317-24. Crossref
- Peng ZW, Yang WH, Miao GD, Jing J, Chan RC. The Chinese version of the Obsessive-Compulsive Inventory-Revised scale: replication and extension to non-clinical and clinical individuals with OCD symptoms. BMC Psychiatry 2011;11:129. Crossref
- Chasson GS, Tang S, Gray B, Sun H, Wang J. Further validation of a Chinese version of the Obsessive-Compulsive Inventory-Revised. Behav Cogn Psychother 2013;41:249-54. Crossref
- Census and Statistics Department, The Government of the Hong Kong Special Administrative Region. The Profile of Hong Kong Population Analysed by District Council District; 2012.
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 4th ed. Washington, DC; 2000.
- 1 Beaton DE, Bombardier C, Guillemin F, Ferraz MB. Guidelines for the process of cross-cultural adaptation of self-report measures. Spine (Phila Pa 1976) 2000;25:3186-91. Crossref
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Research Version, Patient Edition. (SCID-I/P) New York: Biometrics Research, New York State Psychiatric Institute; 2002.
- Goodman WK, Price LH, Rasmussen SA, Mazure C, Delgado P, Heninger GR, et al. The Yale-Brown Obsessive Compulsive Scale. II. Validity. Arch Gen Psychiatry 1989;46:1012-6. Crossref
- Goodman WK, Price LH, Rasmussen SA, Mazure C, Fleischmann RL, Hill CL, et al. The Yale-Brown Obsessive Compulsive Scale. I. Development, use, and reliability. Arch Gen Psychiatry 1989;46:1006-11 Crossref
- Beck AT, Steer RA, Brown GK. BDI-II, Beck depression inventory: manual. San Antonio, Boston: Psychological Corp; Harcourt Brace; Crossref
- Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry 1960;23:56-62. Crossref
- So E, Kam I, Lam L. The Chinese Bilingual SCID-I/P Project: stage 3 - multi-site inter-rater reliability. Hong Kong J Psychiatry 2004;14:19- 25.
- So E, Kam I, Leung CM, Chung D, Liu Z, Fong S. The Chinese- bilingual SCID-I/P Project: stage 1 - reliability for mood disorders and schizophrenia. Hong Kong J Psychiatry 2003;13:7-18.
- So E, Kam I, Leung CM, Pang A, Lam L. The Chinese-bilingual SCID-I/P Project: stage 2 - reliability for anxiety disorders, adjustment disorders, and `no diagnosis’. Hong Kong J Psychiatry 2003;13:19-25.
- Storch EA, Rasmussen SA, Price LH, Larson MJ, Murphy TK, Goodman WK. Development and psychometric evaluation of the Yale- Brown Obsessive-Compulsive Scale--second edition. Psychol Assess 2010;22:223-32. Crossref
- Taylor S. Assessment of obsessions and compulsions: reliability, validity, and sensitivity to treatment effects. Clin Psychol Rev 1995;15:261-96. Crossref
- Lu ML, Che HH, Chang SW, Shen WT. Reliability and validation of Chinese version of the Beck Depression Inventory-II. Formos J Med 2002;16:301-10.
- Zheng YP, Zhao JP, Phillips M, Liu JB, Cai MF, Sun SQ, et al. Validity and reliability of the Chinese Hamilton Depression Rating Scale. Br J Psychiatry 1988;152:660-4. Crossref
- Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Equ Modeling 1999;6:1-55. Crossref
- Gönner S, Leonhart R, Ecker W. The Obsessive-Compulsive Inventory-Revised (OCI-R): validation of the German version in a sample of patients with OCD, anxiety disorders, and depressive disorders. J Anxiety Disord 2008;22:734-49. Crossref
- Schermelleh-Engel K, Moosbrugger H. Evaluating the fit of structural equation models: tests of significance and descriptive goodness-of-fit measures. Methods Psychol Res Online 2003;8:23-74.
- Ecker W, Gönner S. The feeling of incompleteness. Rediscovery of an old psychopathological symptom of obsessive-compulsive disorder [in German]. Nervenarzt 2006;77:1115-20,22.
- Abramowitz JS, Deacon BJ. Psychometric properties and construct validity of the Obsessive-Compulsive Inventory--Revised: replication and extension with a clinical sample. J Anxiety Disord 2006;20:1016-35Crossref
- Sica C, Ghisi M, Altoe G, Chiri LR, Franceschini S, Coradeschi D, et al. The Italian version of the obsessive compulsive inventory: its psychometric properties on community and clinical samples. J Anxiety Disord 2009;23:204-11. Crossref
- Woo CW, Kwon SM, Lim YJ, Shin MS. The Obsessive-Compulsive Inventory-Revised (OCI-R): psychometric properties of the Korean version and the order, gender, and cultural effects. J Behav Ther Exp Psychiatry 2010;41:220-7. Crossref
- Steketee G, Frost R. Compulsive hoarding: current status of the research. Clin Psychol Rev 2003;23:905-27. Crossref
- Grisham JR, Brown TA, Liverant GI, Campbell-Sills L. The distinctiveness of compulsive hoarding from obsessive-compulsive disorder. J Anxiety Disord 2005;19:767-79. Crossref
- Timpano KR, Exner C, Glaesmer H, Rief W, Keshaviah A, Brahler E, et al. The epidemiology of the proposed DSM-5 hoarding disorder: exploration of the acquisition specifier, associated features, and distress. J Clin Psychiatry 2011;72:780-6. Crossref
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed. Washington, DC; 2013. Crossref
- Stein DJ, Kogan CS, Atmaca M, Fineberg NA, Fontenelle LF, Grant JE, et al. The classification of obsessive-compulsive and related disorders in the ICD-11. J Affect Disord 2016;190:663-74. Crossref
- Hodgson RJ, Rachman S. Obsessional-compulsive complaints. Behav Res Ther 1977;15:389-95. Crossref
- Hajcak G, Huppert JD, Simons RF, Foa EB. Psychometric properties of the OCI-R in a college sample. Behav Res Ther 2004;42:115-23. Crossref
- Swinson RP. Obsessive-Compulsive Disorder: Theory, Research, and Treatment. New York: Guilford Press; 1998.
- Ricciardi JN, McNally RJ. Depressed mood is related to obsessions, but not to compulsions, in obsessive-compulsive disorder. J Anxiety Disord 1995;9:249-56. Crossref
- Abramowitz JS. Treatment of obsessive-compulsive disorder in patients who have comorbid major depression. J Clin Psychol 2004;60:1133-41. Crossref